Abstract
Hypothesis
Nonotosclerotic stapes fixation does not represent a significant cause of stapes ankylosis in patients undergoing stapedectomy; the vast majority have otosclerosis.
Background
Nonotosclerotic stapes fixation has been proposed as the diagnosis in 30 to 40% of patients undergoing stapedectomy (after excluding rare congenital, systemic, and syndromic causes of stapes fixation and tympanosclerosis). This finding was based on the histopathologic evaluation of total stapedectomy surgical specimens. Since these specimens do not include the surrounding otic capsule, the histopathologic evidence of otosclerosis may be missed.
Methods
Human temporal bone specimens from patients who underwent stapes mobilization, stapedotomy, or stapedectomy during life were evaluated for histologic evidence of otosclerosis. Cases with a history of temporal bone trauma, tympanosclerosis, and congenital, systemic, or syndromic causes of stapes fixation were excluded. Therefore most temporal bone donors carried a clinical diagnosis of otosclerosis.
Results
Two hundred and ten specimens from three temporal bone collections were independently evaluated. Otosclerosis was found on histology in 99% (207/210). Therefore, the incidence of nonotosclerotic stapes fixation was 1% (3/210). In 2 of the 3 cases that did not have otosclerosis, the contralateral temporal bone had otosclerosis on histopathologic evaluation. These cases may have had otosclerosis in the footplate only (which was removed at the time of surgery and not available for review).
Conclusion
Nonotosclerotic stapes fixation is not likely a distinct pathologic classification from otosclerosis. Most patients diagnosed with nonotosclerotic stapes fixation likely have otosclerosis, but do not have otosclerotic foci in the stapes itself.
Keywords: stapedectomy, otosclerosis, nonotosclerotic stapes fixation
Introduction
Although otosclerosis is the most common cause of stapes ankylosis, there are many different etiologies. Rare causes include congenital stapes fixation, tympanosclerosis, temporal bone trauma, systemic skeletal diseases such as Paget’s disease, osteopetrosis, or osteogenesis imperfecta, and genetic disorders, such as NOG-Related Symphalangism Spectrum Disorders or X-linked stapes gusher syndromes. Identifying the correct etiologic cause of stapes fixation is important in the medical and/or surgical management of the associated hearing loss, and for counseling about the prognosis.
Nonotosclerotic stapes fixation, formerly referred to as pseudo-otosclerosis, may represent another etiology of stapes ankylosis 1. It has been reported as the cause of stapes fixation in up to 40% patients undergoing stapedectomy procedures, after excluding those with the rare causes listed above 2. This diagnosis is based on the absence of otosclerotic foci on histologic examination of whole stapes footplate specimens removed at the time of total stapedectomy. Under the classification of nonotosclerotic stapes fixation, there are six alternative pathologic etiologies of stapes fixation, including annular calcification, globular fibrosis, lymphocytic infiltration, hemosiderosis, granulomas, or amyloidosis 2.
We hypothesize that patients diagnosed with nonotosclerotic stapes ankylosis actually have otosclerosis in the surrounding otic capsule that is not removed as part of the surgical specimen. Stapes footplate specimens may not contain evidence of otosclerotic foci because the disease most often begins in the otic capsule adjacent to the footplate. The otosclerotic foci may be left behind in the otic capsule when the stapes footplate is removed at surgery. Although the diagnosis of otosclerosis can be confirmed on surgical stapes specimens, this may not be an adequate method to rule out a diagnosis of otosclerosis.
In order to clarify whether nonotosclerotic stapes fixation represents a pathologic entity that is distinct from otosclerosis, we evaluated human temporal bone histopathologic specimens. We reviewed consecutive temporal bone specimens from patients who had undergone a stapes surgery for stapes ankylosis in life (mobilization, stapedectomy, or stapedotomy) to determine if there was evidence of otosclerosis in the otic capsule. These specimens included the entire otic capsule, with the cochlea, oval and round window areas, the vestibular organs, and the middle ear with the ossicles and tympanic membrane, but did not include the portion of the stapes that was surgically removed. The goal was to identify cases of nonotosclerotic stapes fixation in these collections, and determine the pathologic etiologies in these cases. This was a multi-institutional study in order to ensure potential pathologic diversity of specimens, include multiple reviewers, and allow for a large sample size.
Materials and Methods
This study included cases from the temporal bone pathology collections at the Massachusetts Eye and Ear Infirmary (MEE), the University of Minnesota (U of M), and House Temporal Bone Laboratory at the University of California Los Angeles (House UCLA). The investigators at each institution independently evaluated the specimens contained in his/her own institution’s temporal bone collection. Consecutive temporal bone specimens with a history of stapes mobilization, stapedectomy, or stapedotomy in life were evaluated, with a goal to reach over 200 reviewed cases between the three institutions. Cases were excluded if there was a history of chronic otitis media with tympanosclerosis, temporal bone trauma, systemic skeletal diseases such as Paget’s disease, osteopetrosis, or osteogenesis imperfecta, and genetic disorders, such as NOG-Related Symphalangism Spectrum Disorders or X-linked stapes gusher syndromes.
Temporal bone specimens had been collected shortly after death, and were fixed, decalcified, and embedded. Sections, 20 microns thick, were made per standard temporal bone histopathologic techniques3. Every tenth section was placed on a slide and stained with Hematoxylin and Eosin. The pathology reports were reviewed. These reports were written by experienced temporal bone histopathologists at each institution based on previous evaluations of the temporal bone specimen. Slides were re-reviewed by light microscopy for any case without a convincing description of a focus/foci of otosclerosis and for any specimen with incomplete records at U of M and House UCLA. The histopathologic slides for all specimens from the MEE collection were re-reviewed in order to identify any disagreements between the previously written pathology reports and the pathologic diagnosis based on our re-review of the slides. There were no discrepancies and the reports were found to be reliable; therefore we re-reviewed slides at the other two institutions only when the reports written by expert otopathologists were incomplete, inconclusive, or not available. The diagnosis of otosclerosis was based on classic pathologic findings in otosclerosis, such as areas of bone resorption, immature bone deposition, increased perivascular spaces due to bone resorption, basophilic staining lesions demonstrating expansion, active areas with high cellularity and inactive areas with connective tissue replacing otic capsule bone4.
Results
A total of 210 temporal bone specimens with a history of stapes mobilization, stapedectomy, or stapedotomy were reviewed. This included all 39 specimens in the U of M collection and all 106 specimens in the MEE collection that met inclusion and exclusion criteria. Although more than 500 temporal bone specimens in the House UCLA collection met the inclusion criteria, only 62 consecutive specimens were included because the combined multi-center goal of more than 200 cases had already been reached.
Otosclerosis was diagnosed on histopathology in 207 out of the 210 reviewed temporal bone specimens (99%). Three out of 210 cases (1%) did not have evidence of otosclerosis on histopathology. These three cases are presented here in further detail.
In all three cases, a successful total stapedectomy had been performed during life. In cases 1 and 3, audiograms were available that documented a significant postoperative hearing improvement with closure of the air bone gap.
In case 2, the patient had a mixed hearing loss pre-operatively with a word recognition score of 16%. A post-operative audiogram was not available, but clinical records indicate marked subjective improvement of hearing though persistent distortion of sounds.
The incus and malleus were normal in all three cases, without evidence of fixation. The stapes prosthesis was in good position in all three cases. Superior canal dehiscence could not be excluded as a cause of conductive hearing loss due to the horizontal sectioning in these specimens.
In Case 1, densely basophilic staining bone was noted anterior to the oval window, surrounding a cartilage rest, but there were no histologic features of otosclerosis (Figure 1). In case 2, a densely basophilic fragment of the stapes crura was seen, but no osteoclasts or pseudo-vascular spaces were present; thus, there was not convincing evidence of otosclerosis (Figure 2). In case 3, the otic capsule anterior to the oval window had dense basophilic staining, but no specific pathologic features of otosclerosis (Figure 3).
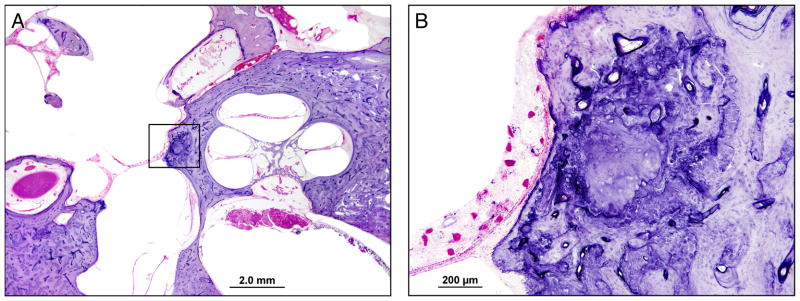
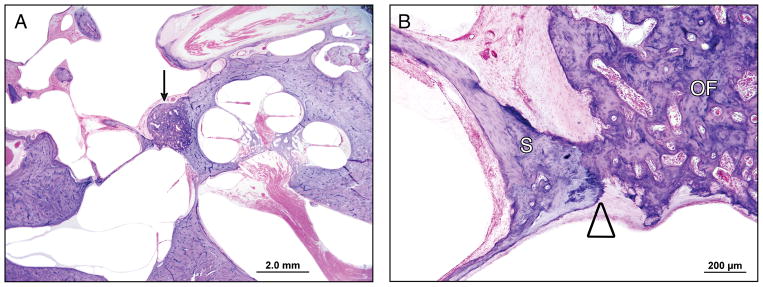
Figure 1.
Temporal Bone Case 1: A) Low power image through the cochlea, vestibule and oval window. No otosclerosis is seen. There is evidence of a stapedectomy with complete removal of the stapes footplate. B) High power image of the boxed area in A, which includes the otic capsule at the anterior margin of the oval window. There is basophilic staining anterior to the oval window with a prominent cartilaginous rest in the area of the fissula ante fenestram, but there is no otosclerosis.
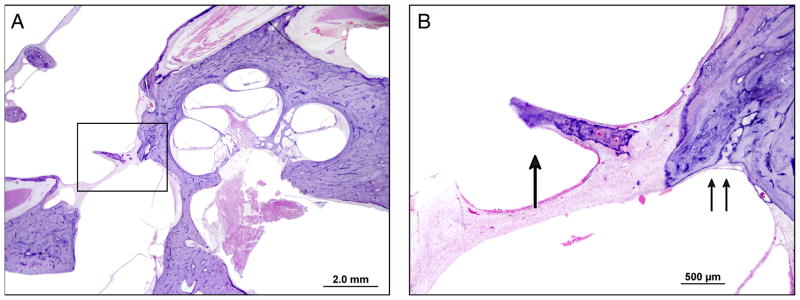
Figure 2.
Temporal Bone Case 2: A) Low power image through the cochlea, vestibule and oval window. No otosclerosis is seen. There is evidence of a stapedectomy with complete removal of the stapes footplate. B) High power image of the boxed area in A, which includes the otic capsule at the anterior margin of the oval window and part of the fibrous seal across the oval window. The single arrow points to bony fragment embedded in the fibrous tissue sealing the oval window, which is likely a piece of the stapes crura. Although this fragment is basophilic with two small vascular spaces, these findings alone are not diagnostic of otosclerosis. The double arrows indicate the normal appearing fissula ante fenestram.
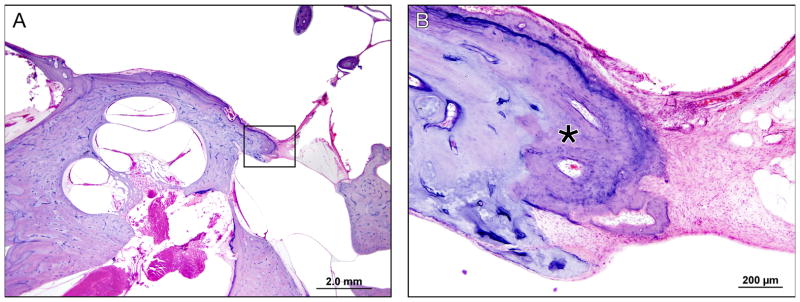
Figure 3.
Temporal Bone Case 3: A) Low power image through the cochlea, vestibule and oval window. No otosclerosis is seen. There is evidence of a stapedectomy with complete removal of the stapes footplate. B) High power image of the boxed area in A, which is the otic capsule at the anterior margin of the oval window. The “*” indicates an area with slightly more basophilic bone, but no otosclerotic foci are seen.
Otosclerosis was found on histopathologic evaluation of the contralateral temporal bone in cases 1 and 2, but not in case 3.
Discussion
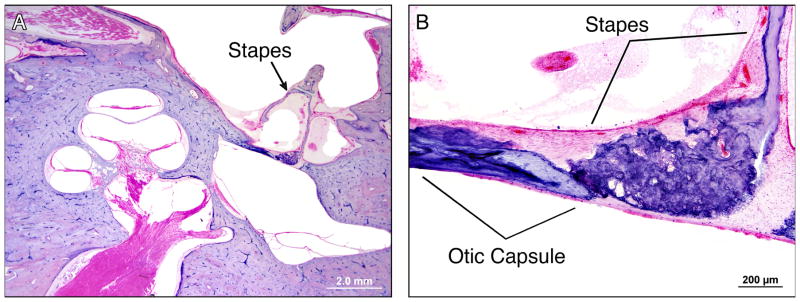
After excluding known rare causes of stapes ankylosis (such as congenital fixation, trauma, tympanosclerosis, and genetic, syndromic, or systemic disorders), 99% of the temporal bone specimens in this study had histopathologic evidence of otosclerosis. In 2 of the 3 cases in which otosclerosis was not found on histology, the contralateral temporal bone had evidence of otosclerosis. The rate of bilaterality in otosclerosis ranges from 75.6% in temporal bones with both clinical and histologic otosclerosis to 90% in clinical studies5,6. The finding of otosclerosis in the contralateral temporal bone, in combination with convincing clinical evidence of stapes ankylosis (i.e. an improved air bone gap after stapedectomy), makes it likely that the examined temporal bones did have otosclerosis. Since the specimens without evidence of otosclerosis had undergone a total stapedectomy during life, the stapes footplates were not available for review. In these cases, there may have been otosclerosis that involved the stapes footplate only, resulting in a focal fixation point (Figure 4). The pathologic evidence of otosclerosis could therefore have been removed with the stapes during the stapedectomy in life. Schuknecht found the rate of otosclerosis totally within the footplate was 1.6% 7, which is consistent with finding that 1% of these patients may have had otosclerosis only in the footplate.
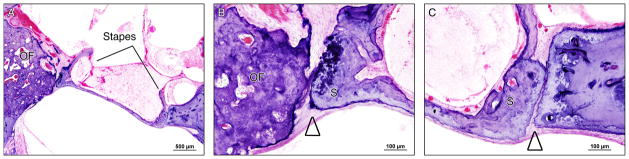
Figure 4.
Example of footplate only otosclerosis. A) Low power image through the otic capsule demonstrating that the only focus of otosclerosis is within the stapes footplate. B) High power image through the stapes footplate demonstrating fixation of the otosclerotic lesion within the footplate to the otic capsule bone forming the superior margin of the oval window.
The findings from this study are not consistent with the 30 to 40% rate of nonotosclerotic stapes fixation reported as a separate pathologic cause of stapes ankylosis in patients undergoing total stapedectomy 2. Otosclerosis is a disease of the otic capsule that most commonly involves the area anterior to the oval window, and often leads to stapes fixation. We propose that histologic evaluation of the stapes footplate alone, without evaluation of the otic capsule, underestimates the incidence of otosclerosis. In some patients, stapes fixation may be due to an isolated point fixation of the footplate without extension of the otosclerotic focus into the footplate itself (Figure 5). Removal of the stapes may not avulse any of the otosclerotic bone that would enable confirmation of otosclerosis as the pathologic cause of ankylosis. Similarly, early lesions of otosclerosis can expand the otic capsule bone adjacent to the oval window, leading to “jamming” of the stapes footplate 8 (Figure 6). Since the otosclerosis does not extend into the footplate itself, the diagnosis may again be missed when post-stapedectomy surgical specimens are examined. In a prior study, McKenna et al. examined 27 stapes footplate specimens from patients undergoing stapedectomy with a clinical diagnosis of otosclerosis, and found only 4 that specimens contained foci of otosclerosis by light microscopy or electron microscopy evaluation 9. Although the examination of fragmented, rather than whole, stapes footplate specimens may yield specimens containing histologic evidence of otosclerosis less frequently, this prior study illustrates the lack of otosclerotic foci in many footplate specimens from patients with a clinical diagnosis of otosclerosis.
Figure 5.
Example of point fixation of an otosclerotic lesion within the otic capsule to the uninvolved footplate A) Low power image through the otic capsule. The arrow points to a focus of otosclerosis anterior to the oval window B) High power image through the anterior stapedovestibular joint area. The triangle indicates the point of fixation where the otosclerotic lesion contacts and fixes the footplate, but note that there is no extension of otosclerosis into the footplate itself. Therefore, removal of the stapes footplate and histologic examination of the footplate would not show evidence of otosclerosis.
Figure 6.
Example of “jamming” of the stapes footplate due to adjacent otosclerotic lesion in the otic capsule. A) Medium power image through the stapes footplate demonstrates an otosclerotic focus (“OF”) anterior to the oval window. B) High power image of the anterior stapedo-vestibular joint space showing point fixation, but no extension of otosclerosis into the stapes itself. C) High power image of the posterior stapedo-vestibular joint space showing “jamming”, or posterior displacement of the stapes footplate so that it contacts the posterior margin of the oval window.
Important advances in understanding the etiology of otosclerosis have come from immunohistochemical and molecular studies of the stapes surgical specimens. Measles virus nucleocapsid was identified by transmission electron microscopy and immunofluorescence and immunoperoxidase staining of stapes footplate fragments with active otosclerosis10. Measles virus RNA has been isolated in stapes specimens containing otosclerosis, but not in those without otosclerosis (i.e. patients diagnosed with nonotosclerotic stapes fixation) 11. Furthermore, stapes specimens containing otosclerosis have demonstrated increased measles virus receptor CD46 positive osteoclasts 12, and increased tumor necrosis factor alpha receptor (TNFR) expression 13 compared to those without otosclerosis (i.e. nonotosclerotic stapes fixation). It is possible that these findings are specific to otosclerotic foci, but not to uninvolved bone from patients who have otosclerosis.
The inability to assess the pathology of the otic capsule during life limits further pathophysiologic understanding of stapes ankylosis in patients diagnosed with nonotosclerotic stapes fixation. High resolution computed tomography (CT) may be used to assess for otosclerotic foci within the otic capsule with a sensitivity of 80% when radiologic findings are compared to temporal bone histology findings 14, or over 90% when radiologic findings are evaluated in patients with a clinical diagnosis of otosclerosis 15. A non-blinded study evaluating high resolution CT findings in 15 patients with nonotosclerotic stapes fixation (diagnosis based on lack of otosclerosis found in the stapes surgical specimens) found no findings suggestive of otosclerosis in all 15 CT studies 16. The lack of radiologic evidence of otosclerosis in all examined specimens certainly suggests a pathology other than otosclerosis. These findings, however, are not consistent with the findings from the current histopathologic study in which nearly all post-stapedectomy temporal bone specimens had otosclerosis.
One limitation of the current study is the inability to evaluate the stapes footplate and stapedo-vestibular joint histopathology with the stapes in situ. This would have enabled clarification of the cause of stapes ankylosis in the three cases in which otosclerosis was not found. Temporal bones from patients who had undergone stapes surgeries were selected as the study specimens, however, because a significant incidence of nonotosclerotic stapes fixation has been reported among patients who underwent stapedectomy.
The current study does not find convincing evidence that nonotosclerotic stapes fixation represents a significant distinct pathologic diagnosis. The correct pathologic classification in cases of stapes ankylosis is critical to future progress in the development and evaluation of novel medical treatments for otosclerosis.
Acknowledgments
The authors wish to thank Diane Jones, Jennifer O’Malley, Barbara Burgess, Mengyu Zhu for preparation of the temporal bone specimens and assistance with searching the Mass. Eye and Ear temporal bone database, and Garyfallia Pagonis for assistance with preparation of the figures and photomicrographs.
This work was supported by a grant from the National Institutes of Health (NIH) U24 DC011943-03.
References
- 1.Karosi T, Kónya J, Petkó M, et al. Two subgroups of stapes fixation: otosclerosis and pseudo-otosclerosis. The Laryngoscope. 2005;115(11):1968–1973. doi: 10.1097/01.mlg.0000178325.48942.f1. [DOI] [PubMed] [Google Scholar]
- 2.Karosi T, Csomor P, Petkó M, et al. Histopathology of nonotosclerotic stapes fixations. Otol Neurotol. 2009;30(8):1058–1066. doi: 10.1097/MAO.0b013e31819fe802. [DOI] [PubMed] [Google Scholar]
- 3.Schuknecht. Pathology of the Ear. Lea & Febiger; 1993. [Google Scholar]
- 4.Merchant SN, Nadol JB. Schuknecht’s Pathology of the Ear. PMPH-USA; 2010. [Google Scholar]
- 5.Hueb MM, Goycoolea MV, Paparella MM, Oliveira JA. Otosclerosis: the University of Minnesota temporal bone collection. Otolaryngology -- Head and Neck Surgery. 1991;105(3):396–405. doi: 10.1177/019459989110500308. [DOI] [PubMed] [Google Scholar]
- 6.Larsson A. Otosclerosis. A genetic and clinical study. Acta Otolaryngol Suppl. 1960;154:1–86. [PubMed] [Google Scholar]
- 7.Schuknecht HF, Barber W. Histologic variants in otosclerosis. The Laryngoscope. 1985;95(11):1307–1317. doi: 10.1288/00005537-198511000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Cherukupally SR, Merchant SN, Rosowski JJ. Correlations between pathologic changes in the stapes and conductive hearing loss in otosclerosis. Ann Otol Rhinol Laryngol. 1998;107(4):319–326. doi: 10.1177/000348949810700410. [DOI] [PubMed] [Google Scholar]
- 9.McKenna MJ, Mills BG, Galey FR, Linthicum FH. Filamentous structures morphologically similar to viral nucleocapsids in otosclerotic lesions in two patients. Am J Otol. 1986;7(1):25–28. [PubMed] [Google Scholar]
- 10.McKenna MJ, Mills BG. Ultrastructural and immunohistochemical evidence of measles virus in active otosclerosis. Acta Otolaryngol Suppl. 1990;470:130–9. discussion 139–40. [PubMed] [Google Scholar]
- 11.Karosi T, Kónya J, Szabó LZ, Sziklai I. Measles virus prevalence in otosclerotic foci. Adv Otorhinolaryngol. 2007;65:93–106. doi: 10.1159/000098677. [DOI] [PubMed] [Google Scholar]
- 12.Karosi T, Jókay I, Kónya J, et al. Activated osteoclasts with CD51/61 expression in otosclerosis. The Laryngoscope. 2006;116(8):1478–1484. doi: 10.1097/01.mlg.0000227251.67251.1f. [DOI] [PubMed] [Google Scholar]
- 13.Csomor P, Sziklai I, Karosi T. TNF-alpha receptor expression correlates with histologic activity of otosclerosis. Otol Neurotol. 2009;30(8):1131–1137. doi: 10.1097/MAO.0b013e3181be6af4. [DOI] [PubMed] [Google Scholar]
- 14.Quesnel AM, Moonis G, Appel J, et al. Correlation of computed tomography with histopathology in otosclerosis. Otol Neurotol. 2013;34(1):22–28. doi: 10.1097/MAO.0b013e318277a1f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lagleyre S, Sorrentino T, Calmels M-N, et al. Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol. 2009;30(8):1152–1159. doi: 10.1097/MAO.0b013e3181c2a084. [DOI] [PubMed] [Google Scholar]
- 16.Karosi T, Csomor P, Sziklai I. The value of HRCT in stapes fixations corresponding to hearing thresholds and histologic findings. Otol Neurotol. 2012;33(8):1300–1307. doi: 10.1097/MAO.0b013e31826352ad. [DOI] [PubMed] [Google Scholar]