Abstract
Gardner-Diamond syndrome (GDS) is an uncommon disease clinically characterized by a wide spectrum of psycho-emotive symptoms associated with painful ecchymoses/purpuric lesions and positivity of auto-erythrocyte sensitization skin test. Herein, a perspective clinical and psychological observation of an adolescent GDS is firstly reported focusing on her psychological features long-term monitored for a 1-year period. The administration of a standardized tools battery allowed us to define psychological features of the young patient over time and to monitored clinical course and response to treatment.
Keywords: Adolescent auto erythrocyte sensitization syndrome, Gardner-Diamond syndrome, psychogenic purpura, unexplained medical symptoms
INTRODUCTION
Gardner-Diamond syndrome (GDS) is an uncommon clinical entity firstly described in 1955, when Frank Gardner and Louis Diamond reported four adult women who developed spontaneous bruising lesions several months after sustaining a trauma.[1]
Young women are more commonly affected. They develop cutaneous symptoms characterized by recurrent flare-ups of ecchymotic painful bruising episodes unrelated to haematologic or coagulation defects. Other unspecific symptoms as well as malaise, abdominal pain, headache, arthralgia, myalgia may be also occur.[2,3]
Concurrently, psycho-emotive disorders, namely depressive symptomatology, occur. Upon these protean clinical features, GDS may be easily misdiagnosed. The auto-sensitization to phosphatidylserine of erythrocyte surface found in the majority of the patients represents a useful diagnostic tool.
Herein, we report an adolescent affected with GDS, focusing on:
The misleading clinical features of this patient;
The long-term perspective psychological assessment of the patient aimed to investigate the personality profile, the clinical course and the response to treatment, monitoring the patient over time with follow-up meetings.
CASE REPORT
A 16-year-old white girl was admitted to our Institute in 2013 for painful bruising of the lower limbs associated with recurrent fever spikes, diarrhoea and aphthous stomatitis. Oedema of the extremities and headache were also referred.
The patient was well up 14, when she developed weight loss, diarrhoea, abdominal pain, recurrent purpuric skin lesions and buccal aphthous lesions. Laboratory tests (complete blood cell count, acute phase reactants urine and stool examination) were persistently negative.
As the symptoms, albeit unspecific, severely restricted her activities, the patient underwent an extensive diagnostic process consulting many specialists. Cutaneous lesions which showed recurrent flare-ups were biopsied twice. No evidence of vasculitis was disclosed. Since abdominal pain, diarrhoea and haematochezia persisted, two ileocolonscopies with multiple biopsies were performed, showed only an aspecific mucosal inflammation. The girl was also investigated by a psychiatrist who suspected an eating disorder. Head computed tomography (CT) and whole body magnetic resonance imaging (MRI) were negative. Nonetheless this diagnostic odyssey, any diagnosis was pointed out.
In the following months the muco-cutaneous symptoms worsened, so the patient came to our observation with the diagnosis of Behçet disease.
At admittance, patient's clinical examination showed poor conditions. Severe underweight, widespread painful bruising lesions at head, upper and lower limbs associated with oedema and dysesthesia of the involved regions were present [Figure 1]. The patient referred arthro-myalgias without signs of arthritis and refused to walk. Secondary amenorrhea was referred from 6 months.
Figure 1.

Bruising lesion localized to the hands with edema and dysesthesia
Since the girl showed also a low mood, an extensive psychological examination was performed.
At first glance, the patient appeared to be seemingly well adjusted. On careful probing, an emotional vulnerability was evident. Moreover depression, social withdrawal (e.g., a private teacher gave her home lessons for 1 year and then she totally refused school), anhedonia, trouble sleeping, irritability, social isolation were present.
Complete blood cell count, erythrocyte sedimentation rate, C reactive protein, coagulation function, proteinemia, antinuclear auto-antibodies and anti-double stranded deoxyribonucleic acid (DNA) antibodies tests were normal or absent.
Taken together, these findings seemed suggestive for GDS. The positive auto-erythrocyte sensitization test allowed us to confirm the diagnosis,[4] After 4 hours, a painful and reddish plaque appeared on the site of erythrocyte injection whereas no reaction was present in the control site.
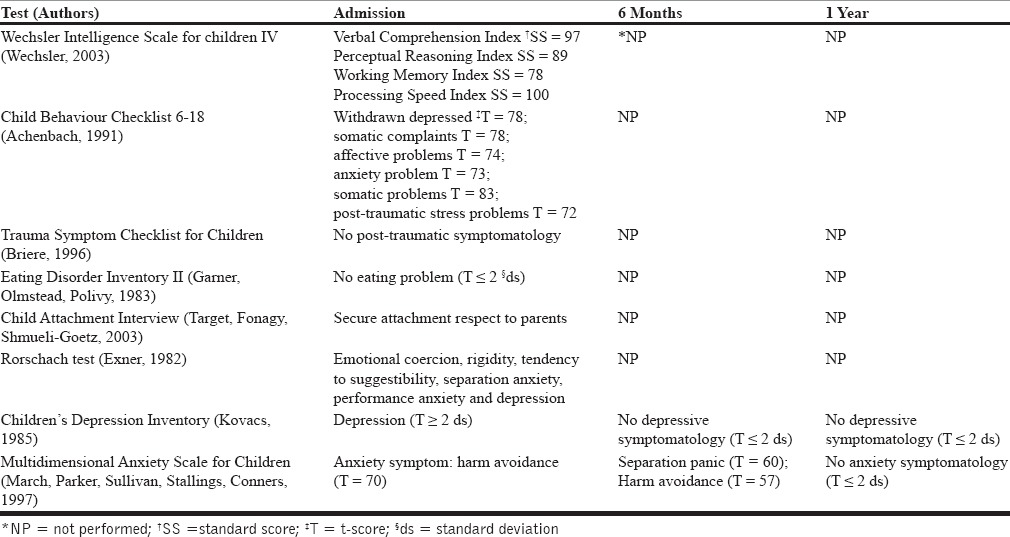
Psychological assessment was based upon different psychological tools [Table 1] administered for defining the patient personality profile. For getting a long-term perspective standardized evaluation, we have periodically re-evaluated the patient 6 and 12 months later, using some of tools yet administered by the same psychologist. Thus, the response of the patient either to drug treatment and psychological treatment was assessed.
Table 1.
Battery of psychological tools and results
Drug anti-depressant treatment with amitriptyline (5 mg twice a day), psychotherapy and parent counselling were started when she was 16.
Initial psychological assessment showed a normal cognitive functioning with poor working memory skill. Emotional state showed emotional coercion, rigidity, depression and anxiety.
Six months after discharge the patient showed good therapeutic alliance and compliance with drug therapy. As shown standardized tools, anxiety symptoms improved and depressive symptoms were absent. She gradually accepted the diagnosis. An impaired social behaviour and underweight were still persistent.
One year from diagnosis, psychological follow-up assessment shows absence of depressive and anxiety symptoms. At present patient social behaviour, daily activities, future planning and underweight are frankly improved, whereas the personality traits characterized by rigidity and low openness emotional remained unchanged.
DISCUSSION
GDS, also named psychogenic purpura, auto-erythrocyte sensitization syndrome or painful bruising syndrome,[1] is still an unsolved diagnostic conundrum for the paediatrician since it mimics diseases quite heterogeneous for etiology and course (e.g., coagulation defects, erythema nodosum, Ehlers-Danlos disease, systemic lupus erythematosus, panniculitis, Schoemberg dermatosis, Munchausen syndrome).
Skin lesions are the most common GDS heralding symptoms. Widespread, painful and reddish plaques occur associated with induration and thickening of subcutaneous. While lesions gradually turn onto ecchymoses, new flare-ups may appear.
Overall cutaneous lesions are not specific. Skin biopsy is consistent for an unspecific perivascular lymphohystiocytic infiltrate. Since gastrointestinal and systemicsymptoms may occur, the disease often remains undiagnosed for long time.
Psychological features strongly characterized GDS and their correct assessment is mandatory for diagnosis and a correct treatment. The patients reported commonly disclose hysterical and psycho-infantile personality traits, emotional vulnerability, tendency to somatic reactions to emotional stimuli, sexual complains, feelings of hostility, dysphoric-explosive behaviour and obsessive-compulsive disorder.[5,6,7,8]
GDS patients undergo a diagnostic odyssey. Long-term medicalization of patients and their families, high social costs, frustration of the medical team, patient and family are commonly experienced.[9,10]
So far, long-term observational studies are lacking. This is the first psychological study with perspective follow-up. Monitoring allowed a standardized assessment of the clinical course. Combined pharmacological and psychotherapeutic treatment seemed to have improved the depressive and anxiety symptoms.
Treatment of GDS is still a particular problem. No method of treatment was sufficiently effective in this disease. In some patients, psychotropic medications were successfully prescribed according to type of psychopathological disorders and psychotherapy was used to improved skin condition and psychic disorders.[6,8]
This orphan-disease may lead to both severe physical and psychological impairment. It is important to establish a multidisciplinary working team aimed diagnose and correctly treat these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gardner FH, Diamond LK. Autoerythrocyte sensitization; a form of purpura producing painful bruising following auto-sensitization to red blood cells in certain women. Blood. 1955;10:675–90. [PubMed] [Google Scholar]
- 2.Kakihara T, Tanaka A, Imai C, Ikarashi Y, Uchiyama M, Emura I. Psychosomatic reaction exhibiting hemorrhagic erythema and motorsensory disturbance. Pediatr Int. 2003;45:472–4. doi: 10.1046/j.1442-200x.2003.01765.x. [DOI] [PubMed] [Google Scholar]
- 3.Edinger LK, Schwartzman RJ. Gardner-Diamond syndrome associated with complex regional pain syndrome. J Dermatol Case Rep. 2013;7:10–4. doi: 10.3315/jdcr.2013.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silny W, Marciniak A, Czarnecka-Operacz M, Zaba R, Schwartz RA. Gardner-Diamond syndrome. Int J Dermatol. 2010;49:1178–81. doi: 10.1111/j.1365-4632.2009.04396.x. [DOI] [PubMed] [Google Scholar]
- 5.Hällström T, Hersle K, Mobacken H. Mental symptoms and personality structure in autoerythrocyte sensitization syndrome. Br J Psychiatry. 1969;115:1269–76. doi: 10.1192/bjp.115.528.1269. [DOI] [PubMed] [Google Scholar]
- 6.Ivanov OL, Lvov AN, Michenko AV, Künzel J, Mayser P, Gieler U. Autoerythrocyte sensitization syndrome (Gardner-Diamond syndrome): Review of the literature. J Eur Acad Dermatol Venereol. 2009;23:499–504. doi: 10.1111/j.1468-3083.2009.03096.x. [DOI] [PubMed] [Google Scholar]
- 7.Ratnoff OD. Psychogenic purpura (autoerythrocyte sensitization): An unsolved dilemma. Am J Med. 1989;87:16–21N. [PubMed] [Google Scholar]
- 8.Sawant NS, Singh DA. Antidepressant-induced remission of Gardner Diamond syndrome. Indian J Psychol Med. 2012;34:388–90. doi: 10.4103/0253-7176.108229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta MA. Somatization disorders in dermatology. Int Rev Psychiatry. 2006;18:41–7. doi: 10.1080/09540260500466832. [DOI] [PubMed] [Google Scholar]
- 10.Meeder R, Bannister S. Gardner-Diamond syndrome: Difficulties in the management of patients with unexplained medical symptoms. Paediatr Child Health. 2006;11:416–9. doi: 10.1093/pch/11.7.416. [DOI] [PMC free article] [PubMed] [Google Scholar]


