A 52-year-old male with history of metastatic melanoma of unknown primary, stage IV with metastases to the left iliac region as well as pancreatic head was diagnosed in early 2014. The metastatic melanoma to the iliac bone presented as a large painful lesion and radiologically as a large lytic lesion. He was treated with palliative radiotherapy, 27 Gy in 3 fractions completed in March 2014 and at about the same time started on Ipilimumab at 3 mg/kg intravenous (230 mg) every 3 weeks for a total of 4 doses, the last one in May 2014. Six days following the second dose of Ipilimumab, the patient presented with a gingival swelling on the lingual aspect of the right mandible. On examination, there was a swelling of the lingual gingiva adjacent to the right mandibular molars, localized bleeding on probing, mild discomfort, and a small amount of purulent discharge was expressed from the gingival sulcus on palpation (Fig. 1A). Panoramic and periapical radiographs showed no obvious radiopaque or radiolucent lesions. The area was irrigated with 0.12% chlorhexidine. He was advised to irrigate the area 3 times per day with chlorhexidine. One week later, he presented for a follow-up, at which time he said “it doesn't feel better”. On examination, the swelling had progressed, a fistula was noted from the lingual area of the right mandibular second molar to the mylohyoid space, and on palpation purulence was expressed from the fistula with slight discomfort. Nevertheless, the patient had excellent oral hygiene. He was prescribed Augmentin 875 mg bid for 7 days. A month later, he presented with a complaint of “my other doctor thought he saw some exposed bone in the area that we have been watching”. He stated that it was asymptomatic; however his tongue noticed something rough. On examination, there was a 2 × 2 mm exposed necrotic-appearing bone on the lingual aspect of the right mandibular second molar (Fig. 1B), there was slight purulence on palpation and the bone was mobile but no tenderness or sensitivity on manipulation. The patient was instructed to continue with the chlorhexidine rinse. In 3 weeks, he returned with the complaint of “the bone is moving around now and bothering my tongue”. There was no history of pain from that area. On examination, an area of exposed necrotic bone measuring 10 × 5 mm was present (Fig. 1C); the bone was very mobile and easily removed with cotton forceps with no associated pain or bleeding on removal. The patient was advised to continue the chlorhexidine rinse. The specimen was submitted for histopathologic evaluation (Fig. 1D), which was reported as a non-vital bone (sequestrum) with bacterial colonies consistent with actinomyces species associated with acute inflammatory cells (Fig. 1E). At his 2 month follow-up examination, the area had fully resolved and healed with no purulent discharge or pain on palpation (Fig. 1F).
Fig. 1.
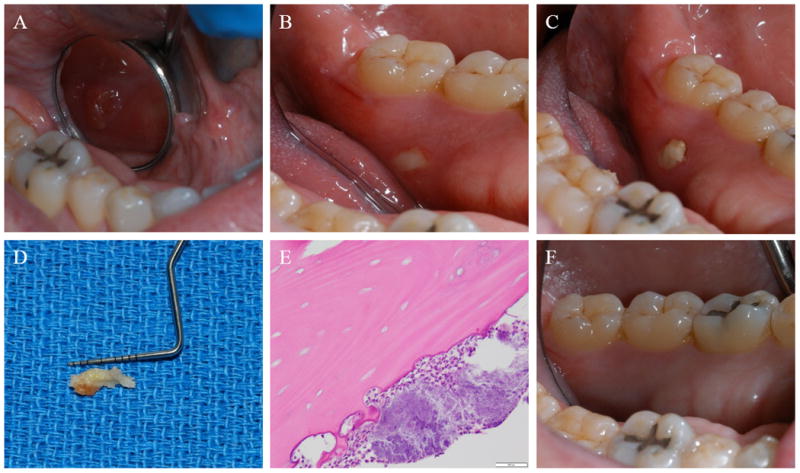
Clinical picture at initial presentation showing a gingival swelling (A), clinical picture a month later showing a 2 × 2 mm area of exposed bone (B), clinical picture 3 weeks later showing a 10 × 5 mm area of exposed necrotic bone (C), specimen removed and submitted for histopathologic evaluation (D), photomicrograph H&E (×200) showing a non-vital bone (sequestrum) with bacterial colonies (E), and a clinical picture of the healed area at 2 month follow-up examination (F).
The clinical findings of bone exposure of the jaw with histopathologic diagnosis of sequestrum with actinomyces and neutrophils are similar to osteonecrosis of the jaw (ONJ) in patients treated with anti-resorptive or antiangiogenic agents. With no history of radiation therapy to the jaw or metastasis of the tumor to the jaw, this can be termed medication related osteonecrosis of the jaw (MRONJ) [1]. Since 2003, there has been an increase in ONJ cases related to anti-resorptive medications such as Alendronate (oral bisphosphonate), Pamidronate and Zolendronate (intravenous bisphosphonate), Denosumab (humanized monoclonal antibody) and anti-angiogenic medications such as Sunitinib (tyrosine kinase inhibitor) and Bevacizumab (humanized monoclonal antibody), which targets the vascular endothelial growth factor pathway [[2], [3], [4], [5], [6], [7]]. This patient had not used any of the aforementioned class of medications.
Ipilimumab was approved by the US Food and Drug Administration in March 2011 as an immunotherapy for the management of advanced (unresectable or metastatic) melanoma both in naïve or post-chemotherapy treated patients. Ipilimumab is a humanized monoclonal antibody against cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4). CTLA-4 is expressed in activated T-cells and in suppressor T-regulatory cells which bind to antigen presenting cells thereby lessening T-cell responses. Blocking the CTLA-4 increases the antitumor responses by activated T-cells. Ipilimumab has demonstrated clinical benefits in the management of melanoma [[8], [9]]. The adverse toxicities of Ipilimumab have been attributed to increased immune-reactivity against normal tissues causing pruritus, diarrhea, vitiligo, hepatitis, and endocrinopathies [10]. Bone necrosis was not reported. We suggest that Ipilimumab may have been involved in the process of bone necrosis in this patient. Ipilimumab increases systemic activated T-cells presence. CTLA4 deficient activated T-cells have been shown to be associated with osteonecrosis, as activated T-cells may elicit osteoclastogenesis via osteoprotegerin ligand resulting in bone loss [11]. Trauma from regular oral activity (chewing or tooth brushing) could increase the demand on this vulnerable bone to mend itself, resulting in localized bone necrosis.
To our knowledge, this is the first report of ONJ in a patient treated with Ipilimumab. Thousands of patients have been treated with Ipilimumab. If osteonecrosis is an associated complication, it is probably rare and maybe because patients are treated for a short time. As this is a relatively new medication with great promise for management of melanoma and other advanced-stage malignancy clinicians involved in the care of patients managed with Ipilimumab should be aware of this complication.
Acknowledgments
Funding: This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Disclosure: All authors declare that there are no financial conflicts associated with this report.
References
- 1.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2014;72:1938–56. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 2.Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2005;63:1567–75. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Estilo CL, Van Poznak CH, Wiliams T, Bohle GC, Lwin PT, Zhou Q, et al. Osteonecrosis of the maxilla and mandible in patients with advanced cancer treated with bisphosphonate therapy. The oncologist. 2008;13:911–20. doi: 10.1634/theoncologist.2008-0091. [DOI] [PubMed] [Google Scholar]
- 4.Estilo CL, Fornier M, Farooki A, Carlson D, Bohle G, 3rd, Huryn JM. Osteonecrosis of the jaw related to bevacizumab. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2008;26:4037–8. doi: 10.1200/JCO.2007.15.5424. [DOI] [PubMed] [Google Scholar]
- 5.Fleissig Y, Regev E, Lehman H. Sunitinib related osteonecrosis of jaw: a case report. Oral surgery, oral medicine, oral pathology and oral radiology. 2012;113:e1–3. doi: 10.1016/j.tripleo.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 6.Aghaloo TL, Felsenfeld AL, Tetradis S. Osteonecrosis of the jaw in a patient on Denosumab. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2010;68:959–63. doi: 10.1016/j.joms.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fusco V, Galassi C, Berruti A, Ciuffreda L, Ortega C, Ciccone G, et al. Osteonecrosis of the jaw after zoledronic acid and denosumab treatment. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29:e521–2. doi: 10.1200/JCO.2011.35.1551. author reply e3-4. [DOI] [PubMed] [Google Scholar]
- 8.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. The New England journal of medicine. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prieto PA, Yang JC, Sherry RM, Hughes MS, Kammula US, White DE, et al. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2012;18:2039–47. doi: 10.1158/1078-0432.CCR-11-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Graziani G, Tentori L, Navarra P. Ipilimumab: a novel immunostimulatory monoclonal antibody for the treatment of cancer. Pharmacological research : the official journal of the Italian Pharmacological Society. 2012;65:9–22. doi: 10.1016/j.phrs.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, et al. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature. 1999;402:304–9. doi: 10.1038/46303. [DOI] [PubMed] [Google Scholar]


