Abstract
Background
Conflict in North Darfur state, Western Sudan started in 2003, and the delivering of curative health services was becoming a greater challenge for the country's limited resources. NGOs have played an important role in providing curative health services.
Objectives
To examine the role that Non-Governmental Organizations (NGOs) have played in providing curative health services, as well as to identify the difficulties and challenges that affect NGOs in delivering curative health services.
Methods
Secondary data was collected from different sources, including government offices and medical organizations in Sudan and in North Darfur state. Primary data was obtained through interviews with government and NGOs representatives. The interviews were conducted with (1) expatriates working for international NGOs (N=15) (2) health professionals and administrators working in health sector (N= 45) in the period from November 2010 to January 2011.
Results
The government in North Darfur state spent 70% of its financial budget on security, while it spent it less than 1% on providing health services. The international NGOs have been providing 70% of curative health services to the State's population by contributing 52.9% of the health budget and 1 390 health personnel. Since 2003 NGOs have provided technical assistance to the health staff. As a result, more than fifty nurses have been trained to provide care and treatment, more than twenty-three doctors have been trained in laboratory equipment operation, and approximately six senior doctors and hospital directors have received management training. NGOs have been managing and supporting 89 public health facilities, and established 24 health centres in IDP camps, and 20 health centres across all the districts in North Darfur state.
Conclusion
The NGOs have played an important role in providing curative health services and in establishing good health facilities, but a future problem is how the government will run these health facilities after a peaceful settlement has been reached which might cause NGOs to leave the region.
Keywords: NGOs, curative health services, provision, North Darfur state, Sudan
Introduction
While Sudan has been in conflict since independence in 1956, the conflict in North Darfur State1[3] started in 2003. The conflict made the delivery of curative health services in the state an enormous challenge. Health service delivery issues in conflict-affected areas are becoming increasingly important1. The conflict in North Darfur state has destroyed health facilities, displaced people, made delivering services unsafe in the remote areas and led to poverty and diseases. Those affected by the conflict are 1.6 million people, 81% of the State's population, with 37% classified as Internally Displaced Persons (IDPs)2. Therefore, the geographical distribution of the state's population has changed, with 90% of the people concentrated in urban areas and IDP camps. This article had the following objectives. Firstly, this article argued that the conflict in North Darfur led to the government's prioritising securities at the expense of health services. NGOs thus emerged to fill the void that was left by the government and the private sector. Secondly, this essay examined the role played by NGOs in providing curative health services. In particular, this essay explored NGOs activities and the resources that they provided to deliver curative health services. Thirdly, this article identified the difficulties and challenges that affected NGOs in delivering curative health services.
Methods
Both quantitative and qualitative research methods were used. Documentation was collected from different sources, including government offices and medical organizations, and from libraries and academic and research institutes in Sudan and in North Darfur state.
Primary qualitative data was obtained through interviews with government and NGO representatives. Semi-structured questionnaires and guidelines were used. From November 2010 to January 2011, the author conducted interviews with (1) expatriates working for international NGOs (N=15) and (2) health professionals and administrators working in the health sector in the state and district levels (N=45). From a total of 60 interviewees there were 49 (82%) responses. 39 of the respondents were working in the government sector at state and district level, while 10 of them were in the NGO sector.
The research methods included observation, recordings and open interviews. The researcher visited health facilities in the field and took notes, extensively interacting and discussing the issues with health administrators and professionals working in health facilities. A check list of items and themes was prepared in order to examine: curative health service provision; the physical condition of health facilities and equipment; and the management and monitoring practices of health systems and policy. Three health facilities from each category of government health facility (rural hospital, health centre and basic health unit) and one teaching hospital and one specialist hospital were investigated. All the government officials' interviews were conducted in Arabic and transcribed into English. This data was then sorted, arranged, and coded into categories; and subsequently analyzed using content analysis.
Results
The provision of curative health services in North Darfur state
The government in North Darfur state faced difficulties in providing curative health services to the population. The budget allocation for health services has declined steadily from 7.6% of overall state expenditure in 2000 to 5.6% in 2009. By contrast, the budget allocated for security has grown substantially, from 23.7% in 2000 to 38.2% in 20094,5. The consequence of the lack of public funds means that the public sector is unable to meet the population's needs, and thus the responsibility has been transferred to the private sector. However, curative health services in the private sector are very expensive. For example, according to the State Ministry of Finance Report5, 80% of residents earned less than 400 Sudanese pounds, or $ 114 per month in the private sector. For a consultation, a patient needs to pay 25 pounds (US$ 7). All in all, bills of 100–150 Sudanese pounds (US$ 29–43) are not unusual for treatment, which is unaffordable for the low income paid and unemployed segments of the population. At the same time, 80% of the people in rural areas and 47% in urban areas have to live on less than US$ 1 per day (State Ministry of Finance Report5) and they were not able to pay and get curative health services from private health facilities.
The provision of curative health services by the public sector in North Darfur State
Providing curative health services in the public sector is the responsibility of the State Ministry of Health in El Fasher. The State Ministry of Health is responsible for managing all health facilities and procuring drugs and supplies. All hospitals in the public sector are organized into an extensive referral system with a hierarchy of several organisations that provide curative health services, from primary level institutions to teaching and specialist hospitals6.
While the conflict has increased the demand for health care services, it has also, through violence and pillage by different rebel groups, decreased the number of health facilities. The number of primary health care centres decreased from 82 in 2002 to 61 in 2010 (by 26%), the dispensary numbers decreased from 111 in 2002 to 79 in 2010 (by 29%) and the number of basic health units decreased from 203 in 2002 to 130 in 2010 (by 64%)7,8. There is a lack of technical equipment in public health facilities and in most private health facilities.
The provision of curative health services by the private sector in North Darfur State
Since the conflict started in North Darfur state in 2003, the numbers of private health facilities have increased. The number of specialist clinics increased from 15 in 2000 to 29 in 2010 (by 48%), the number of general doctor clinics increased from 5 in 2000 to 14 in 2010 (by 64%) and dental clinics increased from one clinic to three in 2010 (by 67%)7,8.
Private health services are not easily accessible to the poor and conflict-affected people and are mostly concentrated in the El Fasher district. El Fasher monopolizes all private pharmacies, X-ray units, dental clinics, and specialist clinics. 83%, 77% and 57% of public pharmacies, laboratories and general-doctor clinics, respectively, are also located in El Fasher District8.
NGOs providing curative health services in North Darfur State
The conflict and its accompanying insecurity led to the breakdown of North Darfur state's transport and communication infrastructure. This has lead to breakdown of the public health system9. As a result international NGOs have come to play an important role in filling some of the gaps in the public system, and in serving that part of the population (such as IDPs) which is not an attractive market for private providers.
In 2010 there were twenty-two international NGOs providing 70% of health services in North Darfur state8. These NGOs were led by WHO and UNICEF. WHO is not an implementing agency but plays a co-ordinating role. It initiates the necessary health actions in close collaboration with the Federal Ministry of Health, the State Ministry of Health, and NGOs such as Médecins Sans Frontières and Oxfam1.
Beside these twenty-two international NGOs there were three local NGOs that have also been providing health services to the poor and conflict-affected people in thestate. These NGOs are Sudan Red Crescent, the Sudan Humanitarian Aid Development, and Project of Water and Environmental Sanitation - which is supported by UNICEF8. These three organisations concentrate their work in urban areas because of their lack of capacity.
Health facilities managed and supported by the NGO sector
In North Darfur state, NGOs manage and support 89 public health facilities, sometimes in partnership with the State Ministry of Health. Also, NGOs have established 24 health centres in IDP camps, and 20 health centres across all the districts in North Darfur state; this occurred in co-operation with the community and the Ministry of Health8. NGOs also manage and support health facilities in five districts, which include 40 health facilities in El Fasher district, 11 in Kepkabiya, 1 in Umm Kaddada, 22 in Kutum and 15 in Mellit district10. The El Fasher district is an urban area, while the other districts are rural areas.
The important role that NGOs played in providing health services by managing and supporting health facilities was confirmed by an interviewee (22[4]-1, 25 December 2010, El Fasher) in the State Ministry of Health:
In reality due to the conflict which erupted in North Darfur state both levels [Federal and State] failed to take responsibility in providing curative health services to the state people. The conflict resulted in decreasing government revenue for health services and increasing revenue for security. The stability of security comes first by paying most of its budget to control the security situation. Therefore, the NGOs come to take the responsibility of providing curative health services to the poor and conflict-affected people, especially in remote areas and IDPs camps. Also the NGOs play an important role in establishing new health facilities.
The State Ministry of Health also depends on international NGOs to provide human and financial resources to deliver curative health services.
Human resources for curative health services delivery in NGO sector
According to a World Health Organization Report10, in North Darfur state, the number of health workers managed by NGOs (1,390) is more than that of the State Ministry of Health (1,164). The shortage of health staff in the public sector was noted by the interviewees. According to one interviewee (2-2, 15 December 2010, El Fasher) in the State Ministry of Health:
In North Darfur state, we have a shortage of health staff to deliver adequate health services. The number of health workers is not adequate in comparison to population size, which results in poor service. In this regard, we have two problems: shortages in number and inequitable in distribution, and inadequate numbers of trained health care workers.
NGOs also provide training courses for health staff in the public sector, especially for doctors, nurses, and midwives. According to the State Ministry of Health Survey Report8, since 2003 NGOs have provided technical assistance to the health staff. As a result, more than fifty nurses have been trained to provide care and treatment, more than twenty-three doctors have been trained in laboratory equipment operation, and approximately six senior doctors and hospital directors have received management training.
This is confirmed by an interviewee (1-1, 19 January 2011, El Fasher) working in Kepkabiya rural hospital: In Kepkabiya district, we are facing a lack of human resources and most of them are not qualified. NGO health staff help us to train health staff to deliver curative health services, where population numbers increase in the rainy season when malaria spreads. Without NGO health staff assistance, the government sector does not have the capacity and capability to deliver curative health services alone to all people in the district. Besides this assistance with human resources, the government has come to depend on NGOs to finance health services. NGOs over the past few years represent the largest source of financial support for curative health services in the State.
Financial resources for curative health in the NGO sector
In North Darfur state, there are various sources of funding for curative health services.
As seen in Table 1, the federal government's contribution to the health budget in North Darfur state is much greater than that of the state government: 40.3% as opposed to 7.7% in 2003, leading to 26.5% versus 7.4% in 2009, although in 2006 the state's share rose to 12.5%. The North Darfur state government then is very reliant on federal support. However it is also noticeable that the federal government's contribution has declined significantly since 2003. This has not been reflected in monetary terms, however, since the overall sources of funding on health almost quadrupled over a six-year period. The contributions of NGOs have been increased from 30.6 in 2003 to 52.9 in 2009. This was confirmed by an interviewee (2-3, 20 December 2010, El Fasher) in the finance division in the State Ministry of Health:
Government expenditure on health is very little when compared with other services, such as security. For example since the conflict started in North Darfur State, the government spent 70% of its financial budget on security, while it spent it less than 1% on providing health services. The provision of health services in this State is not a governmental priority, leaving the provision of health services to the international NGOs which provide 70% of curative health services to the State's population.
Table 1.
Health finance in North Darfur State, 2003 – 2009.
| Year | Total budget for health in millions of Sudanese pounds |
Federal contribution (%) |
State contribution (%) |
NGO contribution (%) |
Other external support (%) |
| 2003 | 327 | 40.3 | 7.7 | 30.6 | 21.4 |
| 2006 | 480 | 37.5 | 12.5 | 31.3 | 18.7 |
| 2009 | 1 134 | 26.5 | 7.4 | 52.9 | 13.2 |
Sources: State Ministry of Health Financial Reports 2006 and 2009.
As also seen in Table 1, external financial support for health care in North Darfur state is substantial and it has become increasingly so, from 30.6% in 2003 and 31.3% in 2006, growing even more to 52.9% in 2009. The State is therefore greatly dependent on the role of NGOs.
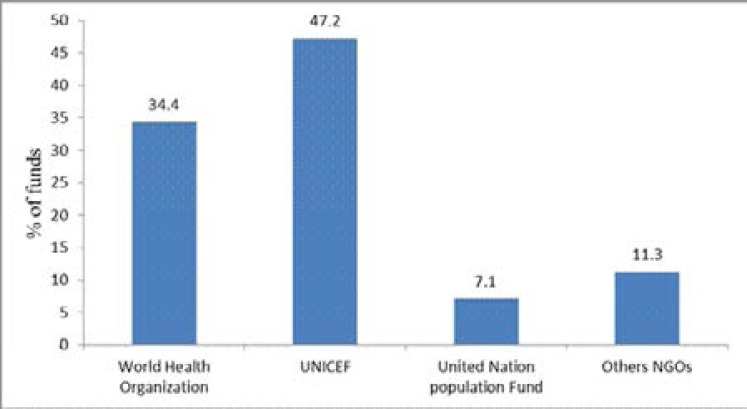
As shown in the Figure 1 above, the main financial support from NGOs for health services in North Darfur state comes from WHO and UNICEF, which contribute 34.4% and 47.2 % of the total health expenditure respectively.
Figure 1.
Relative financial support by NGOs to health services in North Darfur State in 2009.
Source: State Ministry of Health Financial Report5.
The statistical portrait of sources of financing on health was confirmed in most of the interviews. According to an interviewee (2-4, 15 January 2011, El Fasher) in the finance division in the state Ministry of Health:
The State Ministry of Health faces big challenges to finance health services in the State. The government is not able to provide free health services in the public sector because of financial problems. Therefore since the conflict started, the State Ministry of Health is depending completely on donors and international NGOs to support it.
Besides relying on international NGOs, what is noteworthy is North Darfur state's dependency on private user fees. 92% of the expenditure on health services in the public sector in Sudan comes from user fees11.
Discussion
The discussion focuses on the difficulties and challenges that these NGOs face in delivering curative health services, as well as the possibility of sustaining the delivery of curative health services should international NGOs leave the state in the event of the current conflict ending.
Difficulties and challenges that face NGOs in delivering curative health services in the State
NGOs have made an important contribution to curative health service delivery in North Darfur state. They have established 24 health centres and they also provide 70% of curative health services to the IDPs, the poor and vulnerable people of the State. Also, as reported previously, they have provided 52.9% of funds for health care and 1390 health cadres. However, there are many challenges affecting the NGOs' efforts to deliver curative health services to the poor and conflict-affected people, especially in remote areas and IPD camps. These challenges relate to security, political and financial issues.
Firstly, in terms of security issues, NGOs face many difficulties and obstacles in accessing conflict-affected areas because they are mostly controlled by rebel groups. Since the conflict started in Darfur in 2003, most fighting has taken place in North Darfur state and led to NGOs' vehicles being hijacked. The splintering of rebel groups has resulted in a myriad of new groups that are completely undisciplined12. NGOs resources, such as vehicles, are prime targets for these groups. With their lives threatened, NGO staff are forced to give these resources to these groups. Therefore, the security of health staff operating in conflict-affected areas is an increasing obstacle to the success of curative health services delivery for needy people.
Secondly, in terms of political issues, the government is not convinced that NGOs provide health services to the poor and conflict-affected people. The government accuses the NGOs of having a political agenda that serves their countries of origin, especially most international NGOs from Western countries with which the government differs politically and ideologically13.
Therefore, the government has complicated the process of granting permission that NGOs need in order to obtain access to the conflict-affected areas. The process of getting permission to access the conflict-affected areas from security authorities and the humanitarian affairs commission takes four to six days, which compromises the ability of NGOs to provide efficient health services. There have also been cases where the government has expelled NGO workers from Darfur. One example is the case of thirteen NGOs which were expelled from Darfur in early March 2009. Most of these had worked in the health field and this left a huge gap in health services delivery for conflict-affected people13.
Thirdly, in terms of financial issues, the government is often jealous of resources being channelled to NGOs and is wary of the potential that NGOs might be a breeding ground for opposition. NGOs often live in fear of government intervention in their activities5. The NGOs also face difficulties in accessing donor funds which are channelled through the government. These funds are usually given by the donors to the NGOs for specific projects or areas. Inability to access these funds thus jeopardizes these projects. The dominance of international donor support for NGOs has serious implications for the short- and long-term sustainability of their activities.
The possibility of the sustainability of curative health services delivery in the state
A study by Chand and Coffman in a World Health Organization Report14 concluded that in an optimal scenario, donors can successfully disengage some 15–27 years after political conflict has ended. An earlier report by the United States Agency for International Development (2005) recommended at least ten years. By such measures, North Darfur state could contemplate a further decade, perhaps two decades, of assistance from international agencies and NGOs. As long as government depends on NGOs technical and financial support to deliver curative health services to the poor and conflict-affected people, it is currently difficult to see a better alternative to NGOs.
The government faces difficulties in maintaining the level of health financing, especially in conflict-affected areas such as North Darfur state. International NGOs are actively involved in curative health services delivery programmes. In light of the deterioration of government health services infrastructure, NGOs have been providing curative health services in the state, especially in IDP camps, and in remote areas which the government is not able to reach8.
According to the co-ordination between the State Ministry of Health and the NGOs' Office Report15, the delivery of health services which have been carried out by international NGOs during the humanitarian relief phase, compensated for government shortages. This is assisting in the recovery of the health sector and preparing for the return to normality, as well as creating building blocks for future health system development. But the turnover of NGOs in the affected areas has created a vacuum in health services delivery that undermines achievements made during the emergency relief phase. This poses a threat to sustaining health services until longer-term development begins.
The challenges in the recovery period are very critical because the delivery of curative health services to the poor and conflict-affected people in IDP camps and rural areas depends on the NGOs' health resources. Currently some people in rural areas travel approximately 120 kms to gain access the nearest health facility. The question is how the poor and conflict-affected people will obtain curative health services should the NGOs leave the country. The future reconstruction and rehabilitation of health services in North Darfur state remains problematic and unpredictable.
Conclusion
In North Darfur state, the State Ministry of Health has had considerable assistance from NGOs (both international and local) and other stakeholders involved in the financing and delivery of curative health services. NGOs are very active in providing curative health services to the poor and to people affected by conflict in the region. The range of activities carried out by NGOs extends from providing hospitals, clinics and primary health care centres, to providing free consultation and drugs. Therefore these NGOs are important in identifying the people's needs, providing services, linking government and community, and in sharing their expertise. NGOs contribute to curative health service delivery by providing human and financial resources, materials and equipment, sharing information, developing joint projects with government, as well as creating joint committees with government. However, the NGOs face many challenges and obstacles from the government in accessing the conflict-affected areas where health services are in most serious need. Where feasible the NGOs have established health facilities in IDP camps and in the districts, but the real issue is how these can be extended and sustained without much prospect of the Sudanese government being able to meet the expectations of its own comprehensive health services provision.
Acknowledgements
We wish to thank all those who were interviewed. Without their cooperation, we could not have completed this study.
Footnotes
North Darfur State is located in western Sudan and is inhabited by 2 260 262 people, according to information gathered from the census of 20083.
The interviewees and interviews are coded as follows: 1= professional (doctor), 2= administrator. Thus 1-1 indicates an interview with the first professional, 1-2 with the second professional, and so on.
References
- 1.Spiegel P, Checchi F, Colombo S, Paik E. Health-care Needs of People Affected by Conflict: Future Trends and Changing Frameworks. Public Health and HIV Section United Nations High Commissioner for Refugees. Geneva: Switzerland. The Lancet. 2010;375:341–345. doi: 10.1016/S0140-6736(09)61873-0. [DOI] [PubMed] [Google Scholar]
- 2.United Nations, author. Sudan Work Plan 2011. [16/03/2011]. Available from: http://ochadms.unog.ch/quickplace/cap/main.nsf/h_Index/2011_Sudan_Workplan/$FILE/2011_Sudan_Workplan_SCREEN.pdf?openElement.
- 3.Central Bureau of Statistics, author. Fifth Sudan population and housing census. Khartoum, Sudan: 2008. [11/04/2009]. Available from: http://www.cbs.gov.sd/Tiedadat/Tiedadat%205th%20E.htm. [Google Scholar]
- 4.State Ministry of Health Financial Report. North Darfur State, El Fasher: The Final Financial Report of Ministry of Health; 2006. [Google Scholar]
- 5.State Ministry of Health Financial Report. North Darfur State, El Fasher: The Final Financial Report of Ministry of Health; 2009. [Google Scholar]
- 6.State Ministry of Health Survey Report. North Darfur State, El Fasher: The Final Survey Report about Spreads of Diseases in the State; 2009. Dec, [Google Scholar]
- 7.Federal Ministry of Health, Sudan, author. Final Report about Health Facilities and Human Resources in Sudan. Khartoum: 2006. [Google Scholar]
- 8.State Ministry of Health Survey Report. North Darfur State, El Fasher: The Final Survey Report about Spreads of Diseases in the State; 2010. Dec, [Google Scholar]
- 9.Phillips D. Darfur Early Recovery and Development Dossier. Columbia University Center for Study of Human Rights; 2008. [30/03/2009]. Available from: http://hrcolumbia.org/darfur/dossier.pdf. [Google Scholar]
- 10.World Health Organization, author. Health Resources Availability Mapping System, Greater Darfur Report 2nd Quarter. 2010. [15/03/2010]. Available from: http://www.emro.who.int/sudan/pdf/HeRAMS_2Q_2010.pdf.
- 11.World Health Organization, author. Global Health Observatory Data Repository. 2011. [12/05/2011]. Available at http://apps.who.int/ghodata/
- 12.One-click news - western, Arab and African sources, Sudan: the Passion of the Present. 2006. [15/06/2013]. Available from: http://platform.blogs.com/passionofthepresent/
- 13.Wasabi W. Aid Expulsions Leave Huge Gap in Darfur's Health Service. [12/04/2011];World Report. 2009 373 doi: 10.1016/s0140-6736(09)60633-4. Available from: www.thelancet.com. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization, author. Health Cluster Guidance Note on Health Recovery, Report Prepared by the Department of Recovery and Transition Programmes, Health Action in Crisis. 2008. [23/04/2011]. Available from: http://www.who.int/hac/global_health_cluster/guide/117_iasc_global_health_cluster_recovery_strategy_guidelines.pdf.
- 15.State Ministry of Health Report. North Darfur State, El Fasher: A co-ordination between the State Ministry of Health and the NGOs' Office Report; 2010. Dec, [Google Scholar]