Abstract
Objective:
The purpose of the present study was to evaluate the efficacy of midazolam-ondansetron combination in prevention of postoperative nausea and vomiting (PONV) after middle ear surgery and its comparison with using midazolam or ondansetron alone.
Methods:
One hundred and forty patients were enrolled in four groups to receive midazolam 0.75 mg/kg in group M, ondansetron 4 mg in group O, midazolam 0.75 mg/kg and ondansetron 4 mg in group MO, and saline 0.90% in group S intravenously just before anesthesia. Assessment of nausea, vomiting, rescue antiemetic, and side effects of study drugs such as headache and dizziness was carried out postoperatively for 24 h.
Findings:
The incidence of PONV was significantly smaller in group MO than group M and group O, while there was no significant difference between group M and group O during the first 24 h postoperatively. Requirement to the additional antiemetic was significantly more in group S (71.4%) compared to other groups, while in group MO (11.4%) was lower than group M (31.4%) and group O (34.3%).
Conclusion:
Our study showed that prophylactic administration of midazolam 0.75 mg/kg combined with ondansetron 4 mg was more effective than using midazolam or ondansetron alone in prevention of PONV after middle ear surgery.
Keywords: Midazolam, middle ear surgery, Ondansetron, postoperative nausea and vomiting
INTRODUCTION
Postoperative nausea and vomiting (PONV) are common and distressing complications and are the main concern of 40–70% of patients after surgery.[1,2] PONV dose not only cause patient discomfort but also can lead to prolongation of stay in the postanesthesia care unit (PACU) and to serious complications including electrolyte imbalance, aspiration, increased bleeding, and wound dehiscence.[3,4] Patients who suffer from PONV require additional healthcare professional time and material resources.[3] The incidence of PONV is approximately 25–30% in general surgery population and between 62% and 80% after middle ear surgery.[5] Many factors such as the site and characteristics of the surgical procedure, the anesthetic technique, as well as the age, gender, weight of the patients, and vertigo history may influence PONV.[6,7] The timing and the dose of the antiemetic agent to be used in the treatment are also important.[8,9,10,11,12,13,14,15,16]
Ondansetron is a 5-hydroxytryptamine 3 (5-HT3) antagonist which usually recommended for prevention and treatment of nausea and vomiting during and after surgery.[17] It works by blocking the action of serotonin, a natural substance, that may cause nausea and vomiting. Midazolam is in a class of medications called benzodiazepines. It has antiemetic effect by augmentation of the inhibitory effects of gamma amino butyric acid and adenosine-mediated inhibition of dopamine in the chemoreceptor trigger zone.[12,18]
The efficacy of ondansetron or midazolam in prevention of PONV was investigated before.[18] In a previous study, the incidence of PONV after using midazolam or ondansetron was 45%[18] and 22%,[5] respectively. Our hypothesis was that using the combination of midazolam with ondansetron probably reduces the incidence of PONV after middle ear surgery better than using each drug singly. There was not previous study about antiemetic effect of midazolam-ondansetron combination, so we design the present study to evaluate the effect of midazolam, ondansetron, and their combination in prevention of PONV after middle ear surgery in comparison with the placebo group.
METHODS
After obtaining institutional approval from Ethic Committee of university and informed consent from patients, 140 American Society of Anesthesiologist I or II patients, aged 18–62 years who were eligible to participate in this double-blinded randomized clinical trial. These patients were scheduled for elective middle ear surgery, mastoidectomy, or tympanoplasty. Patients with previous history of motion sickness, antiemetic therapy within 24h preoperatively, patients on opioid treatment, smokers, and pregnant patients were not included. If anesthetic technique was changed, the patients were excluded from the study.
Patients were randomized into four groups receiving midazolam 0.75 mg/kg (group M), ondansetron 4 mg (group O), combination of midazolam 0.75 mg/kg and ondansetron 4 mg (group MO), and saline 0.9% (group S) intravenously (IV) before induction of anesthesia. The randomization was done by using random allocation software. The study drugs were administered by an anesthesiologist blinded to data collection.[17]
Before induction of anesthesia, the patients were informed on the using the visual analog scale (VAS) for nausea and pain evaluation. The monitoring was performed by continuous electrocardiogram, noninvasive blood pressure, pulse oximetry, and end-tidal carbon dioxide. Induction of anesthesia was done with sodium thiopental 5 mg/kg, fentanyl 2 µg/kg, and atracurium 0.6 mg/kg. General anesthesia was maintained with 100–150 µg/kg/min propofol infusion and morphine 0.1 mg/kg for analgesia. Neuromuscular blockage was reversed with neostigmine 0.4 mg/kg and atropine 0.2 mg/kg and after that patients were extubated.
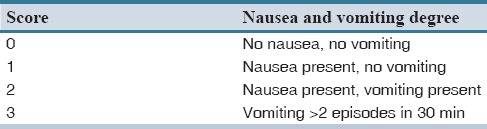
PONV were evaluated using nausea-vomiting score at 0–2 h and 2–24 h [Table 1]. Vomiting was defined as forceful expulsion of gastric contents from mouth or retching.[19,20] Postoperative nausea and pain intensity were evaluated by using VAS at 0–2 and 2–24 h with 0 = no pain or PONV and 10 = the worst imaginable pain or PONV. Patients with a PONV score of 2 or more were given IV metoclopramide 0.15 mg/kg, and that dose was recorded. Time to the first oral intake was recorded. Patients with a pain score of 4 or more were given diclofenac suppository 50 mg and its dose was recorded.
Table 1.
Nausea and vomiting score
Length of staying in the recovery room was evaluated by using Modified Aldrete Score. Extubation time (defined since discontinuation of anesthetic drugs until removal of endotracheal tube) was also recorded.
The patient's satisfaction was rated on a 10-point scale from 0 to 10 where 0 represented “no satisfaction at all and 10 represented complete satisfaction.”[19] Complete response was defined as absence of nausea and vomiting during 24 h postoperatively.[19] Consciousness was assessed based on Observer's Assessment of Alertness/Sedation scale at the time of evaluation of nausea and vomiting (where 1 = awake/alert, and 5 = deep sleep).
The sample size was estimated based on a power calculation which showed that 35 patients per group were necessary to achieve 80% power to detect a 30% difference (from 50% to 20%) in the incidence of PONV between group O with group MO with α =0.05 The data was presented as mean ± standard deviation or numbers (%). Differences among groups for quantitative variables was analyzed by using one-way analysis of variance (ANOVA) and post hoc comparisons at various points in time by using Bonferroni's type I error rate correction for multiple tests of significance. Analysis of continuous variables was done by using repeated measure ANOVA. Categorical variables were analyzed by using Chi-square test. Mann–Whitney U-test and Kruskal–Wallis test were used as appropriate. P <0.05 was considered statistically significant. The analysis of data was performed by using SPSS 20.0 software for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
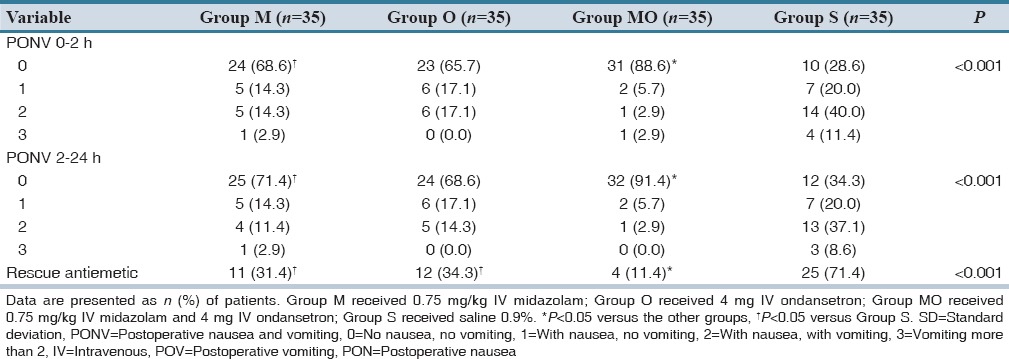
One hundred forty patients were randomly allocated into four groups, and no patient was excluded. Patient characteristics, operation type, duration of surgery, duration of anesthesia, time to oral intake, extubation time, PACU time, and patient satisfaction are shown in Table 2. Time to oral intake was significantly higher in group S (P < 0.001) than to the other groups. PACU time was not significantly different between the four groups [Table 2]. Postoperatively, 11 patients (31.4%) in group M, 12 patients (34.2%) in group O, 4 patients (11.4%) in group MO, and 25 patients (71.4%) in group S, received 0.15 mg/kg metoclopramide IV and there was significant difference between group MO and the other groups (P < 0.001). PONV was significantly less in those patients who received a combination of midazolam and ondansetron as compared to the other groups [Table 3]. Subsequently, the difference was not significant between group M and group O. However, PONV in both of them were significantly less as compared to group S [Table 3]. There was no significant difference between group M with group O in this respect. The overall patient satisfaction was significantly higher in the group MO compared the other groups [P < 0.001, Table 2].
Table 2.
Demographic characteristics and para-clinical data of patients
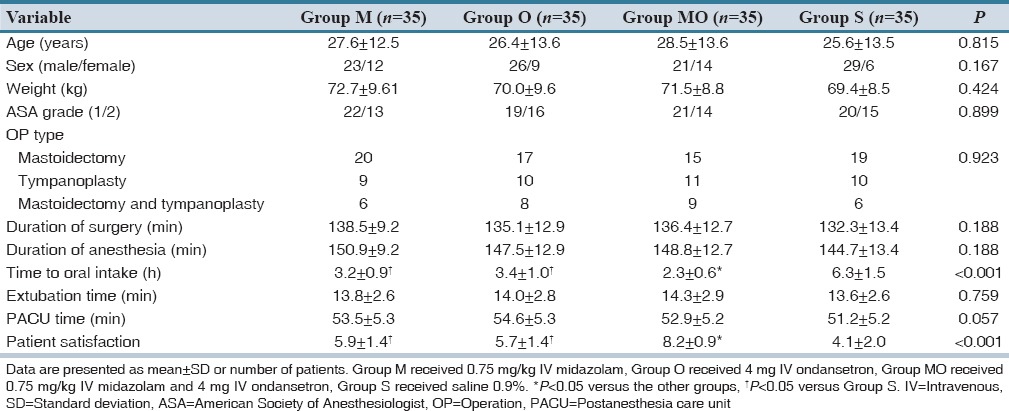
Table 3.
The incidence of patients with PON, POV, PONV and requiring rescue antiemetic in four groups
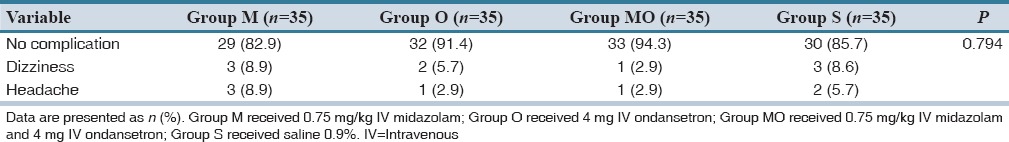
VAS of nausea in group MO was significantly less than other groups (P < 0.001). There was no significant difference between VAS of pain in four groups [Table 4]. No significant difference was found between groups in terms of side effects such as dizziness and headache [Table 5].
Table 4.
Severity of postoperative nausea and pain in four groups
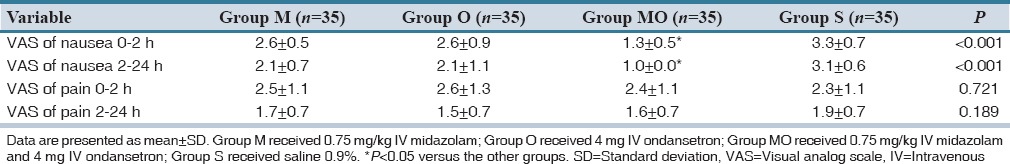
Table 5.
The incidence of postoperative adverse effects in four groups
DISCUSSION
In the present study, we aimed to compare the antiemetic effect of the combination of midazolam-ondansetron with midazolam and ondansetron single and placebo group. We evaluated the incidence of nausea and vomiting and their severity in the first 24 h and the number of patients with nausea and vomiting who used additional antiemetic between 0–2 and 2–24 h. We measured postoperative pain based on VAS which could effect on the incidence of PONV, and there was no significant difference in pain intensity between groups.
In this study, we found the incidence of PONV was significantly smaller in group MO than group M and group O and there was no significant difference between group M and group O. Need to the additional antiemetic was significantly lower in group MO compared with group M or group O.
The use of 5-HT3 receptor antagonists is popular as the drugs have shown good efficacy in preventing PONV.[3,21,22,23,24,25,26] These drugs act by two mechanisms: First, by blocking the 5-HT3 receptors in the area postrema and nucleus tractus solitarius; and second, by blocking peripherally afferent vagal impulses originating from 5-HT3 receptors in the mucosa of the gastrointestinal tract.[27] It has been reported that after prophylactic administration of 4 mg ondansetron in radical mastoidectomy, nausea, and vomiting occurred at the rate of 33% while they occurred at the rate of 81.5% after placebo.[28] Tramèr et al.[29,30] found that the anti-vomiting efficacy of ondansetron was consistently better than the anti-nausea efficacy. In this study, patients who received ondansetron showed a higher incidence of nausea than those who received midazolam in the first 24 h; however, this difference was not significant.
Midazolam is a short-acting drug in the benzodiazepine class. Splinter et al.[31] observed that administering midazolam 0.05 mg/kg after induction of anesthesia had antiemetic effects that were similar to the same dose of droperidol in children undergoing strabismus surgery. Bauer et al.[32] found that preoperative IV midazolam 0.04 mg/kg was an effective way to reduce the frequency of PONV and increased patient satisfaction. Recently, Splinter et al.[33] demonstrated that midazolam used in sub-hypnotic dose was as effective as ondansetron in treating PONV without untoward sedative effects. The results of the above studies are comparable with the results of our study.
Midazolam antiemetic effect is triggered by glycine mimetic inhibitory effect, augmentation of the inhibitory effect of gamma-amino-butyric acid, augmentation of adenosinergic effects, inhibition of dopamine release, and augmentation of adenosine-mediated inhibition of dopamine in the chemoreceptor trigger zone.[33]
One of the clinical effects of midazolam is sedation. It was probable that the using midazolam prolonged sedation time in the recovery room. Our study showed that midazolam did not prolong PACU and extubation time. It was due to using sub-hypnotic dose midazolam for prevention of PONV. It was presumed from the results of our study that the more efficacy of using midazolam-ondansetron combination in comparison with using each drug singly originates from the synergistic effect of two drugs.
In conclusion, our study showed that the prophylactic antiemetic effect of the combination of 0.75 mg/kg midazolam with 4 mg ondansetron was superior to using midazolam or ondansetron singly in the first 24 h after operation. Further studies using this combination in the other surgeries with high incidence of PONV is recommended.
AUTHORS’ CONTRIBUTIONS
MRS has planned the study and finalized it; AH, MC, MN, and MRS did the statistical analysis and prepared the first version of manuscript for publishing. All authors read and approved the final manuscript.
Financial support and sponsorship
Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank sincerely the support of all the colleagues in Kashani Hospital Medical Center affiliated to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This prospective randomized observational study was approved by the Ethics Committee of our university, (Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran) and all patients gave written, informed consent.
REFERENCES
- 1.Koivuranta MK, Läärä E, Ryhänen PT. Antiemetic efficacy of prophylactic ondansetron in laparoscopic cholecystectomy. A randomised, double-blind, placebo-controlled trial. Anaesthesia. 1996;51:52–55. doi: 10.1111/j.1365-2044.1996.tb07654.x. [DOI] [PubMed] [Google Scholar]
- 2.Gan T, Sloan F, Dear Gde L, El-Moalem HE, Lubarsky DA. How much are patients willing to pay to avoid postoperative nausea and vomiting? Anesth Analg. 2001;92:393–400. doi: 10.1097/00000539-200102000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Tang J, White PF, Wender RH, Quon R, Sloninsky A, et al. The effect of timing of dolasetron administration on its efficacy as a prophylactic antiemetic in the ambulatory setting. Anesth Analg. 2001;93:906–11. doi: 10.1097/00000539-200110000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Frighetto L, Loewen PS, Dolman J, Marra CA. Cost-effectiveness of prophylactic dolasetron or droperidol vs rescue therapy in the prevention of PONV in ambulatory gynecologic surgery. Can J Anaesth. 1999;46:536–43. doi: 10.1007/BF03013543. [DOI] [PubMed] [Google Scholar]
- 5.Isik B, Cekmen N, Arslan M, Ozsoylar O, Kordan AZ, Akcabay M. Comparison of the antiemetic effects of ondansetron and dexamethasone on middle ear surgery. Saudi Med J. 2006;27:646–51. [PubMed] [Google Scholar]
- 6.Habib AS, Gan TJ. Evidence-based management of postoperative nausea and vomiting: A review. Can J Anaesth. 2004;51:326–41. doi: 10.1007/BF03018236. [DOI] [PubMed] [Google Scholar]
- 7.Apfel CC, Greim CA, Haubitz I, Grundt D, Goepfert C, Sefrin P, et al. The discriminating power of a risk score for postoperative vomiting in adults undergoing various types of surgery. Acta Anaesthesiol Scand. 1998;42:502–9. doi: 10.1111/j.1399-6576.1998.tb05158.x. [DOI] [PubMed] [Google Scholar]
- 8.American Society of Health System Pharmacists. ASHS Therapeutic guideline on the management of nausea and vomiting in adult and pediatric patients receiving chemotherapy or radiation therapy or undergoing surgery. Am J Health Syst Pharm. 1999;56:729–64. doi: 10.1093/ajhp/56.8.729. [DOI] [PubMed] [Google Scholar]
- 9.Wang JJ, Ho ST, Tzeng JI, Tang CS. The effect of timing of dexamethasone administration on its efficacy as a prophylactic antiemetic for postoperative nausea and vomiting. Anesth Analg. 2000;91:136–9. doi: 10.1097/00000539-200007000-00025. [DOI] [PubMed] [Google Scholar]
- 10.McRae RG, Weissburg AJ, Chang KW. Iatrogenic hyponatremia: A cause of death following pediatric tonsillectomy. Int J Pediatr Otorhinolaryngol. 1994;30:227–32. doi: 10.1016/0165-5876(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 11.Gayer S, Lubarsky DA. Cost-effective Antiemesis. Int Anesthesiol Clin. 2003;41:145–64. doi: 10.1097/00004311-200341040-00011. [DOI] [PubMed] [Google Scholar]
- 12.Tramèr MR. Strategies for postoperative nausea and vomiting. Best Pract Res Clin Anaesthesiol. 2004;18:693–701. doi: 10.1016/j.bpa.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Goksu S, Kocoglu H, Bayazit YA, Yüksek S, Karci Y, Kanlikama M, et al. Antiemetic effects of granisetron, droperidol and dexamethasone in otologic surgery. Auris Nasus Larynx. 2002;29:253–6. doi: 10.1016/s0385-8146(02)00004-4. [DOI] [PubMed] [Google Scholar]
- 14.Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. 2000;59:213–43. doi: 10.2165/00003495-200059020-00005. [DOI] [PubMed] [Google Scholar]
- 15.Nader ND, Simpson G, Reedy RL. Middle ear pressure changes after nitrous oxide anesthesia and its effect on postoperative nausea and vomiting. Laryngoscope. 2004;114:883–6. doi: 10.1097/00005537-200405000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Naylor RJ, Inall FC. The physiology and pharmacology of postoperative nausea and vomiting. Anaesthesia. 1994;49 Suppl:2–5. doi: 10.1111/j.1365-2044.1994.tb03575.x. [DOI] [PubMed] [Google Scholar]
- 17.Safavi M, Honarmand A, Negahban M, Attari M. Prophylactic effects of intrathecal Meperidine and intravenous Ondansetron on shivering in patients undergoing lower extremity orthopedic surgery under spinal anesthesia. J Res Pharm Pract. 2014;3:94–9. doi: 10.4103/2279-042X.141105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Honarmand A, Safavi M, Khalili G, Mohammadnejad F. Prophylactic administration of haloperidol plus midazolam reduces postoperative nausea and vomiting better than using each drug alone in patients undergoing middle ear surgery. Saudi J Anaesth. 2012;6:145–51. doi: 10.4103/1658-354X.97028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grover VK, Mathew PJ, Hegde H. Efficacy of orally disintegrating ondansetron in preventing postoperative nausea and vomiting after laparoscopic cholecystectomy: A randomised, double-blind placebo controlled study. Anaesthesia. 2009;64:595–600. doi: 10.1111/j.1365-2044.2008.05860.x. [DOI] [PubMed] [Google Scholar]
- 20.Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Honkavaara P. Effect of ondansetron on nausea and vomiting after middle ear surgery during general anaesthesia. Br J Anaesth. 1996;76:316–8. doi: 10.1093/bja/76.2.316. [DOI] [PubMed] [Google Scholar]
- 22.Russell D, Kenny GN. 5-HT3 antagonists in postoperative nausea and vomiting. Br J Anaesth. 1992;69(7 Suppl 1):63S–8S. doi: 10.1093/bja/69.supplement_1.63s. [DOI] [PubMed] [Google Scholar]
- 23.Naguib M, el Bakry AK, Khoshim MH, Channa AB, el Gammal M, el Gammal K, et al. Prophylactic antiemetic therapy with ondansetron, tropisetron, granisetron and metoclopramide in patients undergoing laparoscopic cholecystectomy: A randomized, double-blind comparison with placebo. Can J Anaesth. 1996;43:226–31. doi: 10.1007/BF03011739. [DOI] [PubMed] [Google Scholar]
- 24.Steinbrook RA, Freiberger D, Gosnell JL, Brooks DC. Prophylactic antiemetic for laparoscopic Cholecystectomy: Ondansetron versus droperidol olus metoclopramide. Anesth Analg. 1996;83:1081–3. doi: 10.1097/00000539-199611000-00032. [DOI] [PubMed] [Google Scholar]
- 25.Steinbrook RA, Gosnell JL, Freiberger D. Prophylactic antiemetics for laparoscopic cholecystectomy: A comparison of perphenazine, droperidol plus ondansetron, and droperidol plus metoclopramide. J Clin Anesth. 1998;10:494–8. doi: 10.1016/s0952-8180(98)00077-4. [DOI] [PubMed] [Google Scholar]
- 26.Philip BK, Pearman MH, Kovac AL, Chelly JE, Wetchler BV, McKenzie R, et al. Dolasetron for the prevention of postoperative nausea and vomiting following outpatient surgery with general anaesthesia: A randomized, placebo-controlled study. The Dolasetron PONV Prevention Study Group. Eur J Anaesthesiol. 2000;17:23–32. doi: 10.1046/j.1365-2346.2000.00594.x. [DOI] [PubMed] [Google Scholar]
- 27.Gyermek L. Pharmacology of serotonin as related to anesthesia. J Clin Anesth. 1996;8:402–25. doi: 10.1016/0952-8180(96)00093-1. [DOI] [PubMed] [Google Scholar]
- 28.Sadhasivam S, Saxena A, Kathirvel S, Kannan TR, Trikha A, Mohan V. The safety and efficacy of prophylactic ondansetron in patients undergoing modified radical mastectomy. Anesth Analg. 1999;89:1340–5. doi: 10.1097/00000539-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Tramèr MR, Phillips C, Reynolds DJ, McQuay HJ, Moore RA. Cost-effectiveness of ondansetron for postoperative nausea and vomiting. Anaesthesia. 1999;54:226–34. doi: 10.1046/j.1365-2044.1999.00704.x. [DOI] [PubMed] [Google Scholar]
- 30.Tramèr MR, Reynolds DJ, Moore RA, McQuay HJ. Efficacy, dose-response, and safety of ondansetron in prevention of postoperative nausea and vomiting: A quantitative systematic review of randomized placebo-controlled trials. Anesthesiology. 1997;87:1277–89. doi: 10.1097/00000542-199712000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Splinter W, Noël LP, Roberts D, Rhine E, Bonn G, Clarke W. Antiemetic prophylaxis for strabismus surgery. Can J Ophthalmol. 1994;29:224–6. [PubMed] [Google Scholar]
- 32.Bauer KP, Dom PM, Ramirez AM, O’Flaherty JE. Preoperative intravenous midazolam: Benefits beyond anxiolysis. J Clin Anesth. 2004;16:177–83. doi: 10.1016/j.jclinane.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Splinter WM, MacNeill HB, Menard EA, Rhine EJ, Roberts DJ, Gould MH. Midazolam reduces vomiting after tonsillectomy in children. Can J Anaesth. 1995;42:201–3. doi: 10.1007/BF03010676. [DOI] [PubMed] [Google Scholar]


