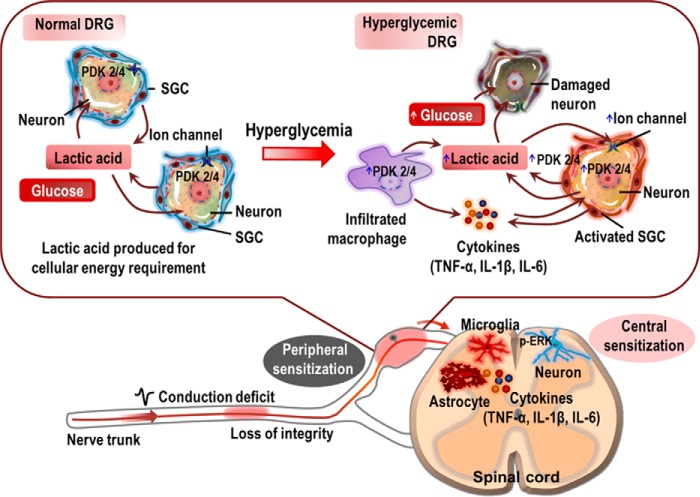
FIGURE 9.
A proposed schematic outlining the implications of PDK2/4 in the pathogenesis of painful diabetic neuropathy. Hyperglycemia induces the expression of PDK2/4 in DRG neurons, SGCs, and infiltrated macrophages. Glucose is thought to directly enhance the expression of the PDKs in DRG sensory neurons, besides exerting direct neurotoxic effects. Consequently, the hyperglycemia-induced heightened expression of the PDKs facilitates the conversion of pyruvate into lactic acid via inhibition of PDH. The infiltrated macrophages and reactive SGCs also participate in the production of lactic acid. The glycolytic metabolic shift in the DRG and ensuing production of lactic acid induces neuronal damage and lowers pH. The acidic microenvironment favors the enhanced expression of Trpv1 and Asic3 in the ganglionic sensory neurons, which causes neuronal hyperexcitability (peripheral sensitization). Furthermore, reactive SGCs and infiltrated macrophages in the DRG also release diverse proalgesic mediators, including inflammatory cytokines. The peripheral nerve trunk is also affected by hyperglycemia, contributing to the induction of peripheral sensitization. Finally, the glucose-PDK-PDH-lactic acid axis in the DRG induces central sensitization involving spinal glial activation, up-regulation of proinflammatory cytokines, and neuronal ERK phosphorylation. Thus, PDK2/4 up-regulation in the diabetic DRG plays a critical role in inducing peripheral as well as central sensitizations, eventually causing diabetic neuropathic pain.