Summary
Objectives
Effective and efficient communication is crucial in healthcare. Written communication remains the most prevalent form of communication between specialised and primary care. We aimed at reviewing the literature on the quality of written communication, the impact of communication inefficiencies and recommendations to improve written communication in healthcare.
Design
Narrative literature review.
Methods
A search was carried out on the databases PubMed, Web of Science and The Cochrane Library by means of the (MeSH)terms ‘communication’, ‘primary health care’, ‘correspondence’, ‘patient safety’, ‘patient handoff’ and ‘continuity of patient care’. Reviewers screened 4609 records and 462 full texts were checked according following inclusion criteria: (1) publication between January 1985 and March 2014, (2) availability as full text in English, (3) categorisation as original research, reviews, meta‐analyses or letters to the editor.
Results
A total of 69 articles were included in this review. It was found that poor communication can lead to various negative outcomes: discontinuity of care, compromise of patient safety, patient dissatisfaction and inefficient use of valuable resources, both in unnecessary investigations and physician worktime as well as economic consequences.
Conclusion
There is room for improvement of both content and timeliness of written communication. The delineation of ownership of the communication process should be clear. Peer review, process indicators and follow‐up tools are required to measure the impact of quality improvement initiatives. Communication between caregivers should feature more prominently in graduate and postgraduate training, to become engraved as an essential skill and quality characteristic of each caregiver.
Review criteria
A search was carried out on the different databases by means of the (MeSH)terms ‘communication’, ‘primary health care’, ‘correspondence’, ‘patient safety’, ‘patient handoff’ and ‘continuity of patient care’. Reviewers screened 4609 records and 462 full texts were checked according following inclusion criteria: (1) publication between January 1985 and March 2014, (2) availability as full text in English, (3) categorisation as original research, reviews, meta‐analyses or letters to the editor.
Message for the clinic
There is room for improvement of both content and timeliness of written communication. The delineation of ownership of the communication process should be clear. Peer review, process indicators and follow‐up tools are required to measure the impact of quality improvement initiatives. Communication between caregivers should feature more prominently in graduate and postgraduate training, to become engraved as an essential skill and quality characteristic of each caregiver.
Introduction
In the evolution of medicine, an increasing number of patients, in particular with chronic disease or illness, is requiring treatment by healthcare providers from different disciplines 1. Two major trends emerge. First, diagnostic workups and treatments are increasingly organised on an outpatient basis, and, second, especially treatment and care is shifting towards primary care. Both trends increase the need for sharing information between specialists and general practitioners (GPs) to ensure continuity of care, in an integrated transmural model 2, 3, 4, 5. The practice and delivery of healthcare is argued to be fundamentally and critically dependent on effective and efficient communication 6. This is especially true for countries such as the UK, Denmark and the Netherlands, where GPs act as obligatory gatekeepers and the communication towards and from secondary care determines the smooth running of the healthcare system 7. However, countries or healthcare systems without this obligatory gatekeeper function may be at higher risk for suboptimal communication between levels of care.
The aim of the present paper is to review the existing literature on quality, efficacy and impact of written communication in healthcare as well as of recommendations for improvement.
Methods
The databases PubMed, Web of Science and The Cochrane Library were searched using the (MeSH)terms ‘communication’, ‘primary health care’, ‘correspondence’, ‘patient safety’, ‘patient handoff’ and ‘continuity of patient care’. The MeSH terms were internally validated by the coauthors. Articles in this review needed to be (1) published prior to March 2014 and after January 1985, (2) available as full text in English, (3) categorised as original research, reviews, meta‐analyses or letters to the editor. Database screening was closed 31 March 2014. Titles and abstracts were reviewed to verify these criteria. If all inclusion requirements were present or if this remained unclear, the articles were fully read. In case the full text revealed that not all requirements were present, the paper was excluded. Additional literature was obtained through searching references in the manuscripts (snowball method).
A framework with four categories was predefined: modalities of communication, deficits in communication, economic impact of communication inefficiencies and recommendations. An individual paper could be categorised into different fields. The review was further elaborated by addressing each category separately and rereading all articles that were relevant for that category.
Results
The results of the search process are summarised in Figure 1. Out of a total of 5013 papers selected, 404 duplicates were removed. 4609 records were screened and 462 remained for full text screening. Finally, 69 articles were included in the review. The aim, setting, sample description, design, coverage of categories addressed within the review and main findings of these individual studies are summarised in the online supplement.
Figure 1.
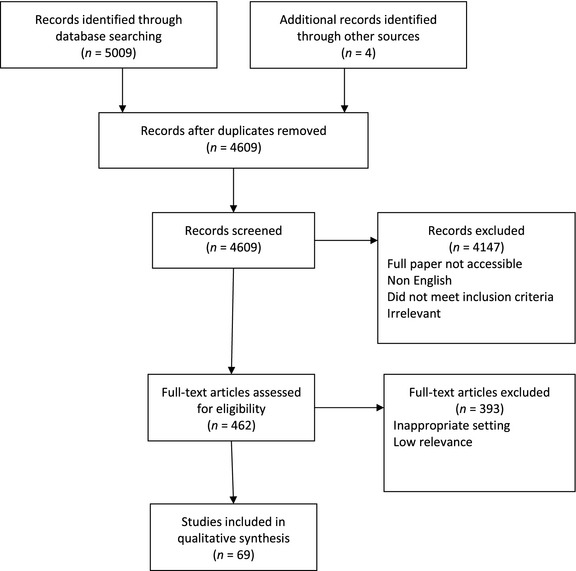
Review stages based on PRISMA flow diagram 8
Modalities of communication
Although a review of the literature revealed that face‐to‐face communication is recommended, in practice, written communication remains the most usual means of communication between healthcare professionals. Furthermore, there is a consensus about particular advantages of written communication over face‐to‐face communication.
Face‐to‐face communication is essential to get the full conversation. In face‐to‐face communication, all involved parties can not only hear what is being said but also they can see the body language and facial expressions that provide key information so they can better understand the meaning behind the words. In the past, this type of communication was only possible in person, but as technology advances there are more ways to have these face‐to‐face conversations 9. Video conferencing is also a form of face‐to‐face communication, even though it uses technology to connect the participants. These forms of direct communication may in fact have decreased in the electronic communication age, favoring indirect rather than direct communication 10. Rapidly delivered e‐mail letters with a read confirmation may represent a good proxy to telephone or face‐to‐face contacts and have the advantage of traceability and consultation by third parties.
Written communication in the larger interpretation remains the most usual, and sometimes the only, means of communication between healthcare professionals 3. The most frequently used forms of written communication are referral and discharge letters. Referral letters can be subdivided into three types: i.e. requests for a specific assessment or treatment, request for a second opinion and requests for mutual responsibility for the care of a patient 11. Discharge letters on the other hand generally refer to patients discharged from hospital. However, the term is also used for other settings such as answer letters after a specialist outpatient visit without hospitalisation. This in itself poses a problem of semantics and definitions, as the terminology of discharge letters seems not to have followed the shift towards mainly outpatient care.
Written communication certainly has its advantages. For instance, it can be used for future reference purposes and it can be easily and simultaneously distributed to the required number of caregivers involved in the care process 12. They are not only a means of communication but can also serve as a medico‐legal value 13. Moreover, in the current electronic environment, written communication has evolved towards a more immediate medium and may therefore be preferred 14.
Letters also have an educational goal. They can provide extra information that can increase the understanding of the problem, its implications, the problems, and options in management or the prognosis expected 15. Specialists ‘teach’ more in their letters than GPs 7 and it was found that one quarter of the specialists’ letters had an educational value, as compared to 3% of GPs’ letters 15.
Inefficiencies in written communication
There is a large body of literature on inefficiencies in written communication. Cross‐sectional studies, performed in different countries and settings, show a unequivocal concordance in both perceptions of the ideal content of written communication and its current inefficiencies. Reviews align with these findings. This overall agreement enables drawing conclusions for clinical practice. In this section, on the one hand reports on subjective views of GPs and specialists setting out what they think letters should contain, and on the other hand reports with empirical data on the analysis of the content of actual letters are included 16.
Mutual perceptions in the trialogue between patient, physician and society
General practitioners and specialists disagree about the quality of their mutual communication. Specialists mention GPs’ referral letters to lack information. Furthermore, they feel that GPs insufficiently follow their specialist advice. GPs in turn mention that many of their questions are insufficiently addressed by the specialists. The latter does not correspond with specialist opinion in a cross‐sectional study among a random sample of 550 GPs and 533 specialists selected from the Netherlands Medical Address Book 17 (Table 1). This study showed that GPs telephone accessibility is qualified as poor by specialists (32.8% agrees with ‘GP can be easily reached’), while GPs consider their telephone accessibility as good (85.3% agrees). Specialists think poorly of the GPs’ referral letter, as only 29.1% of specialists rate these letters as of good quality. Merely half of GPs feels their questions are addressed appropriately by the specialist, whereas specialists feel this number to be considerably higher. According to specialists, GPs often do not follow the advice given. GPs rate their compliance much higher. Less than a quarter of GPs feel specialist letters arrive on time, whereas specialists have a different perception. Both parties wish to receive feedback from each other, while in practice they hardly do so 17. Overall, less GPs’ letters are judged as being of excellent quality than specialists’ letters (39.5% vs. 78.6%) 7. GP letters were found to have inaccurate medication lists (drugs or doses) in 42% of the cases 18. In a study from a single general hospital in Norway assessing referral and discharge letters, the Delphi technique was used by two expert panels (each with one general hospital specialist, one GP and one public health nurse) using a standardised evaluation protocol with a visual analogue scale 19. The panels assessed the quality of the description of the patient's actual medical condition, former medical history, clinical signs, medication, activity of daily living (ADL), social network, need of home care and the benefit of general hospital care. This analysis revealed low consensus between health professionals at primary and secondary level and low quality of a majority of referral letters, considered as a health hazard. Overall, 20% of the discharge letters was missing vital medical information and less than half of the letters contained high‐quality information on ADL, social network or need for home care. However, it seems that some specialists (11%) and GPs (28%), are also dissatisfied about their own letters mainly because of time constraints impacting on quality 10.
Table 1.
GPs’ and specialists’ perceptions on aspects of communication 17
| GPs agree | Specialists agree (%) | p‐value | |
|---|---|---|---|
| GPs telephone accessibility is good | 85.3 | 32.8 | < 0.001 |
| Referral letter of GP is of good quality | – | 29.1 | |
| Questions are addressed by the specialist | 50.0 | 87.5 | < 0.001 |
| GPs follow the advice given by the specialist | 92.2 | 49.5 | < 0.001 |
| Specialist letter is sent back in a timely manner | 22.5 | 61.8 | < 0.001 |
Expectations on the modalities and content issues of communication may differ according to phases in particular diseases. This is indicated in an assessment on communication issues across the primary/secondary interface in ovarian cancer 20. GPs and specialists also have different expectations on the content of cancer patients’ discharge letters, especially on psychosocial items 21.
In the modern relational personalistic ethical perspective, the patient viewpoint and experience of the collaboration between GP and specialists is at least as important as the perception of the healthcare professionals. To this purpose, a consumer quality index continuum of care has been validated for assessing patient's experiences across the interface between primary and secondary care. This instrument consists of statements on GP approach, GP referral, specialist communication and collaboration between GP and specialists and was shown to be a useful instrument to assess aspects of the collaboration between GPs and specialists from patients’ perspective 1.
Relevance of communication items
Referral letters from GPs to specialists
More than 20 years ago, Newton et al. questioned GPs and specialists on which items they considered important, revealing a high degree of consensus 16. They also reported what the GP expects from the referral. These expectations are also described in Tattersall et al. 22, who, in contrast, found large differences between GPs and specialists concerning the information their letters should contain. A number of items are summarised in Table 2.
Table 2.
Content of referral letters
| Content of referral letters and information that specialists want in referral letters | Letters from specialists and information that referring doctors want in reply letters | ||
|---|---|---|---|
| Newton et al. (1992) | Tattersall et al. (2002) | Newton et al. (1992) | Tattersall et al. (2002) |
| Clinical content of general practitioner's letter: | Items of information: | Clinical content of consultant's reply: | Items of information: |
Medical information
|
Medical information
|
Medical information
|
Medical information
|
Patient/Family involvement
|
Patient/Family involvement
|
Patient/Family involvement
|
Patient/Family involvement
|
Clinician expectations
|
Clinician expectations
|
Clinician expectations
|
Clinician expectations
|
Administrative content of general practitioner's letter:
|
|||
Hartveit et al. aimed at identifying the recommended content of referral letters from GPs to specialised mental healthcare by means of discussion groups. Seven headings were proposed: personal and contact information, introductory information (e.g. is the patient suicidal?), case history and social situation, present state and results, past and ongoing treatment and the professional network involved, the patient's assessment, the reason for referral. More specifically, as compared with other referral letters, in mental healthcare a stronger emphasis on the planned integrated care, the specialist's role and on the patient's involvement is recommended 23.
Jiwa et al. analysed 350 referral letters for upper gastro‐intestinal investigation from GPs and found that only few upper gastro‐intestinal symptoms were included 24. Furthermore, GP referral letters do not always include a specific question and when a question is formulated, it is not always addressed. This disables a real information exchange 25. McConnell et al. performed an information audit of referral and reply letters in cancer care. Oncologists wanted to have more information about the patient's medical status, the involvement of other doctors and any special considerations. GPs preferred more information about the treatment plan, future management and expectations and psychosocial concerns. Referral letters about older patients were of low quality and only the actual medical situation was well described. Discharge letters did often not describe the functioning of the patient and the need for home care services, neither who was responsible for follow‐up 19.
Answer letters, including discharge letters after hospitalisation
A review by Kripalani et al. addressed which information GPs rate as most important in a discharge letter to provide adequate follow‐up: main diagnosis (lacks in 13–17.5%), physical findings (10.5–45.5%), results of investigations (38–65%), test results pending at discharge (65–88%), discharge medication (21–25%) and the reason for any changes to previous medication, details of follow‐up arrangements (14–30%), information given to the patient and family (91–92%) 2. The latter was also identified in an earlier study, in which was found that specialists only sporadically (< 20%) include such social information 26. Wrong diagnoses have also been found, as well as discrepancies between the discharge summary and the take‐home prescription (39%) 27. Tattersall et al. compared the content of letters to the patients and letters to the referring physician. The latter were not well tailored to the referring physicians’ needs and lacked information on recommended future tests, treatment options, side effects and prognosis 28.
Durbin et al. summarised fifteen audit studies on discharge or referral/consultation letters in mental healthcare 29. The items were grouped into four domains: administrative details, patient details, clinical details and discharge/referral details. In discharge letters, clinical history, physical findings, test results and follow‐up details were less reported. For referral letters, results were poorer: reason for referral was present in only 74% of the cases, 25% did not contain present complaints, urgency and risk information were rarely reported, only 26% reported about the information given to the patient and clinical information and diagnosis were unsatisfactory in many cases 29.
The readability level of letters was another issue raised. Letters of specialists would be too detailed and not enough structured (e.g. lacking headings, long paragraphs) 30, 31.
Reasons for the poor content of written communication are also multifactorial: a lack of time to create notes 10, GPs maybe do not make a full assessment of the problems 24, GPs and specialists may use a different point of view 19, they may consider letters to have different goals (e.g. a tool for information transfer vs. archiving) 17, etc.
Timeliness
A considerable number of studies assessed timeliness of communication, either the subjective perception or real delays. It is clear that timeliness is a significant contributor to communication efficiency for all stakeholders.
Besides the unsatisfactory content of written communication, timeliness is another frequently reported problem. Tardivity of specialists’ letters has been identified as a major complaint of GPs 20, 32. Less than one quarter thinks the specialists’ letters are delivered in time (as compared to 61.8% of the specialists) 17. One week after discharge, 53% of the discharge letters reached the GP and approximately 11% never reached the GP 33. Hence, patients often contact or see their GP before he has received the letter (16–53%), which means that patients are then the first to inform the GP about their hospitalisation 2. This delay can have multiple causes and occurs at different stages of the reporting process: the specialist can wait too long to draw up the letter (whether dictated or extracted form an electronic patient record); the administrative workup (e.g. typing the letter) and verification (finalised by signature) can add significantly to the final delay 20. This could explain the perceptions of GPs and specialists about timeliness. For example, specialists report to answer GPs within 7 days, whereas GPs report receiving an answer within 7 days only in 36% of the cases 10. Moreover, 4 weeks after the referral visit, 25% of the GPs had still not received an answer from the specialist 10.
Inefficient communication has several potentially negative consequences, for all involved in the healthcare process. Continuity of care, the connection of separate and discrete elements of care into a longitudinal process, suffers from inadequate communication. This applies especially to informational continuity, the reporting of adaptations in the chronic care process and their integration within a history of antecedents 34. It is evident that information on prior events can influence current decisions on the patient's care and that the lack or incompleteness of such information can lead to (potentially) preventable adverse events and subsequent patient harm. As well, poor communication often causes several types of delays, such as in consultation response or acceptance of a referral, in diagnoses and treatment 29, 35. As a consequence, patient safety may be compromised when the right information is not available to the right person at the right time (e.g. translating into inconsistent treatment plans and inadequate follow‐up, medication errors and increasing polypharmacy) 29, 35, 36.
For healthcare providers, poor communication leads to additional workload as it decreases confidence in decisions 29, 37. Last, patients can be confronted with having to repeat their stories, double tests, treatment delays and can receive conflicting information 29, which, in turn, may lead to decreased patient confidence and satisfaction 35, 38. Several of these mechanisms additionally imply increased, unnecessary and avoidable costs, e.g. because of unnecessary repeat investigations 35.
Economic impact of communication inefficiencies
Although healthcare providers spend a significant amount of their time in communication, studies trying to quantify the economic impact of communication efficiencies are very scarce 6. This lack in the literature is even more surprising when keeping in mind that communication influences patient safety 39.
Literature provides numerous examples of outcomes of poor communication with an economic impact. First, it leads to avoidable hospital admissions 19 and readmissions 40, 41. Interventions to improve communication and coordination have been found to reduce hospital admissions 42. Other avoidable healthcare expenditures can be seen in unnecessary testing, polypharmacy inappropriate referrals and repeated referrals for problems which were not adequately addressed during the first visit 10, 35, 43. But, and this comes on top of the economic impact, patient safety suffers from poor communication 36. Residents considered communication difficulties as being the cause of the vast majority of medical mishaps 39. Indeed, as 10% of the test results after discharge require action from the GP, but if these do not reach the GP (in time), there may be propensity to medical error 44. The most striking results come from Australia. The study found that communication problems were responsible for 11%, inadequate skill levels of practitioners for 6% and inadequate resources for 4% of the adverse outcomes respectively 45.
In cancer care, three types of costs because of poor communication have been defined: the cost of psychological distress, the cost of unnecessary treatment and the cost of indirect system distress (e.g. distress by healthcare providers) 46.
Agarwal et al. propose a conceptual model of communication outcomes, shown in Figure 2.
Figure 2.
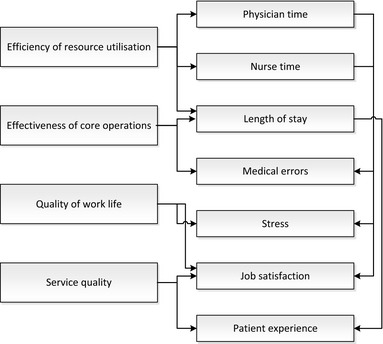
Conceptual model of communication outcomes in a hospital 6
Hospital resources that should be efficiently used include physician and nurse time. A time–motion study reported that communication accounts for 24% of the work time of specialists 47. Communication inefficiencies in the hospital setting for physicians are estimated to generate a waste of $800 million annually. Hendrich et al. reported a breakdown of nurse activities, in which approximately 20.6% of each nursing shift was classified as ‘care coordination’ (i.e. communication with team members or other departments) and 6.6% as ‘wasted time’ 48. The economic impact of communication inefficiencies in nursing practices is estimated at about $4.9 billion per year. As a third factor influencing resource utilisation, wasted costs because of poor communication leading hospital overstay, were estimated to be $6.6 billion annually. The effectiveness of core operations is represented by the swiftness and safety of diagnostic and treatment processes, as ineffectiveness and errors will increase complication rates and lengths of stay. To this purpose, pathology adjusted length of stay and medication error rates are measurable process indicators. Quality of work life is also affected by communication, as reflected in stress and job satisfaction measures. Fourth, since healthcare is a service business, hospitals are service organisations and should provide service quality. Poor communication (e.g. patients not being timely informed about test results, delays in patient discharge, lack of information availability for the family of the patient…) affect patient experience.
In this model, tangible as well as less tangible outcomes are combined. Tangible outcomes, such as length of stay and wasted physician and nurse time, can be easily translated into monetary terms. Less tangible outcomes on the other hand, such as job satisfaction, have an economic impact through other processes. Job dissatisfaction leads to staff turnover as it represents an incentive to healthcare professionals for career moves. Therefore, increased costs are incurred for recruiting and training new employees with a learning curve, translating into less effectivity. Negative patient experiences with communication and service levels 49 will predispose to future choices for different hospitals and care organisations, turning away potential clients. Along the same line, referring physicians may switch specialists and hospitals because of poor communication 49. These trends are likely to be reinforced by the increasing demand for transparency regarding effectivity in specific diseases and the use of social media.
In spite of this conceptualisation, reported data on economic impact remain derived from and based on assumptions. In the USA, hospitals waste over $12.4 billion per year because of communication inefficiencies. More than half of that amount (53%) is because of an increase in length of stay, 40% is because of wasted nurse time and 6.7% because of wasted physician time. For a 500‐bed hospital, annual losses because of communication inefficiencies are estimated to be $4 million 6.
Recommendations to improve written communication
Structured letters
A well‐supported recommendation is the use of structured referral and reply/discharge letters. Reply letters could, for example, contain a problem list, a management list and free text below. Structured letters take no longer to read and improve comprehension 50. Using a template leads to higher quality and reduced length of discharge letters 51. Structured letters are preferred by GPs, but only few specialists write structured letters 52. GPs can partly influence this by putting specific requests in their referral letter, which could then be repeated in the reply letter, followed by specific answers 25.
This strategy can be facilitated by the use of health information technology, such as electronic patient records 53. However, this method can still become more standardised and possibly also user‐friendly by the use of structured instead of free text fields 54. Effective health information technology could produce automatically structured computer‐generated letters 30. These letters are preferred by GPs because of higher scores on clarity and content 55.
However, standardisation and user‐friendliness often can be improved by the use of structured instead of free text fields.
There are nonetheless some pitfalls associated with structured letters. A referral template was developed by the Irish Health Information and Quality Authority and the Irish College of GPs, but was found to be rarely used by specialists 56. They can result in extra workload for the physician because of long forms (to write and to read) 29. The inclusion of a tick box for urgent referrals should also be well considered: there is a risk for overuse 57 and patients are not seen earlier 15.
Curriculum – feedback
Another strategy is the use of different forms of feedback. First of all, specialists can provide feedback on the referral letters. This improves the quality of referral letters and can make referrals more focused 58. Of course, GPs can also provide feedback to specialists. Peer assessment is able to significantly improve the quality of the written communication between both parties 22, 59. To facilitate feedback or peer assessment, specific tools could be used 3.
Feedback can also be introduced earlier, namely in the curriculum of medical students. Up till now, written communication is rarely addressed in communication courses 60. Training sessions have showed to raise knowledge about written communication in healthcare, but should not be restricted to ‘knowing’ and ‘knowing how’ but should equally focus on ‘doing’ 60. Improvement strategies outlined above (feedback, peer assessment, tool) could also be used during written communication courses.
Changing processes
A clear written communication between specialists and GPs is of great importance. But as Durbin et al. notice ‘changing clinical practice is difficult’ and therefore, multifaceted and broad interventions may be more effective than interventions with a very specific impact. In their review of audit studies in mental healthcare, a combination of guidelines, training and a structured form is proposed 29. The use of computer‐generated letters could also be considered a change to the earlier process of dictated letters. This results in a higher percentage of discharge summaries completed at 4 weeks and moreover, reduces the amount of omitted, essential items 61, 62, 63, 64. For GPs too, computerised referral systems could reduce their administrative work and could probably give the benefit to more timely communication 10.
Such tools could also contain a pharmaceutical decision‐support system which could reduce mistakes in medication lists 18. For dictated letters, a seemingly self‐evident recommendation is to always read and sign them when they are ready, to avoid unintentional mistakes 65.
A suggestion to partly solve the timeliness problem is to give the letter to the patient (or give him a copy). As such, letters could sometimes sooner reach the addressee 2, 61, 66. Discharge letters could for example be combined with a prescription form for take‐home medication 67. Another possibility is to share medical notes with patients, which allows patients to review the notes (project ‘Open Notes’) 68. This change should, however, not be implemented without any restriction because it may lead to specialists omitting information in the letter in order not to distress the patient 69.
With the availability of different communication channels, these could be combined using respective advantages, such as direct telephone calls for urgent and essential communications, conferences for on line multidisciplinary assessments, involving GPs, backed up with formal written or electronic letters. The latter may serve as validation and referral documents of the former. Electronic communication often needs, in the absence of the direct telephone communication, an alert system, guaranteeing reception and rendering appropriate action by the receiver more likely. Improving interaction will lead to better results, such as better patient outcomes, better gatekeeping and standardisation of work processes, as evidenced in the meta‐analysis by Foy et al. 70.
A qualitative study in GPs confirms the above‐mentioned strategies: greater use of telephone, secretarial support, templates and delivery of the letters by the patient. In addition, nurse‐led communications were proposed. They are also willing to reconsider electronic patient records so that GPs, or even patients, could also have access to it 20.
In contrast to other fields in medicine (such as in the treatment and prevention of blood stream infections 71 and other nosocomial infections, such as sepsis (Surviving Sepsis Campaign), there is no literature documenting the impact of a bundle approach assessing the specific impact of a selected number of interventions with process and/or outcome indicators. It is clear that communication in any healthcare setting may be the subject of such a bundle approach that would define priorities in an improvement programme and render such an improvement initiative feasible in the field, against a jungle of recommendations.
Strengths and limitations of this review
This is a comprehensive review of the literature on written communication in healthcare, providing a multidimensional overview of this important topic. During the search for this review has screened a vast amount of the literature (over 4500 articles) across a number of databases. Clear and concrete ideas for improvement were proposed and explained.
Conclusion
In recent years, in many countries healthcare is experiencing a shift towards primary care, particularly driven by the growing number of chronically ill patients. At the same time, healthcare becomes more and more specialised and as such, communication between specialised and primary care is of paramount importance.
Poor communication can indeed lead to various negative outcomes: discontinuity of care, compromise of patient safety, inefficient use of valuable resources, dissatisfaction in patients and overworked physicians and economic consequences, often hidden. As written communication is still the most used form of communication between specialised and primary care, this review can be a guidance for improvements in this field.
There is a clear need for a structured approach, addressing both content (ensuring the required items, addressal of referral questions, diagnosis and management issues) and timeliness. This structured approach also includes clear delineation of ownership of the communication process. Peer review is needed to assess quality indicators in this respect in each particular care process component. Process indicators and follow‐up tools are required to measure the impact of quality improvement initiatives, according to the SMART (specific, measurable, achievable, realistic, time related) principle 72. Finally, communication between caregivers and the importance as well as quality, should feature more prominently in both graduate and postgraduate training, to become engraved as an essential skill and quality characteristic of each caregiver.
Funding
None.
Author contributions
All coauthors contributed to the study design and reviewed drafts of the manuscript. The first author screened all the articles for inclusion in this review and appraised the study quality. Sophie Degroote screened a sample of these at title/abstract and full text. Dominique Vandijck scored the quality of a sample of the included articles. Peter Vermeir, Sophie Degroote, Dominique Vandijck and Dirk Vogelaers drafted the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
The authors thank Ms. Marie Blankaert for providing administrative support.
Disclosures
There are no potential conflicts of interest to be reported.
References
- 1. Berendsen AJ, Groenier KH, de Jong GM et al. Assessment of patient's experiences across the interface between primary and secondary care: Consumer Quality Index Continuum of care. Patient Educ Couns 2009; 77: 123–7. [DOI] [PubMed] [Google Scholar]
- 2. Kripalani S, LeFevre F, Phillips CO et al. Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007; 297: 831–41. [DOI] [PubMed] [Google Scholar]
- 3. Francois J. Tool to assess the quality of consultation and referral request letters in family medicine. Can Fam Phys 2011; 57: 574–5. [PMC free article] [PubMed] [Google Scholar]
- 4. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005; 83: 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moosbrugger MC. Unclogging the physician referral network. Winning referrals requires research and tracking. Healthc Exec 1988; 3: 28–9. [PubMed] [Google Scholar]
- 6. Agarwal R, Sands DZ, Schneider JD. Quantifying the economic impact of communication inefficiencies in U.S. hospitals. J Healthc Manag 2010; 55: 265–81; discussion 81‐2. [PubMed] [Google Scholar]
- 7. Westerman RF, Hull FM, Bezemer PD, Gort G. A study of communication between general practitioners and specialists. Brit J Gen Pract 1990; 40: 445–9. [PMC free article] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–9 W64. [DOI] [PubMed] [Google Scholar]
- 9. Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs. Acad Med 2005; 80: 1094–9. [DOI] [PubMed] [Google Scholar]
- 10. Gandhi TK, Sittig DF, Franklin M et al. Communication breakdown in the outpatient referral process. J Gen Intern Med 2000; 15: 626–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thorsen O, Hartveit M, Baerheim A. General practitioners’ reflections on referring: an asymmetric or non‐dialogical process? Scand J Prim Health Care 2012; 30: 241–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. GeekInterview.com . Understanding oral and written communication, 2011. http://www.learn.geekinterview.com/career/communication-skills/understanding-oral-written-communication.html (accesed 7 March 2014).
- 13. Campbell B, Vanslembroek K, Whitehead E et al. Views of doctors on clinical correspondence: questionnaire survey and audit of content of letters. BMJ 2004; 328: 1060–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pixy Ferris S. Writing electronically: The effects of computers on traditional writing. J Electronic Publ 2002; 8: DOI: http://dx.doi.org/10.3998/3336451.0008.104. [Google Scholar]
- 15. Jacobs LG, Pringle MA. Referral letters and replies from orthopaedic departments: opportunities missed. BMJ 1990; 301: 470–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Newton J, Eccles M, Hutchinson A. Communication between general practitioners and consultants: what should their letters contain? BMJ 1992; 304: 821–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berendsen AJ, Kuiken A, Benneker WH et al. How do general practitioners and specialists value their mutual communication? A survey BMC Health Serv Res 2009; 9: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carney SL. Medication accuracy and general practitioner referral letters. Intern Med J 2006; 36: 132–4. [DOI] [PubMed] [Google Scholar]
- 19. Garasen H, Johnsen R. The quality of communication about older patients between hospital physicians and general practitioners: a panel study assessment. BMC Health Serv Res 2007; 7: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Farquhar MC, Barclay SI, Earl H et al. Barriers to effective communication across the primary/secondary interface: examples from the ovarian cancer patient journey (a qualitative study). Eur J Cancer Care 2005; 14: 359–66. [DOI] [PubMed] [Google Scholar]
- 21. Stalhammar J, Holmberg L, Svardsudd K, Tibblin G. Written communication from specialists to general practitioners in cancer care. What are the expectations and how are they met? Scand J Prim Health Care 1998; 16: 154–9. [DOI] [PubMed] [Google Scholar]
- 22. Tattersall MH, Butow PN, Brown JE, Thompson JF. Improving doctors’ letters. Med J Aust 2002; 177: 516–20. [DOI] [PubMed] [Google Scholar]
- 23. Hartveit M, Thorsen O, Biringer E et al. Recommended content of referral letters from general practitioners to specialised mental health care: a qualitative multi‐perspective study. BMC Health Serv Res 2013; 13: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jiwa M, Coleman M, McKinley RK. Measuring the quality of referral letters about patients with upper gastrointestinal symptoms. Postgrad Med J 2005; 81: 467–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grol R, Rooijackers‐Lemmers N, van Kaathoven L et al. Communication at the interface: do better referral letters produce better consultant replies? Brit J Gen Pract 2003; 53: 217–9. [PMC free article] [PubMed] [Google Scholar]
- 26. Bado W, Williams CJ. Usefulness of letters from hospitals to general practitioners. Br Med J 1984; 288: 1813–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adhiyaman V, Oke A, White AD, Shah IU. Diagnoses in discharge communications: how far are they reliable? Int J Clin Pract 2000; 54: 457–8. [PubMed] [Google Scholar]
- 28. Tattersall MH, Griffin A, Dunn SM et al. Writing to referring doctors after a new patient consultation. What is wanted and what was contained in letters from one medical oncologist? Aust N Z J Med 1995; 25: 479–82. [DOI] [PubMed] [Google Scholar]
- 29. Durbin J, Barnsley J, Finlayson B et al. Quality of communication between primary health care and mental health care: an examination of referral and discharge letters. J Behav Health Serv Res 2012; 39: 445–61. [DOI] [PubMed] [Google Scholar]
- 30. Wasson J, Pearce L, Alun‐Jones T. Improving correspondence to general practitioners regarding patients attending the ENT emergency clinic: a regional general practitioner survey and audit. J Laryngol Otol 2007; 121: 1189–93. [DOI] [PubMed] [Google Scholar]
- 31. Myers KA, Keely EJ, Dojeiji S, Norman GR. Development of a rating scale to evaluate written communication skills of residents. Acad Med 1999; 74: S111–3. [DOI] [PubMed] [Google Scholar]
- 32. McConnell D, Butow PN, Tattersall MH. Improving the letters we write: an exploration of doctor‐doctor communication in cancer care. Br J Cancer 1999; 80: 427–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mageean RJ. Study of “discharge communications” from hospital. Br Med J 1986; 293: 1283–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Haggerty JL, Reid RJ, Freeman GK et al. Continuity of care: a multidisciplinary review. BMJ 2003; 327: 1219–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Epstein RM. Communication between primary care physicians and consultants. Arch Fam Med 1995; 4: 403–9. [DOI] [PubMed] [Google Scholar]
- 36. Kaelber DC, Bates DW. Health information exchange and patient safety. J Biomed Inform 2007; 40: S40–5. [DOI] [PubMed] [Google Scholar]
- 37. Jiwa M, Dhaliwal S. Referral writer: preliminary evidence for the value of comprehensive referral letters. Qual Prim Care 2012; 20: 39–45. [PubMed] [Google Scholar]
- 38. Preston C, Cheater F, Baker R, Hearnshaw H. Left in limbo: patients’ views on care across the primary/secondary interface. Qual Health Care 1999; 8: 16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med 2004; 79: 186–94. [DOI] [PubMed] [Google Scholar]
- 40. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med 2002; 17: 186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 2003; 18: 646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA 2009; 301: 603–18. [DOI] [PubMed] [Google Scholar]
- 43. Jenkins RM. Quality of general practitioner referrals to outpatient departments: assessment by specialists and a general practitioner. Brit J Gen Pract 1993; 43: 111–3. [PMC free article] [PubMed] [Google Scholar]
- 44. Roy CL, Poon EG, Karson AS et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med 2005; 143: 121–8. [DOI] [PubMed] [Google Scholar]
- 45. Zinn C. 14000 preventable deaths in Australian hospitals. Brit Med J 1995; 310: 1487. [DOI] [PubMed] [Google Scholar]
- 46. Thorne SE, Bultz BD, Baile WF, Team SC. Is there a cost to poor communication in cancer care?: a critical review of the literature. Psycho‐oncology 2005; 14: 875–84; discussion 85‐6. [DOI] [PubMed] [Google Scholar]
- 47. O'Leary KJ, Liebovitz DM, Baker DW. How hospitalists spend their time: insights on efficiency and safety. J Hosp Med 2006; 1: 88–93. [DOI] [PubMed] [Google Scholar]
- 48. Hendrich A, Chow MP, Skierczynski BA, Lu Z. A 36‐hospital time and motion study: how do medical‐surgical nurses spend their time? Permanente J 2008; 12: 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bourguet C, Gilchrist V, McCord G. The consultation and referral process. A report from NEON. Northeastern Ohio Network Research Group. J Fam Pract 1998; 46: 47–53. [PubMed] [Google Scholar]
- 50. Melville C, Hands S, Jones P. Randomised trial of the effects of structuring clinic correspondence. Arch Dis Child 2002; 86: 374–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rao P, Andrei A, Fried A et al. Assessing quality and efficiency of discharge summaries. Am J Med Qual 2005; 20: 337–43. [DOI] [PubMed] [Google Scholar]
- 52. Rawal J, Barnett P, Lloyd BW. Use of structured letters to improve communication between hospital doctors and general practitioners. BMJ 1993; 307: 1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Prince SB, Herrin DM. The role of information technology in healthcare communications, efficiency, and patient safety: application and results. J Nurs Admin 2007; 37: 184–7. [DOI] [PubMed] [Google Scholar]
- 54. Kern LM, Dhopeshwarkar R, Barron Y et al. Measuring the effects of health information technology on quality of care: a novel set of proposed metrics for electronic quality reporting. Jt Comm J Qual Patient Saf 2009; 35: 359–69. [DOI] [PubMed] [Google Scholar]
- 55. Ray S, Archbold RA, Preston S et al. Computer‐generated correspondence for patients attending an open‐access chest pain clinic. J R Coll Physicians Lond 1998; 32: 420–1. [PMC free article] [PubMed] [Google Scholar]
- 56. Oosthuizen JC, McShane D, Kinsella J, Conlon B. General practitioner ENT referral audit. Irish J Med Sci 2015; 184: 143–6 [DOI] [PubMed] [Google Scholar]
- 57. Hilton C, Bajaj P, Hagger M et al. What should prompt an urgent referral to a community mental health team? Ment Health Fam Med 2008; 5: 197–201. [PMC free article] [PubMed] [Google Scholar]
- 58. Jiwa M, Walters S, Mathers N. Referral letters to colorectal surgeons: the impact of peer‐mediated feedback. Brit J Gen Pract 2004; 54: 123–6. [PMC free article] [PubMed] [Google Scholar]
- 59. Keely E, Myers K, Dojeiji S, Campbell C. Peer assessment of outpatient consultation letters–feasibility and satisfaction. BMC Med Educ 2007; 7: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Nestel D, Kidd J. Teaching and learning about written communications in a United Kingdom medical school. Educ Health 2004; 17: 27–34. [DOI] [PubMed] [Google Scholar]
- 61. Sandler DA, Mitchell JR. Interim discharge summaries: how are they best delivered to general practitioners? Br Med J 1987; 295: 1523–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lissauer T, Paterson CM, Simons A, Beard RW. Evaluation of computer generated neonatal discharge summaries. Arch Dis Child 1991; 66: 433–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Smith RP, Holzman GB. The application of a computer data base system to the generation of hospital discharge summaries. Obstet Gynecol 1989; 73: 803–7. [PubMed] [Google Scholar]
- 64. van Walraven C, Laupacis A, Seth R, Wells G. Dictated versus database‐generated discharge summaries: a randomized clinical trial. Can Med Assoc J 1999; 160: 319–26. [PMC free article] [PubMed] [Google Scholar]
- 65. Shere S. Not reading and signing letters you have dictated is dangerous. BMJ 2001; 322: 992. [PMC free article] [PubMed] [Google Scholar]
- 66. Kenny C. Hospital discharge medication: is seven days supply sufficient? Pub Health 1991; 105: 243–7. [DOI] [PubMed] [Google Scholar]
- 67. Kendrick AR, Hindmarsh DJ. Which type of hospital discharge report reaches general practitioners most quickly? BMJ 1989; 298: 362–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Delbanco T, Walker J, Darer JD et al. Open notes: doctors and patients signing on. Ann Intern Med 2010; 153: 121–5. [DOI] [PubMed] [Google Scholar]
- 69. Murray GK, Nandhra H, Hymas N, Hunt N. Copying letters to patients. Psychiatrists omit information from letters when they know patients will be sent copies. BMJ 2003; 326: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Foy R, Hempel S, Rubenstein L et al. Meta‐analysis: effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med 2010; 152: 247–58. [DOI] [PubMed] [Google Scholar]
- 71. Blot K, Bergs J, Vogelaers D et al. Prevention of central line‐associated bloodstream infections through quality improvement interventions: a systematic review and meta‐analysis. Clin Infect Dis 2014; 59: 96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Doran G. There's a S.M.A.R.T. way to write management's goals and objectives. Manage Rev (AMA FORUM) 1981; 70: 35–6. [Google Scholar]


