Abstract
Background
Pooled data from two large registries, Cubicin® Outcomes Registry and Experience (CORE; USA) and European Cubicin® Outcomes Registry and Experience (EU-CORE; Europe, Latin America, and Asia), were analyzed to determine the characteristics and clinical outcomes of daptomycin therapy in patients with Gram-positive infections across wide geographical regions.
Methods
Patients receiving at least one dose of daptomycin between 2004 and 2012 for the treatment of Gram-positive infections were included. Clinical success was defined as an outcome of ‘cured’ or ‘improved’. Post-treatment follow-up data were collected for a subset of patients (CORE: osteomyelitis and orthopedic foreign body device infection; EU-CORE: endocarditis, intracardiac/intravascular device infection, osteomyelitis, and orthopedic device infection). Safety was assessed for up to 30 days after daptomycin treatment.
Results
In 11,557 patients (CORE, 5482; EU-CORE, 6075) treated with daptomycin (median age, 62 [range, 1–103] years), the most frequent underlying conditions were cardiovascular disease (54.7 %) and diabetes mellitus (28.0 %). The most commonly treated primary infections were complicated skin and soft tissue infection (cSSTI; 31.2 %) and bacteremia (21.8 %). The overall clinical success rate was 77.2 % (uncomplicated SSTI, 88.3 %; cSSTI, 81.0 %; osteomyelitis, 77.7 %; foreign body/prosthetic infection (FBPI), 75.9 %; endocarditis, 75.4 %; and bacteremia, 69.5 %). The clinical success rate was 79.1 % in patients with Staphylococcus aureus infections (MRSA, 78.1 %). An increasing trend of high-dose daptomycin (>6 mg/kg/day) prescribing pattern was observed over time. Clinical success rates were higher with high-dose daptomycin treatment for endocarditis and FBPI. Adverse events (AEs) and serious AEs possibly related to daptomycin therapy were reported in 628 (5.4 %) and 133 (1.2 %) patients, respectively.
Conclusions
The real-world data showed that daptomycin was effective and safe in the treatment of various Gram-positive infections, including those caused by resistant pathogens, across wide geographical regions.
Keywords: CORE, Daptomycin, Efficacy, EU-CORE, Gram-positive infections, High dose, MRSA, Real-world, Safety, Staphylococcus aureus
Background
Resistant Gram-positive pathogens such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) are associated with increased morbidity, mortality, and healthcare expenditures in hospitalized patients [1, 2]. Vancomycin is known to be an active agent for the treatment of Gram-positive infections, but there are concerns regarding its declining efficacy, potentially due to the “minimum inhibitory concentration creep” in MRSA [1, 3]. Therapeutic options such as clindamycin, co-trimoxazole, fluoroquinolones, minocycline, or the addition of rifampin may be useful, however, their use is limited to patients without life-threatening infections [4, 5]. Moreover, resistance to linezolid has been reported and its prolonged exposure can lead to myelosuppression [6, 7]. Other antibiotics with MRSA activity such as ceftaroline, ceftobiprole, telavancin, and tigecycline represent alternatives for the treatment of infections caused by drug-resistant Gram-positive pathogens [8]. However, there are some reports of safety issues associated with these antibiotics; hematological disorders and rash with ceftaroline, gastrointestinal upset with ceftobiprole, nephrotoxicity with telavancin, and pancreatitis with tigecycline [9–12].
Treatment choices are increasing for Gram-positive infections, including those caused by resistant pathogens. Various agents have either been recently approved (e.g. tedizolid, oritavancin) [8] or are under development, reflecting the need for “niche” antibiotics, particularly for difficult-to-treat infections [4, 13, 14].
Daptomycin is a cyclic lipopeptide with rapid bactericidal activity against a wide range of Gram-positive pathogens such as methicillin-susceptible S. aureus (MSSA), MRSA, and VRE [15, 16]. Daptomycin is approved in adult patients for the treatment of complicated skin and soft tissue infection (cSSTI; 4 mg/kg/day), right-sided infective endocarditis (RIE) due to S. aureus, and bacteremia associated with cSSTI or RIE (6 mg/kg/day) [17, 18]. However, high-dose (>6 mg/kg/day) daptomycin is often recommended for difficult-to-treat infections [14, 19–22]. Several study reports showed that high-dose daptomycin is increasingly used in patients with various deep seated infections and in those failing treatment with other antibiotics [23–26]. In addition to the approved indications, daptomycin has shown to be effective in the treatment of other infections, such as left-sided infective endocarditis (LIE), osteomyelitis, and orthopedic device infections [27–29]. Randomized controlled trials have shown a favorable safety and efficacy profile of daptomycin in patients with S. aureus bacteremia, endocarditis, and osteomyelitis/orthopedic device infections [30–32].
The Cubicin® Outcomes Registry and Experience (CORE) and the European Cubicin® Outcomes Registry and Experience (EU-CORE), both multicenter, retrospective, non-interventional registries, were conducted to collect real-world data on the characteristics and clinical outcomes of patients receiving daptomycin [33, 34]. CORE included data from approximately 164 sites in the United States of America (USA) [35–37], whereas EU-CORE comprised data from 310 sites across 18 countries in Europe (12), Latin America (5), and Asia (1). Various independent reports on the results from CORE (2004–2009) and EU-CORE (2006–2012) have been published [33–36, 38]. The results of CORE and EU-CORE showed that daptomycin is also used for treating infections other than those approved [35, 39]. Combining data from two real-world registries conducted in different regions may help in understanding the trend of prescribing patterns and duration of treatment versus effectiveness and safety in a large number of patients treated with daptomycin between 2004 and 2012.
Methods
Patients and data collection
The protocols were approved by the health authority and the Institutional Review Board (IRB) or Ethics Committee (EC) of each participating country. The methodologies have been published previously [36, 40]. Written informed consent was obtained from patients according to the requirements of the IRB or EC and/or the local data privacy regulations. Patients who had received at least one dose of daptomycin between January 2004 and April 2012 for treatment of Gram-positive bacterial infections were included. Patients should have been followed up for 30 days after treatment. Patients who had received daptomycin as part of a controlled clinical trial were not eligible. In CORE, patients with osteomyelitis or orthopedic foreign body device infection (enrolled between 2007 and 2008) were evaluated at the end of daptomycin treatment; those with at least one post-treatment follow-up assessment were also included in the follow-up data collection up to 2009. In EU-CORE, patients with endocarditis, intracardiac/intravascular device infection, osteomyelitis, or orthopedic device infection were followed for up to 2 years from 2012 to 2014. In both registries, the overlapping data collection period was from 2007 to 2009. Demographic, antibiotic, microbiologic, and clinical data were recorded retrospectively using standardized case report forms as per the protocols. This analysis extracted data from all patients who received daptomycin from 2004 to 2012 (CORE, 2004–2009; EU-CORE, 2006–2012).
Definitions
Clinical outcomes were assessed by investigators at the end of daptomycin treatment based on the following protocol-defined criteria: cured, clinical signs and symptoms resolved, no additional antibiotic therapy was necessary, or infection cleared with a negative culture reported; improved, partial resolution of clinical signs and symptoms and/or additional antibiotic therapy was warranted; failed, inadequate response to daptomycin therapy, worsening or new/recurrent signs and symptoms, need for a change in antibiotic therapy, or a positive culture reported at the end of the therapy; and non-evaluable, unable to determine response due to insufficient information. Clinical success was defined as an outcome of ‘cured’ or ‘improved’. Time to improvement was recorded. The reasons for discontinuation of daptomycin therapy and details of other antibiotics prescribed concomitantly or following daptomycin were also recorded. Among all registry-enrolled patients, the safety population comprised patients for whom any safety parameters were assessed, and the efficacy population comprised patients for whom clinical outcomes were assessed. All adverse events (AEs) were reported, regardless of their relationship to daptomycin; the severity of these AEs was determined by the investigators.
Statistical analysis
Statistical analysis was performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA). Due to the nature of the two observational uncontrolled registry trials, inferential analyses were not conducted and no formal statistical methodology, except simple descriptive statistics, was used. All analyses were considered to be explanatory. Numerical variables were summarized as arithmetic mean, standard deviation, median, minimum, first quartile, third quartile, and maximum for the continuous variables, whereas the categorical variables were summarized according to absolute and relative frequencies.
Logistic regression analysis was performed to assess risk factors for CPK elevation, with CPK elevation (yes/no) as response variable and the following variables as covariates: age, use of statin therapy, history of renal disease or diabetes mellitus, significant underlying disease, infection type, initial dose level, surgical procedure, concomitant use of antibiotics, creatinine clearance (CrCl), and baseline CPK.
Results
Patient demographics and clinical characteristics
A total of 11,557 patients (CORE, 5482; EU-CORE, 6075) treated with daptomycin were included in this analysis. Baseline patient demographic and clinical characteristics by overall pooled data and individual studies during the overlapping period from 2007 to 2009, are summarized in Table 1. The median age of the patients was 62 (range, 1–103) years, with 38.4 % aged ≥65 years, and a majority (88.7 %) having significant underlying diseases. The most common underlying conditions were cardiovascular disease (54.7 %) and diabetes mellitus (28.0 %), followed by malignancy (16.7 %) and renal disease (16.6 %). Daptomycin was used to treat a wide range of primary infections (Table 2). The commonly treated primary infections were cSSTI (31.2 %), bacteremia (21.8 %), foreign body/prosthetic infection (FBPI; 8.5 %), osteomyelitis (8.6 %), and endocarditis (6.9 %; including 3.9 % with LIE). The most common secondary infections were bacteremia (3.8 %), cSSTI (2.6 %), osteomyelitis (1.7 %), and endocarditis (1.2 %). Overall, 14.5 % of patients had renal impairment (CrCl <30 mL/min) and 1095 (9.5 %) patients were on dialysis at the time of initiation of daptomycin therapy.
Table 1.
Baseline patient demographic and clinical characteristics
| Characteristic | Pooled data (2004–2012) N = 11,557 n (%) |
Overlapping time period (2007–2009) | |
|---|---|---|---|
| COREa | EU-COREa | ||
| N = 2827 n (%) |
N = 3333 n (%) |
||
| Male | 6587 (57.0) | 1454 (51.4) | 2150 (64.5) |
| Ageb (years), median (range) | 62.0 (1–103) | 56.5 (4–99) | 63.0 (1–103) |
| <65 years | 7111 (61.5) | 1945 (68.8) | 1758 (52.7) |
| ≥65 years | 4441 (38.4) | 882 (31.2) | 1572 (47.2) |
| ≥75 years | 1732 (15.0) | 265 (9.4) | 734 (22.0) |
| Body weight (kg), median (range) | 78.0 (6–275) | 81.9 (15–259) | 75.0 (6–200) |
| Race, Caucasian | 7191 (62.2) | 1967 (69.6) | 3058 (91.7) |
| Setting prior to daptomycin therapyc | |||
| Hospital | 7278 (63.0) | 1359 (49.3) | 2558 (76.7) |
| Nursing home/extended care | 431 (3.7) | 152 (5.4) | 102 (3.1) |
| Community | 3772 (32.6) | 1275 (45.1) | 637 (19.1) |
| Other | 57 (0.5) | 5 (0.2) | 24 (0.7) |
Data are presented as n (%), unless indicated otherwise
aData are from three overlapping periods: 2007–2009
bData missing for 5 patients
cData missing for 19 patients
Table 2.
Primary infections and pathogens
| Primary infection | Pooled data (2004–2012) N = 11,557 n (%) |
Overlapping time period (2007–2009) | |
|---|---|---|---|
| COREa | EU-COREa | ||
| N = 2827 n (%) |
N = 3333 n (%) |
||
| Complicated skin and soft tissue infection | 3607 (31.2) | 803 (28.4) | 1092 (32.8) |
| Bacteremia | 2522 (21.8) | 642 (22.7) | 741 (22.2) |
| Endocarditis | 798 (6.9) | 103 (3.6) | 338 (10.1) |
| Foreign body/prosthetic infection | 988 (8.5) | 217 (7.7) | 294 (8.8) |
| Osteomyelitis (non-prosthetic and prosthetic device-related) | 994 (8.6) | 281 (9.9) | 193 (5.8) |
| Uncomplicated skin and soft tissue infection | 1510 (13.1) | 475 (16.8) | 334 (10.0) |
| Otherb | 1138 (9.8) | 306 (10.8) | 341 (10.2) |
| Primary pathogen | Pooled data (2004–2012) N = 7912 n (%) |
Overlapping time period (2007–2009) | |
|---|---|---|---|
| COREa | EU-COREa | ||
| Positive culturec | N = 2002 n (%) |
N = 2240 n (%) |
|
| Staphylococcus aureus | 3673 (46.4) | 925 (46.2) | 931 (41.6) |
| Methicillin-susceptible | 1104 (14.0) | 208 (10.4) | 356 (15.9) |
| Methicillin-resistant | 2261 (28.6) | 621 (31.0) | 509 (22.7) |
| Susceptibility unknown | 308 (3.9) | 96 (4.8) | 66 (2.9) |
| CoNS | 1690 (21.4) | 276 (13.8) | 677 (30.2) |
| Staphylococcus epidermidis | 850 (10.7) | 103 (5.1) | 390 (17.4) |
| Staphylococcus spp.–coagulase negative | 840 (10.6) | 173 (8.6) | 287 (12.8) |
| Enterococci | 1380 (17.4) | 495 (24.7) | 255 (11.4) |
| Vancomycin-resistant | 576 (7.2) | 284 (14.2) | 36 (1.0) |
| Enterococcus faecalis | 492 (6.2) | 134 (6.7) | 125 (5.6) |
| Vancomycin-resistant | 83 (1.0) | 37 (0.5) | 10 (0.3) |
| Enterococcus faecium | 684 (8.6) | 277 (13.8) | 110 (4.9) |
| Vancomycin-resistant | 493 (6.2) | 247 (12.3) | 26 (0.8) |
| Enterococcus spp. | 204 (2.6) | 84 (4.2) | 20 (0.9) |
| Streptococci | 326 (4.1) | 71 (3.5) | 98 (4.4) |
| Otherd | 843 (10.7) | 235 (11.7) | 279 (12.5) |
CoNS coagulase-negative staphylococci
aData are from three overlapping periods: 2007–2009
bIncludes septic arthritis, urinary tract infections/pyelonephritis, central nervous system infections, metastatic abscess, antibiotic prophylaxis (surgical and non-surgical), neutropenic fever, necrotizing fasciitis, necrotizing infections, unknown or not otherwise specified infections, and data missing
cPercentage is calculated based on positive culture results
dIncludes Clostridium difficile, Clostridium perfringens, Clostridium species, Corynebacterium species, Staphylococcus species coagulase not specified, Gram-positive and Gram-negative bacilli and cocci, Leuconostoc species, Peptococcus species, Peptostreptococcus species, fungi/yeast, viruses, and organisms with invalid/ambiguous pathogen code
Microbiology
Culture results were available for a total of 9664 (83.6 %) patients, of whom 7912 (81.9 %) had positive culture results and 1752 (18.1 %) had negative culture results (Table 2). The most frequently isolated pathogens in patients with positive culture results were S. aureus (46.4 %, including 28.6 % MRSA and 14.0 % MSSA), coagulase-negative staphylococci (CoNS; 21.4 %), and enterococci (17.4 %; VRE, 7.3 %).
Previous and concomitant therapies
The majority of patients (n = 8221; 71.1 %) received prior antibiotic therapy, most commonly glycopeptides (34.3 %; vancomycin, 30.6 %; teicoplanin, 4.2 %), penicillins (19.5 %), cephalosporins (15.6 %), and fluoroquinolones (13.9 %). The most common reasons for switching to daptomycin included failure of prior antibiotic therapy (28.0 %), resistant or non-susceptible Gram-positive organism (10.7 %), and narrow antibiotic spectrum (10.0 %). Daptomycin was used concomitantly with other antibiotics in 6631 (57.4 %) patients who received treatment in an inpatient setting; the frequently administered concomitant antibiotics were carbapenems (17.6 %), penicillins (12.1 %), fluoroquinolones (11.5 %), and cephalosporins (10.0 %).
Daptomycin prescribing patterns
The most commonly prescribed dose of daptomycin was 6 mg/kg/day (n = 4968; 43.0 %), followed by 4 mg/kg/day (n = 3469; 30.0 %). A similar daptomycin prescribing pattern was noted in the overlapping period of CORE (6 mg/kg/day [48.5 %], followed by 4 mg/kg/day [26.6 %]) and EU-CORE (6 mg/kg/day [45.5 %], followed by 4 mg/kg/day [29.9 %]). In particular, 54.2 % of patients with bacteremia and 42.0 % patients with cSSTI were treated with daptomycin 6 mg/kg/day and 4 mg/kg/day, respectively. A total of 1564 (13.5 %) patients received high-dose daptomycin (>6 mg/kg/day). A trend toward use of higher doses (>6 mg/kg/day) over time was observed for most of the infections, particularly in patients with bacteremia, osteomyelitis, and FBPI (Fig. 1).
Fig. 1.
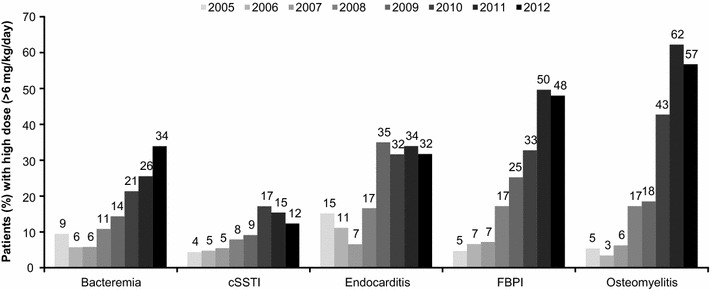
Prescribing pattern of high-dose daptomycin over time. cSSTI complicated skin and soft tissue infection, FBPI foreign body/prosthetic infection
Overall, the median duration of treatment with daptomycin was 12.0 (range, 1–370) days; 8.0 (range, 1–246) days in the inpatient setting and 16.0 (range, 1–358) days in the outpatient setting. The mean duration of daptomycin treatment according to inpatient/outpatient treatment settings over time (years) is shown in Fig. 2. The duration of treatment was lower in inpatients compared with outpatients. Among the key primary infections, the median inpatient treatment duration was longest for endocarditis at 16.0 (range, 1–112) days and shortest for uncomplicated SSTI (uSSTI) at 6.0 (range, 1–56) days. The mean durations of daptomycin treatment by primary infection over time are shown in Fig. 3. The duration of treatment was higher for endocarditis, FBPI, and osteomyelitis as compared with uSSTI, cSSTI, and bacteremia. An increasing trend was observed in mean duration of treatment for osteomyelitis, FBPI, and endocarditis over time.
Fig. 2.
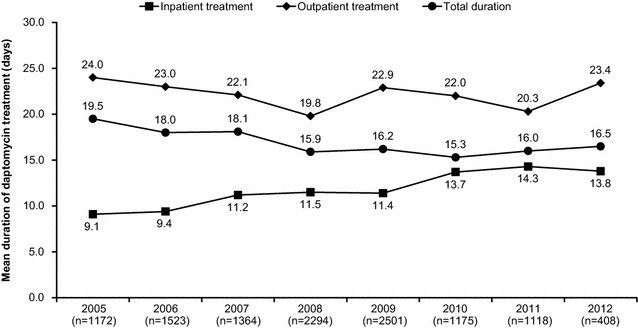
Mean durations of daptomycin treatment according to inpatient and outpatient treatment settings over time (2005–2012)
Fig. 3.
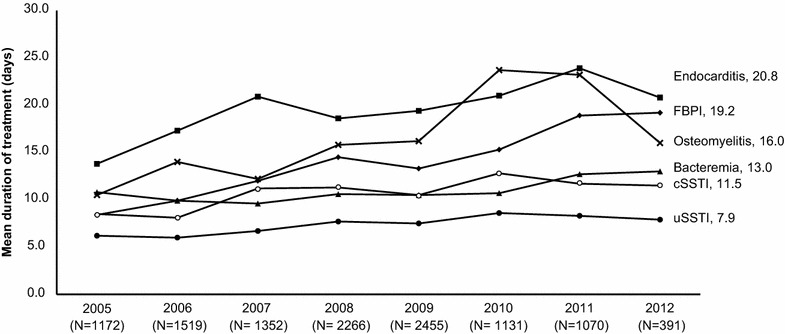
Mean durations of daptomycin treatment by primary infection over time (2005–2012). cSSTI complicated skin and soft tissue infection, FBPI foreign body/prosthetic infection
A total of 6471 (56.0 %) patients completed the daptomycin treatment; however, 23.4 % switched therapy (e.g., stepped-down to oral antibiotic therapy). Discontinuation of daptomycin therapy due to AEs and treatment failure was reported in 4.6 and 3.3 % of patients, respectively.
Clinical outcomes
An overall clinical success rate of 77.2 % was reported with daptomycin therapy. The clinical success rates ranged from 69.5 % for bacteremia to 88.3 % for uSSTI (Fig. 4). The clinical success rates during the overlapping period (2007–2009) were similar overall and for the different primary infections. The success rates in patients with resistant pathogens such as MRSA and VRE were 78.1 and 68.8 %, respectively (Fig. 5).
Fig. 4.
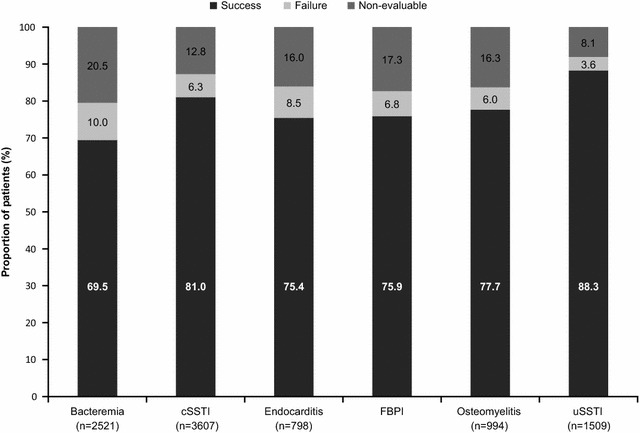
Clinical outcomes by primary infection. cSSTI complicated skin and soft tissue infection, FBPI foreign body/prosthetic infection, uSSTI uncomplicated skin and soft tissue infection
Fig. 5.
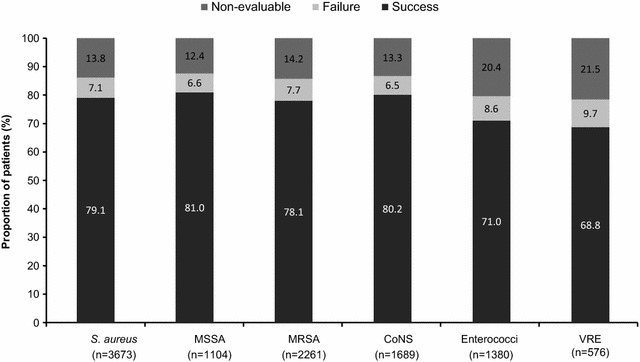
Clinical outcomes by primary pathogen. CoNS coagulase-negative staphylococci, MRSA methicillin-resistant S. aureus, MSSA methicillin-susceptible S. aureus, VRE vancomycin-resistant enterococci
The clinical success rate was slightly higher (80.3 %) when daptomycin was used as a first-line than that when used as a second-line therapy (75.9 %). For infections associated with MRSA as the primary pathogen, the clinical success rate with first-line daptomycin treatment (n = 841) was 83.7 % compared with 76.3 % with second-line daptomycin treatment (n = 2819). Clinical success rates tended to be higher with increasing daptomycin doses for endocarditis and FBPI (Fig. 6).
Fig. 6.
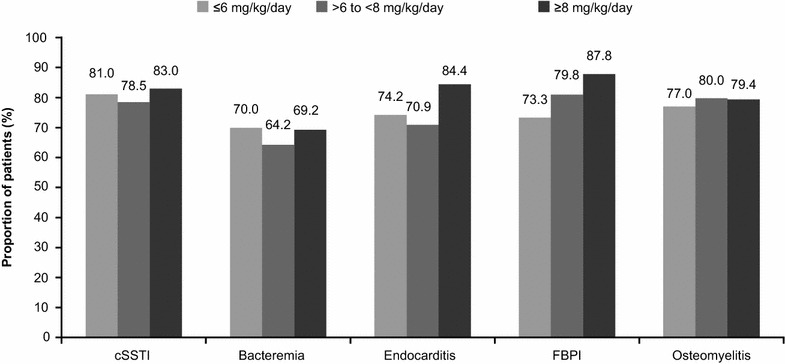
Clinical success rates for primary infection by daptomycin dose. cSSTI complicated skin and soft tissue infection, FBPI foreign body/prosthetic infection
The patients who received daptomycin as monotherapy reported higher (82.7 %) clinical success rates than those who received concomitant antibiotic therapy (74.3 %).
Safety
Daptomycin was generally well tolerated. AEs, regardless of their relationship to daptomycin treatment, were reported in 1879 (16.3 %) patients, and serious AEs (SAEs) were reported in 1050 (9.1 %) patients. Increased blood creatine phosphokinase (CPK; 1.9 %), multi-organ failure (1.0 %), and sepsis (1.0 %) were the most commonly reported AEs regardless of relationship to daptomycin treatment, and the most common SAEs were multi-organ failure (1.0 %), sepsis (1.0 %), and septic shock (0.7 %). AEs and SAEs possibly related to daptomycin treatment were reported in 628 (5.4 %) and 133 (1.2 %) patients, respectively. Elevated blood CPK levels in 175 (1.5 %) patients, myalgia in 21 (0.2 %) patients, rhabdomyolysis in 12 (0.1 %) patients, and both myopathy and eosinophilic pneumonia in 4 (0.03 %) patients each were reported as AEs possibly related to daptomycin treatment.
Blood CPK levels at baseline were measured in 4206 (36.4 %) patients. Of these, the majority (n = 3503; 83.3 %) had CPK levels ≤1 × upper limit of normal (ULN), 72 (1.7 %) had levels >5–10 × ULN, and 115 (2.7 %) had levels >10 × ULN. Blood CPK levels during daptomycin therapy were measured in 5024 (43.5 %) patients; of those, 3794 (75.5 %) had CPK levels ≤1 × ULN, 126 (2.5 %) had levels >5–10 × ULN, and 166 (3.3 %) had levels >10 × ULN.
Results of the logistic regression analysis to assess risk factors for CPK elevation showed that factors such as age, initial daptomycin dose and CrCl were not statistically significant at 5 % level of significance; however, surgical intervention and concomitant antibiotic therapy were found to be statistically significant at 5 % level of significance (Fig. 7). A total of 57 (1.7 %) patients experienced a shift of CPK elevation from ≤10 × ULN at baseline to >10 × ULN. AEs leading to study drug discontinuation occurred in 519 (4.5 %) patients, most frequently due to infections and infestations (1.0 %) including sepsis (0.3 %) and septic shock (0.3 %). A total of 674 (5.8 %) patients died during the daptomycin treatment; the most frequent causes of death were sepsis (0.9 %) and septic shock (0.7 %).
Fig. 7.
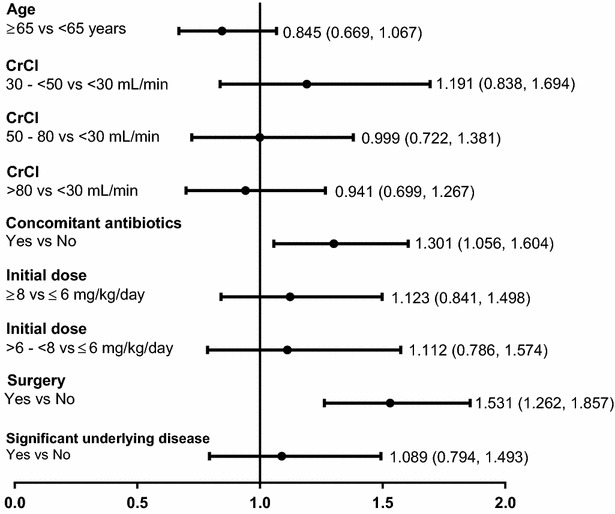
Logistic regression analysis of CPK elevation versus risk factors. Data are presented as odds ratio and 95 % confidence interval. CrCl creatinine clearance
Discussion
The CORE and EU-CORE pooled data analysis reflects the clinical experience with daptomycin use in a real-world setting. The results suggest that daptomycin is widely used to treat various infections caused by Gram-positive bacteria, including resistant strains (MRSA, CoNS, and VRE), in a complex patient population with multiple co-morbidities across the USA, Europe, Latin America, and Asia. Daptomycin demonstrated good safety and effectiveness outcomes, when used as second- or first-line therapy. Daptomycin was used to treat the approved indications (cSSTI, bacteremia, and RIE). In addition, patients with LIE, osteomyelitis, prosthetic joint infections, neutropenic fever, sepsis of unknown origin, and surgical site infections caused by Gram-positive pathogens were also treated, which reflects an unmet medical need of approved treatment options for these conditions. Several reports have suggested that daptomycin is effective and has an overall good safety profile in various clinical conditions such as SSTI, bacteremia, osteomyelitis and endocarditis in different geographical regions [15, 29, 41–43]. Rege et al. have reported good tolerability and high clinical success rates with daptomycin when administered for >14 days, in a patient population from the USA [34]. Similarly, the results from an 8-year clinical experience with daptomycin showed favorable safety and effectiveness profiles with lower overall clinical failure rates in Europe, Latin America, and Asia [33, 40, 43]. These results complement the previously published data from randomized clinical trials [31, 32]. Treatment with daptomycin in the real-world setting showed high clinical success rates across a range of pathogens, both for labeled (cSSTI, bacteremia, and RIE), and non-labeled (osteomyelitis, FBPI, and LIE) infections. High success rates with daptomycin treatment were observed irrespective of first-line or second-line use. In patients with MRSA infections, the clinical success rates were numerically higher with first-line (83.7 %) compared with second-line (76.3 %) daptomycin treatment. Increased use of first-line daptomycin treatment for suspected and confirmed resistant pathogens, such as MRSA, reflects increasing awareness of daptomycin use for resistant pathogens and the limitations of available treatment options [31, 32, 44]. This pooled analysis reinforces the data from the previously published real-world reports (CORE and EU-CORE) [33, 35].
Considering the linear pharmacokinetics and dose-dependent bactericidal activity of daptomycin [45], high dose (>6 mg/kg/day) is sometimes recommended to minimize the risk of resistance development in patients with difficult-to-treat infections including those caused by resistant pathogens (MRSA and VRE) [45–47]. Daptomycin has a long half-life of 8 h, and demonstrates a prolonged post-antibiotic effect of up to 6.8 h. It is highly bound to serum proteins (90 %) and is distributed primarily in the extracellular fluid. It effectively penetrates bone and inflamed soft tissues and, therefore, is efficacious in the treatment of deep tissue infections [18, 48].
A number of national and international guidelines recommend high-dose daptomycin (>6 mg/kg/day) as a possible therapeutic alternative for difficult-to-treat infections [20, 21, 49, 50]. In combination with other antibiotics, daptomycin (10 mg/kg/day) is also recommended for persistent MRSA bacteremia and vancomycin treatment failures [19, 20, 49, 51].
A study including 70 patients with IE receiving high-dose daptomycin (≥8 mg/kg/day) has shown successful clinical outcomes in all patients without any reports of discontinuation due to toxicity or AEs [52]. In a larger study of 250 patients with complicated Gram-positive infections, high-dose daptomycin (8 mg/kg/day) was reported to be effective and have a favorable safety profile [52]. Furthermore, various studies demonstrated that high-dose daptomycin is effective and well tolerated in the treatment of difficult-to-treat infections such as LIE, mediastinitis after cardiac surgery, and osteomyelitis [7, 52]. The results from the current analysis showed a trend toward the use of higher doses (>6 mg/kg/day) over time with high success rates for endocarditis and FBPI, which is also supported by previously published literature [7, 49, 52].
It is well recognized that daptomycin treatment is associated with blood CPK elevation, however, no significant correlation was reported between daptomycin dose and blood CPK elevation [14, 53, 54]. In the present analysis, a small proportion of patients experienced elevation in blood CPK levels; however, this was not always associated with adverse musculoskeletal effects. There was no correlation observed between blood CPK elevation and factors such as age, initial daptomycin dose, or CrCl. Furthermore, no new or unexpected safety findings were observed in this analysis. These safety results are consistent with earlier published real-world reports from the USA and Europe [34, 41, 55].
The registries have inherent limitations, such as the retrospective nature of the data collection and non-comparative, non-blinded, and non-randomized design. However, the registries allow the inclusion of diverse infections and the use of concomitant antibiotics, including broad-spectrum antibiotics. Therefore, the results mimic real-world clinical experience with daptomycin and expand the evidence derived from clinical trials.
The present analysis re-affirms the real-world safety and effectiveness of daptomycin across wide geographical regions including the USA and Europe. The data suggest that daptomycin is effective and well tolerated for the management of difficult-to-treat infections caused by various Gram-positive pathogens, including those caused by resistant species (MSSA, MRSA, CoNS, and VRE). Moreover, a trend of increased use of high-dose daptomycin was noted over time, specifically in patients with endocarditis, osteomyelitis, and prosthetic joint infections.
Authors’ contributions
All authors were involved in data interpretation, defining the content for the manuscript and critically reviewing it. RAS, AGR, KOC, and KAC were involved in data collection, while RP and KH conducted the data analysis. KH was involved in writing the manuscript. All of the authors had full access to data in the study, discussed the results, reviewed the draft manuscript and agreed on the final version. KH, the corresponding author, had final responsibility for the decision to submit the manuscript for publication. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge the work of the CORE and EU-CORE investigators, Kenneth Lamp (previous medical director, CORE) and Uwe Trostmann (previous clinical scientist, EU-CORE). Medical writing support was provided by Anupama Tamta (Novartis Healthcare Pvt. Ltd., Hyderabad, India). At all stages, the authors had control over the content of this manuscript, for which they have given final approval and take full responsibility.
Competing interests
RAS received consultancy fees and honoraria for speaking at Novartis sponsored symposia. AGR received fees from Novartis, Pfizer, Cubist, and Gilead for staff training, being member of Advisory Boards, and being member of speakers panels. He also received support from Novartis to attend scientific conferences including accommodation and travel payments, and a grant to support his research. KOC was involved in speakers’ bureau for Cubist Pharmaceuticals and Merck and received research funding from Cubist Pharmaceuticals. KAC received honoraria from Cubist Pharmaceuticals, Merck, ProCE, and Simon and Shuster. RP is an employee of Novartis Healthcare Pvt. Ltd. KH is an employee of Novartis Pharmaceuticals Corporation.
Funding
CORE was funded by Cubist Pharmaceuticals and EU-CORE by Novartis Pharma AG.
Contributor Information
R. Andrew Seaton, Email: andrew.seaton@ggc.scot.nhs.uk.
Armando Gonzalez-Ruiz, Email: armando.gonzalez@nhs.net.
Kerry O. Cleveland, Email: kclevel1@uthsc.edu
Kimberly A. Couch, Email: kim_couch@yahoo.com
Rashidkhan Pathan, Email: rashidkhan.pathan@novartis.com.
Kamal Hamed, Email: kamal.hamed@novartis.com.
References
- 1.Rivera AM, Boucher HW. Current concepts in antimicrobial therapy against select gram-positive organisms: methicillin-resistant Staphylococcus aureus, penicillin-resistant pneumococci, and vancomycin-resistant enterococci. Mayo Clin Proc. 2011;86(12):1230–1243. doi: 10.4065/mcp.2011.0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sievert DM, Rudrik JT, Patel JB, McDonald LC, Wilkins MJ, Hageman JC. Vancomycin-resistant Staphylococcus aureus in the United States, 2002–2006. Clin Infect Dis. 2008;46(5):668–674. doi: 10.1086/527392. [DOI] [PubMed] [Google Scholar]
- 3.Joana S, Pedro P, Elsa G, Filomena M. Is vancomycin MIC creep a worldwide phenomenon? assessment of S. aureus vancomycin MIC in a tertiary university hospital. BMC Res Notes. 2013;6:65. doi: 10.1186/1756-0500-6-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dryden M, Andrasevic AT, Bassetti M, Bouza E, Chastre J, Cornaglia G, et al. A European survey of antibiotic management of methicillin-resistant Staphylococcus aureus infection: current clinical opinion and practice. Clin Microbiol Infect. 2010;16(Suppl 1):3–30. doi: 10.1111/j.1469-0691.2010.03135.x. [DOI] [PubMed] [Google Scholar]
- 5.Leekha S, Terrell CL, Edson RS. General principles of antimicrobial therapy. Mayo Clin Proc. 2011;86(2):156–167. doi: 10.4065/mcp.2010.0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caballero JD, Pastor MD, Vindel A, Maiz L, Yague G, Salvador C, et al. Emergence of cfr-mediated linezolid resistance in a methicillin-resistant Staphylococcus aureus epidemic clone isolated from patients with cystic fibrosis. Antimicrob Agents Chemother. 2015; pii: AAC.02067-15. [DOI] [PMC free article] [PubMed]
- 7.Casapao AM, Kullar R, Davis SL, Levine DP, Zhao JJ, Potoski BA, et al. Multicenter study of high-dose daptomycin for treatment of enterococcal infections. Antimicrob Agents Chemother. 2013;57(9):4190–4196. doi: 10.1128/AAC.00526-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bassetti M, Righi E. Safety profiles of old and new antimicrobials for the treatment of MRSA infections. Expert Opin Drug Saf. 2016;6:1–15. doi: 10.1517/14740338.2016.1142528. [DOI] [PubMed] [Google Scholar]
- 9.Jain R, Chan JD, Rogers L, Dellit TH, Lynch JB, Pottinger PS. High incidence of discontinuations due to adverse events in patients treated with ceftaroline. Pharmacotherapy. 2014;34(7):758–763. doi: 10.1002/phar.1435. [DOI] [PubMed] [Google Scholar]
- 10.Polyzos KA, Mavros MN, Vardakas KZ, Makris MC, Rafailidis PI, Falagas ME. Efficacy and safety of telavancin in clinical trials: a systematic review and meta-analysis. PLoS ONE. 2012;7(8):e41870. doi: 10.1371/journal.pone.0041870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noel GJ, Bush K, Bagchi P, Ianus J, Strauss RS. A randomized, double-blind trial comparing ceftobiprole medocaril with vancomycin plus ceftazidime for the treatment of patients with complicated skin and skin-structure infections. Clin Infect Dis. 2008;46(5):647–655. doi: 10.1086/526527. [DOI] [PubMed] [Google Scholar]
- 12.Okon E, Engell C, van Manen R, Brown J. Tigecycline-related pancreatitis: a review of spontaneous adverse event reports. Pharmacotherapy. 2013;33(1):63–68. doi: 10.1002/phar.1159. [DOI] [PubMed] [Google Scholar]
- 13.David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23(3):616–687. doi: 10.1128/CMR.00081-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kullar R, Sakoulas G, Deresinski S, van Hal SJ. When sepsis persists: a review of MRSA bacteraemia salvage therapy. J Antimicrob Chemother. 2015;71(3):576–586. doi: 10.1093/jac/dkv368. [DOI] [PubMed] [Google Scholar]
- 15.Dohmen PM, Guleri A, Capone A, Utili R, Seaton RA, Gonzalez-Ramallo VJ, et al. Daptomycin for the treatment of infective endocarditis: results from a European registry. J Antimicrob Chemother. 2013;68(4):936–942. doi: 10.1093/jac/dks467. [DOI] [PubMed] [Google Scholar]
- 16.Livermore DM. Future directions with daptomycin. J Antimicrob Chemother. 2008;62(Suppl 3):iii41–iii49. doi: 10.1093/jac/dkn371. [DOI] [PubMed] [Google Scholar]
- 17.Malizos K, Sarma J, Seaton RA, Militz M, Menichetti F, Riccio G, et al. Daptomycin for the treatment of osteomyelitis and orthopaedic device infections: real-world clinical experience from a European registry. Eur J Clin Microbiol Infect Dis. 2015;35(1):111–118. doi: 10.1007/s10096-015-2515-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Traunmuller F, Schintler MV, Metzler J, Spendel S, Mauric O, Popovic M, et al. Soft tissue and bone penetration abilities of daptomycin in diabetic patients with bacterial foot infections. J Antimicrob Chemother. 2010;65(6):1252–1257. doi: 10.1093/jac/dkq109. [DOI] [PubMed] [Google Scholar]
- 19.Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015;36(44):3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 20.Gudiol F, Aguado JM, Almirante B, Bouza E, Cercenado E, Dominguez MA, et al. Executive summary of the diagnosis and treatment of bacteremia and endocarditis due to Staphylococcus aureus. A clinical guideline from the Spanish Society of Clinical Microbiology and Infectious Diseases (SEIMC) Enferm Infecc Microbiol Clin. 2015;33(9):626–632. doi: 10.1016/j.eimc.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52(3):285–292. doi: 10.1093/cid/cir034. [DOI] [PubMed] [Google Scholar]
- 22.Perrottet N, Steinrucken J, Chan M, Pannatier A, Borens O, Yusuf E, et al. Efficacy and safety of high-dose daptomycin (>6 mg/kg) for complicated bone and joint infections and implant-associated infections caused by gram-positive bacteria. Int J Antimicrob Agents. 2015;46(4):480–482. doi: 10.1016/j.ijantimicag.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Lai CC, Sheng WH, Wang JT, Cheng A, Chuang YC, Chen YC, et al. Safety and efficacy of high-dose daptomycin as salvage therapy for severe gram-positive bacterial sepsis in hospitalized adult patients. BMC Infect Dis. 2013;13:66. doi: 10.1186/1471-2334-13-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Legout L, D’Elia P, Sarraz-Bournet B, Ettahar N, Haulon S, Leroy O, et al. Tolerability of high doses of daptomycin in the treatment of prosthetic vascular graft infection: a retrospective study. Infect Dis Ther. 2014;3(2):215–223. doi: 10.1007/s40121-014-0035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moise PA, Hershberger E, Amodio-Groton MI, Lamp KC. Safety and clinical outcomes when utilizing high-dose (>or = 8 mg/kg) daptomycin therapy. Ann Pharmacother. 2009;43(7):1211–1219. doi: 10.1345/aph.1M085. [DOI] [PubMed] [Google Scholar]
- 26.Parra-Ruiz J, Hernandez-Quero J. Safety and efficacy of daptomycin therapy in older adults with pluripathology. Enferm Infecc Microbiol Clin. 2012;30(Suppl 1):50–53. doi: 10.1016/S0213-005X(12)70072-1. [DOI] [PubMed] [Google Scholar]
- 27.Beiras-Fernandez A, Vogt F, Sodian R, Weis F. Daptomycin: a novel lipopeptide antibiotic against gram-positive pathogens. Infect Drug Resist. 2010;3:95–101. doi: 10.2147/IDR.S6961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guleri A, Utili R, Dohmen P, Petrosillo N, Piper C, Pathan R, et al. Daptomycin for the treatment of infective endocarditis: results from European cubicin((R)) outcomes registry and experience (EU-CORE) Infect Dis Ther. 2015;4(3):283–296. doi: 10.1007/s40121-015-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seaton RA, Malizos KN, Viale P, Gargalianos-Kakolyris P, Santantonio T, Petrelli E, et al. Daptomycin use in patients with osteomyelitis: a preliminary report from the EU-CORE(SM) database. J Antimicrob Chemother. 2013;68(7):1642–1649. doi: 10.1093/jac/dkt067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Byren I, Rege S, Campanaro E, Yankelev S, Anastasiou D, Kuropatkin G, et al. Randomized controlled trial of the safety and efficacy of daptomycin versus standard-of-care therapy for management of patients with osteomyelitis associated with prosthetic devices undergoing two-stage revision arthroplasty. Antimicrob Agents Chemother. 2012;56(11):5626–5632. doi: 10.1128/AAC.00038-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fowler VG, Jr, Boucher HW, Corey GR, Abrutyn E, Karchmer AW, Rupp ME, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006;355(7):653–665. doi: 10.1056/NEJMoa053783. [DOI] [PubMed] [Google Scholar]
- 32.Konychev A, Heep M, Moritz RK, Kreuter A, Shulutko A, Fierlbeck G, et al. Safety and efficacy of daptomycin as first-line treatment for complicated skin and soft tissue infections in elderly patients: an open-label, multicentre, randomized phase IIIb trial. Drugs Aging. 2013;30(10):829–836. doi: 10.1007/s40266-013-0114-8. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez-Ruiz A, Gargalianos-Kakolyris P, Timerman A, Sarma J, Jose Gonzalez Ramallo V, Bouylout K, et al. Daptomycin in the clinical setting: 8-year experience with gram-positive bacterial infections from the EU-CORE(SM) registry. Adv Ther. 2015;32(6):496–509. doi: 10.1007/s12325-015-0220-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rege S, Mohr J, Lamp KC, Yoon M, Lindfield KC. Safety of daptomycin in patients completing more than 14 days of therapy: results from the cubicin(R) outcomes registry and experience. Int J Antimicrob Agents. 2013;41(5):421–425. doi: 10.1016/j.ijantimicag.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 35.Rolston KV, Besece D, Lamp KC, Yoon M, McConnell SA, White P. Daptomycin use in neutropenic patients with documented gram-positive infections. Support Care Cancer. 2014;22(1):7–14. doi: 10.1007/s00520-013-1947-8. [DOI] [PubMed] [Google Scholar]
- 36.Rolston KVI, Segreti J, Lamp KC, Friedrich LV. Cubicin outcomes registry and experience (CORE) methodology. Am J Med. 2007;120(10, Supplement 1):S4–S5. doi: 10.1016/j.amjmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 37.Martone WJ, Lindfield KC, Katz DE. Outpatient parenteral antibiotic therapy with daptomycin: insights from a patient registry. Int J Clin Pract. 2008;62(8):1183–1187. doi: 10.1111/j.1742-1241.2008.01824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Owens RC, Jr, Lamp KC, Friedrich LV, Russo R. Postmarketing clinical experience in patients with skin and skin-structure infections treated with daptomycin. Am J Med. 2007;120(10 Suppl 1):S6–S12. doi: 10.1016/j.amjmed.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 39.Keil F, Daikos GL, Skoutelis A, Dominguez JI, Pathan R, Hamed K. Daptomycin for gram-positive infections in patients with neutropenia: clinical experience from a European outcomes registry. Adv Ther. 2015;32(8):715–726. doi: 10.1007/s12325-015-0231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gonzalez-Ruiz A, Beiras-Fernandez A, Lehmkuhl H, Seaton RA, Loeffler J, Chaves RL. Clinical experience with daptomycin in Europe: the first 2.5 years. J Antimicrob Chemother. 2011;66(4):912–919. doi: 10.1093/jac/dkq528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gonzalez-Ruiz A, Beiras-Fernandez A, Lehmkuhl H, Dohmen PM, Loeffler J, Chaves RL. Effectiveness and safety of daptomycin in complicated skin and soft-tissue infections and bacteraemia in clinical practice: results of a large non-interventional study. Int J Antimicrob Agents. 2013;41(4):372–378. doi: 10.1016/j.ijantimicag.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 42.Seaton RA, Gonzalez-Ramallo VJ, Prisco V, Marcano-Lozada M, Gonzalez-Ruiz A, Gallegos B, et al. Daptomycin for outpatient parenteral antibiotic therapy: a European registry experience. Int J Antimicrob Agents. 2013;41(5):468–472. doi: 10.1016/j.ijantimicag.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 43.Timerman A, Brites C, Bicudo E, Grinbaum RS, Costa Filho R, Carrilho CD, et al. Brazilian experience in EU-CORE: daptomycin registry and treatment of serious gram-positive infections. Braz J Infect Dis. 2013;17(6):647–653. doi: 10.1016/j.bjid.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crompton JA, North DS, McConnell SA, Lamp KC. Safety and efficacy of daptomycin in the treatment of osteomyelitis: results from the CORE registry. J Chemother. 2009;21(4):414–420. doi: 10.1179/joc.2009.21.4.414. [DOI] [PubMed] [Google Scholar]
- 45.Benvenuto M, Benziger DP, Yankelev S, Vigliani G. Pharmacokinetics and tolerability of daptomycin at doses up to 12 milligrams per kilogram of body weight once daily in healthy volunteers. Antimicrob Agents Chemother. 2006;50(10):3245–3249. doi: 10.1128/AAC.00247-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu G, Abraham T, Rapp J, Vastey F, Saad N, Balmir E. Daptomycin: evaluation of a high-dose treatment strategy. Int J Antimicrob Agents. 2011;38(3):192–196. doi: 10.1016/j.ijantimicag.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Seaton RA, Menichetti F, Dalekos G, Beiras-Fernandez A, Nacinovich F, Pathan R, et al. Evaluation of effectiveness and safety of high-dose daptomycin: results from patients included in the European cubicin((r)) outcomes registry and experience. Adv Ther. 2015;32(12):1192–1205. doi: 10.1007/s12325-015-0267-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Safdar N, Andes D, Craig WA. In vivo pharmacodynamic activity of daptomycin. Antimicrob Agents Chemother. 2004;48(1):63–68. doi: 10.1128/AAC.48.1.63-68.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mensa J, Barberan J, Llinares P, Picazo J, Bouza E, Alvarez-Lerma F, et al. Guidelines for the treatment on infections caused by methicillin-resistant Staphylococcus aureus. Rev Esp Quimioter. 2008;21(4):234–258. [PubMed] [Google Scholar]
- 50.Baddour LM, Wilson WR, Bayer AS, Fowler VG, Jr, Tleyjeh IM, Rybak MJ, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American heart association. Circulation. 2015;132(15):1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 51.Gudiol F, Aguado JM, Pascual A, Pujol M, Almirante B, Miro JM, et al. [Consensus document for the treatment of bacteremia and endocarditis caused by methicillin-resistent Staphylococcus aureus. Sociedad Espanola de Enfermedades Infecciosas y Microbiologia Clinica] Enfermedades Infecciosas y Microbiología Clínica. 2009;27(2):105–115. doi: 10.1016/j.eimc.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 52.Kullar R, Casapao AM, Davis SL, Levine DP, Zhao JJ, Crank CW, et al. A multicentre evaluation of the effectiveness and safety of high-dose daptomycin for the treatment of infective endocarditis. J Antimicrob Chemother. 2013;68(12):2921–2926. doi: 10.1093/jac/dkt294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Figueroa DA, Mangini E, Amodio-Groton M, Vardianos B, Melchert A, Fana C, et al. Safety of high-dose intravenous daptomycin treatment: 3-year cumulative experience in a clinical program. Clin Infect Dis. 2009;49(2):177–180. doi: 10.1086/600039. [DOI] [PubMed] [Google Scholar]
- 54.Kullar R, Davis SL, Levine DP, Zhao JJ, Crank CW, Segreti J, et al. High-dose daptomycin for treatment of complicated gram-positive infections: a large, multicenter, retrospective study. Pharmacotherapy. 2011;31(6):527–536. doi: 10.1592/phco.31.6.527. [DOI] [PubMed] [Google Scholar]
- 55.Utili R, Cogo A, Cristini F, Prisco V, Sagnelli E, Tascini C, et al. Clinical experience with daptomycin in Italy: results from a registry study of the treatment of gram-positive infections between 2006 and 2009. J Chemother. 2012;24(2):113–121. doi: 10.1179/1120009X12Z.00000000023. [DOI] [PubMed] [Google Scholar]


