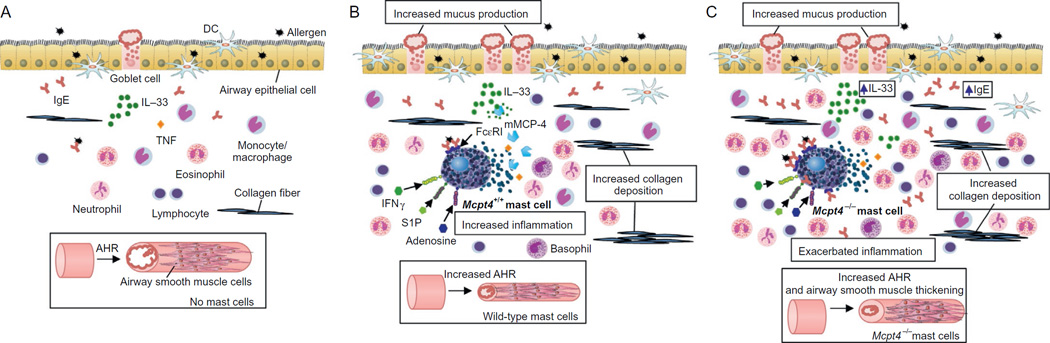
Figure 3. Roles of mast cells (MCs) and mMCP-4 in allergen-induced airway inflammation, airway hyper-responsiveness (AHR), and tissue remodeling.
In the depicted model of allergic airway inflammation (see Nakae et al., 2007; Waern et al., 2009, 2013; Williams & Galli, 2000; Yu et al., 2006, 2011), challenge of sensitized C57BL/6 and WBB6F1 mice with allergen via the airways i.n. produces different tissue responses in c-kit mutant mice lacking MCs or mMCPT-4 than in the corresponding wild-type mice. In mice lacking MCs (A), allergen challenge induces lower levels of AHR to methacholine challenge, airway inflammation, and tissue changes compared to those observed when MCs are present (B and C). (B) In the presence of wild-type MCs, the binding of allergen by IgE molecules bound to adjacent FcεRI molecules induces FcεRI aggregation, activating MCs to secrete preformed mediators (e.g., mMCP-4 and some TNF), lipid mediators, and many cytokines, chemokines, and growth factors. Some aeroallergens (e.g., HDM) can directly induce MC degranulation and secretion of mMCP-4. The secreted mediators can induce migration, maturation, and activation of DCs, amplify inflammatory responses and TH2 cytokine production, enhance AHR, and promote tissue changes, such as goblet cell metaplasia and overproduction of mucus, collagen deposition, and hyperplasia of airway smooth muscle cells. The activation of airway MCs can potentially be modulated by tissue factors, e.g., IFNγ, S1P, adenosine, and IL-33, or by cells, e.g., TH2 cells and Treg cells, which may be present in these sites. Studies in MC knockin mice indicate that some actions of MCs (such as increasing the numbers of epithelial goblet cells) can occur in a model of chronic asthma by MC-dependent mechanisms that do not require MC signaling via the FcεRIγ chain, whereas MCs must express both the FcεRIγ chain and the INFγR to mediate robust increases in lung eosinophils, neutrophils, and collagen (Yu et al., 2006, 2011). (C) In Mcpt4−/− mice which have MCs but lack MC-associated mMCP-4, there are higher levels of serum IgE after sensitization, which may result in increased IgE levels in the airway tissues, as is depicted in the figure. The increased levels of IgE can favor the expression of increased numbers of FcεRI on MCs and basophils. Moreover, compared to the airway changes in wild-type mice (B), in mMCP-4-deficient mice (C), allergen challenge induces exacerbated AHR and enhanced thickening of airway smooth muscle, increased levels of inflammatory cell infiltration (with increases in eosinophils, lymphocytes, and neutrophils), and elevated levels of IL-33 in the airway. In wild-type mice (B), the degradation of IL-33 by MC-derived mMCP-4 can potentially dampen IL-33-mediated eosinophil recruitment, TH2 responses, and IgE production. AHR, airway hyper-responsiveness; TNF, tumor necrosis factor; HDM, house dust mite; DCs, dendritic cells; IFNγ, interferon γ; S1P, sphingosine-1-phosphate.