Abstract
[Purpose] Smartphones are widely used by teenagers and adults for various purposes. As teenagers use smartphones more actively than adults, they are more prone to be addicted to smartphones. Furthermore, excessive usage of smartphones can lead to various psychosocial and physical symptoms. [Subjects and Methods] One hundred teenage subjects were recruited and divided into normal and addiction groups, based on the criteria of the smartphone addiction scale-short version questionnaire. Craniocervical posture and mobility were examined by lateral cephalometric analysis and a cervical range of motion instrument. [Results] Cephalometric analysis showed no significant difference in the craniocervical angles of the resting positions of the two groups. However, measurement using an inclinometer revealed a significantly flexed cervical posture while using smartphones and decreased cervical range of motion in the smartphone-addicted teenagers. The clinical profile of temporomandibular disorders revealed that muscular problems were more frequently presented in the smartphone-addicted teenagers. [Conclusion] These findings suggest that smartphone addiction has a negative influence on craniocervical posture and mobility. Further, it can be postulated that smartphone addiction among teenagers may have contributed to the occurrence of myogenous temporomandibular disorders. In conclusion, smartphone-addicted teenagers may be more frequently subjected to muscular disturbance in the craniocervical area, which probably affects the pathologic process of temporomandibular disorders in teenagers.
Key words: Craniocervical posture, Craniocervical pain, Smartphone addiction
INTRODUCTION
Smartphones have made ubiquitous internet access possible, with no bounds on time or place, and are used for a wide range of purposes ranging from simple pleasure and communication to business. Since the iPhone was publicly introduced in 2009, the number of smartphone users has markedly grown to more than 40 million (79.6%) in Korea1). However, at the same time, there are growing concerns about smartphone addiction, which is defined as the uncontrollable overuse of smartphones and their subsequent interference with daily life2). Though these phones are still only a recent introduction, a National Information Agency survey has revealed that the prevalence of smartphone addiction (8.4%) has surpassed than that of internet addiction (7.7%)3). However, sufficient information including proper guidelines has not been provided either by manufacturers or clinicians regarding the use of smartphones. Regarding the age-dependent prevalence of smartphone addiction, previous studies have reported that teenagers are more likely to be absorbed in digital media, and have a higher addiction rate than adults. A recent study showed that the smartphone penetration rate among teenagers was greater than in other age groups4). Furthermore, a different national survey revealed that smartphone addiction is twice more prevalent among teenagers than among adults5).
The symptoms of smartphone addiction can be grossly classified into two categories: psychosocial disorders, including sleep disorders, aggressive or depressive symptoms, dropping out of school, and antisocial personality disorder; and physiological disorders, including dry eyes, carpal tunnel syndrome, musculoskeletal disorders, and migraine headaches6). Among them, musculoskeletal disorders occur predominantly in the fingers, neck, back, and shoulder, which are the regions mainly involved in prolonged usage of a smartphone7). In addition, previous researchers have reported that prolonged usage of digital media, including smartphones, frequently causes deleterious alterations to head and neck posture, rounding the shoulders and pushing the head forward8). Furthermore, the increased usage of smartphones has been reported to cause significant alterations in upper cervical posture8). It is also known that misalignment of the upper cervical posture can induce alterations in muscular tone, musculoskeletal dysfunction, and pain, even resulting in structural damage to the head and shoulders9). Other studies have found that smartphone use could be related to musculoskeletal symptoms, including muscular fatigue and tenderness, as well as a decreased cervical range of motion10, 11).
Furthermore, many studies have suggested that a misaligned craniocervical posture could be partly responsible for the initiation or aggravation of temporomandibular disorders (TMDs), which are defined as musculoskeletal disorders of the masticatory muscles and temporomandibular joint12). Previous studies have found that poor cervical posture may contribute to the pathologic process of TMDs by changing the muscle tone of the stomatognathic system13, 14). Even though a few studies have reported that smartphone addiction leads to various alterations in head and shoulder posture and mobility, the exact musculoskeletal effect of smartphone addiction in the craniocervical area remains unclear. Moreover, there has been little study of the effect of smartphone addiction on the clinical profiles of teenagers with TMDs.
The purpose of this study was, therefore, to define the effect of smartphone addiction on cervical posture and function as well as TMDs in teenagers with smartphone addiction. This study was designed to analyze the lateral cephalometric profile of the craniocervical area and measure the cervical range of motion using a motion inclinometer after identifying smartphone addiction in teenagers with TMD-related symptoms using the Smartphone Addiction Scale—Short Version (SAS-SV) questionnaire15).
SUBJECTS AND METHODS
One hundred teenage participants were randomly enrolled from patients who visited the Department of Oral Medicine at Kyungpook National University Hospital with TMD-related symptoms from December 2014 to February 2015. Individuals with a history of rheumatoid arthritis or congenital musculoskeletal problems were excluded from this study. Fifty subjects each were recruited for the normal and addiction groups, based on the criteria of the smartphone addiction scale-short version (SAS-SV) validated by Kwon et al15). These patients voluntarily consented to participate in the experiment after receiving sufficient explanation regarding the experiment’s methods and the study’s purpose. Because the participants were teenagers, their parents were also given explanations about the study. This study was approved by Kyungpook National University Hospital’s Institutional Review Board (IRB code: 2014-11-018). In addition, all subjects and their parents were provided with a full explanation of the protocol, and their written informed consent was obtained before the study began. The demographic characteristics of the subjects who participated in this study are summarized in Table 1.
Table 1. Demographic characteristics of the subjects.
| Normal group (n=50) | Addiction group (n=50) | |
|---|---|---|
| Gender (M/F) | 16/34 | 12/38 |
| Age (years) | 16.86 ± 1.60 | 17.02 ± 2.00 |
Values are mean ± SD
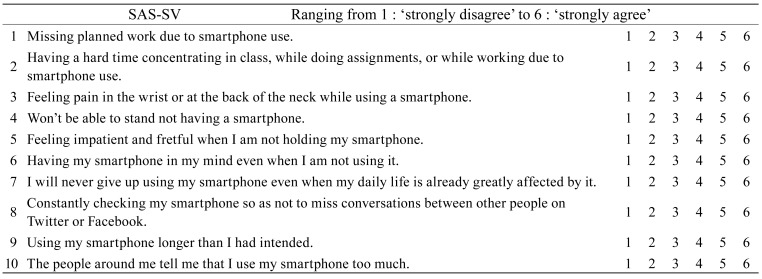
The SAS-SV is a self-reporting scale of smartphone addiction that consists of 6 factors and 10 items with a six-point Likert-type scale (ranging from 1: ‘strongly disagree’ to 6: ‘strongly agree’). The six factors include daily-life disturbance, positive anticipation, withdrawal, cyberspace-oriented relationship, overuse, and tolerance. Participants were asked to fill out the questionnaire on smartphone addiction-related symptoms occurring within the past 3 months. The questionnaire is included in Appendix 1.
Lateral cephalograms were taken using a CX-90SP II (Asahi Roentgen Ind. Co. Ltd., Kyoto, Japan) with exposure settings of 70 kV and 80 mA. The subjects were instructed to close their mouths in centric occlusion. Any deviations of the head and neck were corrected with the guidance of a light beam by an examiner blinded to the group classification. This procedure allowed the examiner to maintain a fixed distance between the mid-sagittal plane of the head and the x-ray source and cassette. This technique ensures a constant enlargement of 10% of the mid-sagittal plane and thus permits the precise analysis of the linear and angular dimensions. Ear rods in the cephalostat were not used to minimize external influences and to allow the participant to assume a resting posture. The radiologist was asked to register a lateral skull radiograph including the neck from the vertex to the sixth cervical vertebra16).
The cervical lordosis angle represents the alignment of the cervical spine. If it is decreased from the normal range, it may mean that there is a straightened neck or cervical kyphosis. To assess this angle, three reference points (cv2tg, cv4ip, cv6ip) were marked, and two reference lines [CVT (cv2tg-cv4ip) and EVT (cv4ip-cv6ip)] were traced using a software program (INFINITT PACS®, INFINITT Co. Ltd., Seoul, Korea) used at Kyungpook National University Dental Hospital. These reference points and lines were traced according to the analytical method described by D’Attilio et al16). The cervical lordosis angle (CVT/EVT) was defined as the downward opening angle between the CVT/EVT lines (Fig. 1). To eliminate intra-examiner variation, all measurements were performed 3 times. The mean value of 3 consecutive measurements was calculated and used for the data analysis.
Fig. 1.
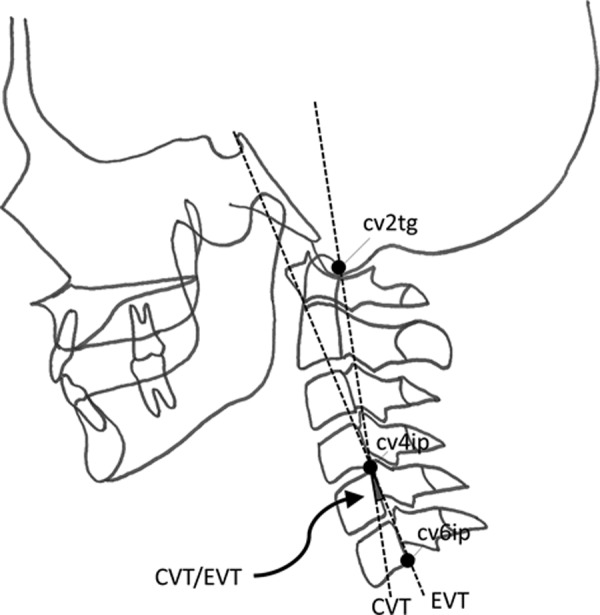
Cervical lordosis angle. cv2tg: tangent point of the superior, posterior extremity of the odontoid process of the second cervical vertebra; cv4ip: the most inferior-posterior point on the body of the fourth cervical vertebra; cv6ip: the most inferior-posterior point on the body of the sixth cervical vertebra; CVT: upper part of cervical spine, line through cv2tg and cv4ip; EVT: lower part of the cervical spine, line through cv4ip and cv6ip; CVT/EVT: cervical lordosis angle, downward opening angle between the CVT and EVT lines.
The craniocervical angle (NSL/OPT, NSL/CVT) represents the posture of the head relative to the cervical column line (Fig. 2). For the NSL/OPT angle, four reference points (N, S, cv2tg, and cv2ip) were marked and two lines [NSL (N-S) and OPT (cv2tg-cv2ip)] were traced. Four reference points (N, S, cv2tg, and cv4ip) were marked for the NSL/CVT angle, and two lines [NSL (N-S) and CVT (cv2tg-cv4ip)] were traced. To eliminate intra-examiner variation, all measurements were performed 3 times. The mean value of 3 consecutive measurements was calculated and used for the data analysis.
Fig. 2.
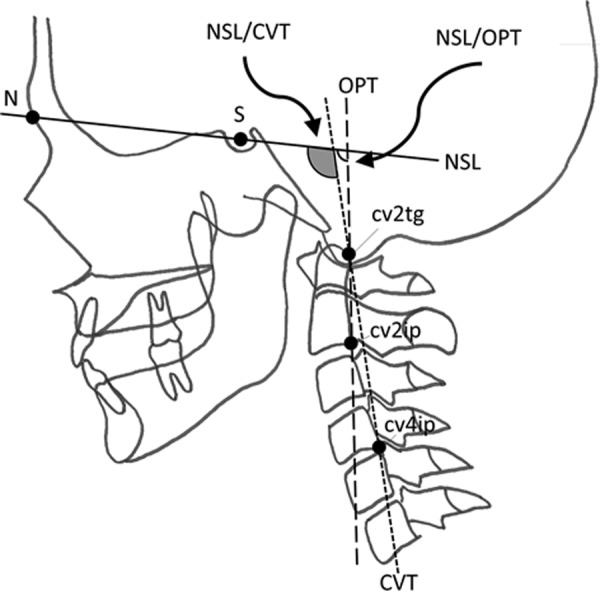
Craniocervical angle. N: nasion point; S: sella point; cv2tg: tangent point of the superior, posterior extremity of the odontoid process of the second cervical vertebra; cv2ip: the most inferior-posterior point on the body of the fourth cervical vertebra; cv4ip: the most inferior-posterior point on the body of the sixth cervical vertebra; NSL: nasion-sella line, line through N and S; OPT: odontoid line, line through cv2tg and cv2ip; CVT: upper part of the cervical spine, line through cv2tg and cv4ip; NSL/OPT: craniocervical angle, downward opening angle between the NSL and OPT lines; NSL/CVT: craniocervical angle, downward opening angle between the NSL and CVT lines.
A cervical range of motion (CROM) device (cervical range of motion instrument, Sammons Preston, Oklahoma, USA) was used to measure the cervical range of motion. This instrument has both high inter- and intra-observer reliabilities17). The CROM was aligned on the nose bridge and ears and then fastened to the head with a Velcro strap (Fig. 3A). Three dial angle meters were used to take most of the measurements. The sagittal plane meter and the lateral flexion meter are gravity meters. The rotation meter is magnetic and responds quickly to the shoulder-mounted magnetic yoke, accurately measuring cervical rotation. Because the rotation meter is controlled by the magnetic yoke, shoulder substitution is eliminated. Participants were seated on an adjustable-height chair without a backrest, with their knee and hip joints at 90° and their feet on the floor. The subjects were instructed to adopt the posture they habitually adopt during smartphone usage. Then, the sagittal view of the cervical flexion angle was measured to evaluate the habitual posture assumed while using a smartphone.
Fig. 3.
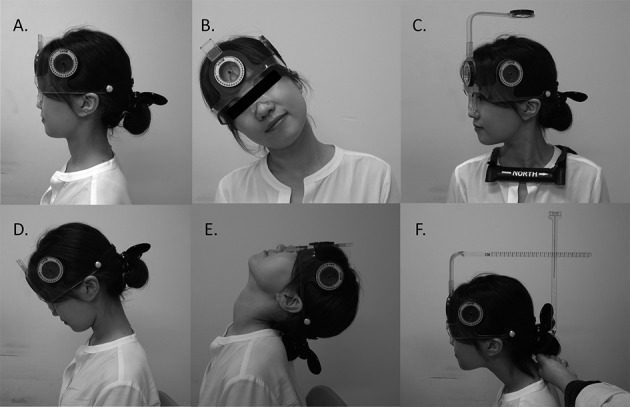
A: Aligned cervical range of motion; B: Cervical lateral flexion; C: Cervical rotation; D: Cervical Flexion; E: Cervical Extension; F: Cervical protrusion.
To examine the craniocervical mobility, subjects were instructed to flex their heads laterally to the left while keeping the shoulders level and without rotating the head. To exclude shoulder movement, the examiner restricted shoulder elevation by lightly placing his or her hand on the subject’s right shoulder and manually correcting any head motion that occurred outside the coronal plane. The same procedure was also followed for lateral flexion to the right (Fig. 3B). A magnetic yoke was placed on the subject’s shoulders with the arrow pointing north. The lateral flexion and sagittal plane meters must read zero for the rotation meter to be level. As the subject faced straight ahead, the examiner adjusted the rotation meter with his or her thumb and index finger until one of the pointers indicated a zero point. The subjects were then instructed to rotate their head horizontally to left side as far as possible without any shoulder rotation. The same procedure was also followed for rotation to the right (Fig. 3C). To assure maximal flexion in multi-joint areas, the participant was first instructed to ‘nod your head to make a double chin’ (suboccipital flexion), then encouraged to flex further until full cervical flexion was obtained (Fig. 3D). To measure cervical extension, the subject was instructed to ‘nod your head back’ (suboccipital extension), then extend further until full extension was achieved (Fig. 3E). The aforementioned measurements were calibrated in angles using suitable dial angle meters.
A forward head arm was attached to the CROM in place of the rotation arm. To position the forward head arm horizontally, the examiner guided the subject to position his or her head in a position where the sagittal plane meter indicated zero. While the subject maintained this position, the examiner located the foot (bottom tip) of the vertebra locator on the spinous process of the 7th cervical vertebra. The subject was instructed to retrude the head as far back as possible while keeping the chin level. Thereafter, the participant was again asked to protrude the head forward as much as possible with the air bubble placed centrally within the liquid-filled vial on top of the vertebral locator. Cervical protrusion was calibrated in centimeters for the horizontal distance from the retruded position to the maximally protruded position, as indicated by cross points between the forward head arm and the locator contact point (Fig. 3F). For higher reliability, all measurements were performed 3 times. The mean value of 3 consecutive measurements was calculated and used for data analysis.
Diagnosis of TMDs was made based on patients’ chief complaints, clinical histories, radiological examinations (panoramic, the four TMJ panoramic, and lateral cephalometric radiograph), and clinical examinations using the modified research diagnostic criteria for temporomandibular disorders (RDC/TMD) with an extended examination of craniocervical muscle. Diagnoses were categorized into joint (e.g., anterior disc displacement, degenerative joint disease, capsulitis, and so on), muscular (e.g., masseter muscle, temporalis muscle, local muscle soreness, and so on), and mixed problems (muscular problems along with joint problems). To eliminate inter-examiner variation, one examiner made the diagnosis for all patients.
The statistical analysis for quantitative variables was carried out using descriptive measures, such as mean value ± standard deviation. The qualitative variables were analyzed by calculating the absolute and relative frequencies (percentage). Statistical evaluation of the data was performed using the Statistical Package for the Social Sciences (SPSS) version 22.0 software for Windows (SPSS Inc., Chicago, IL, USA), including the independent two-sample t-test, Mann-Whitney U test, and Pearson Chi-square test (independence test). The independent two-sample t-test for an independent sample was selected for comparing the differences in posture while using a smartphone, lateral flexion, rotation, cervical flexion, cervical extension, and cervical protrusion between the normal and the addicted group. The Mann-Whitney U test was used to compare differences in posture between the normal and the addicted group, according to subdiagnoses of TMDs. We assessed posture while using a smartphone, lateral flexion, rotation, cervical flexion, cervical extension, and cervical protrusion. Pearson’s χ2 test was used to analyze the differences in diagnoses of TMDs between the two groups. A difference of p < 0.05 was considered statistically significant.
RESULTS
The mean SAS-SV score was 23.74±5.48 in the addicted group and 38.54±5.42 in the normal group. The cut-off value for the SAS-SV score was applied as 31 for boys and 33 for girls as determined by a previous study on the diagnostic ability of SAS-SV18). Twelve of 28 boys (42%) and 38 of 72 girls (52%) were accordingly assigned to the addiction group.
The mean value of the cervical lordosis angle (CVT/EVT) was measured as 6.64° for the normal group and 5.78° for the addiction group. Although this value was smaller in the addiction group than in the normal group, there was no significant difference between the two groups. The mean value of the craniocervical angle (NSL/OPT) was 102.87° for the normal group and 101.63° for the addiction group. In addition, the mean value for the craniocervical angle (NSL/CVT) was 107.07° for the normal group and 106.22° for the addiction group. Although the mean value of the craniocervical angle in the addiction group was smaller than in the normal group, no significant difference was found between the two groups (Table 2).
Table 2. Analysis of resting posture.
| Normal group | Addiction group | |
|---|---|---|
| Cervical lordosis angle (°) (CVT/EVT) | 6.64 ± 4.91 | 5.78 ± 4.86 |
| Craniocervical angle (°) (NSL/OPT) | 102.87 ± 8.09 | 101.63 ± 6.03 |
| Craniocervical angle (°) (NSL/CVT) | 107.07 ± 7.80 | 106.22 ± 6.17 |
Values are mean ± SD
The mean flexion angle was 12.87° in the normal group and 28.86° for the addiction group, indicating that subjects in the addiction group had a cervical posture that was twice as flexed while using a smartphone. Significant decreases in lateral flexion, rotation, cervical flexion, and cervical extension were found. However, there was no significant difference in cervical protrusion between the two groups. These results show that craniocervical mobility in the addiction group was significantly decreased in almost every direction compared to the normal group (Table 3). There were significant differences in all measurements between the normal and addiction groups with muscular problems, except for lateral flexion. There were also significant differences in all measurements between the two groups with joint problems, except for right lateral flexion and cervical flexion. However, no significant difference while using a smartphone was found between the groups with a mixed problem, except for cervical flexion (Table 4).
Table 3. Habitual posture and craniocervical mobility.
| Normal group | Addiction group | |
|---|---|---|
| Cervical flexion posture while using a smartphone (°) | 12.87 ± 10.56 | 28.86 ± 13.02** |
| Lateral flexion (Rt.) (°) | 40.57 ± 4.69 | 33.57 ± 8.72** |
| Lateral flexion (Lt.) (°) | 42.87 ± 5.97 | 36.13 ± 7.62** |
| Rotation (Rt.) (°) | 68.50 ± 7.26 | 59.60 ± 6.85** |
| Rotation (Lt.) (°) | 69.37 ± 8.24 | 61.40 ± 7.22** |
| Cervical flexion (°) | 60.57 ± 9.18 | 51.40 ± 11.10** |
| Cervical extension (°) | 74.26 ± 8.19 | 68.99 ± 9.15** |
| Cervical protrusion (cm) | 4.79 ± 1.33 | 4.91 ± 1.16 |
Values are mean ± SD. **significant difference, p < 0.01
Table 4. Habitual posture and craniocervical mobility of the normal and addiction groups according to subdiagnosis of TMDs.
| Normal group | Addiction group | |||||
|---|---|---|---|---|---|---|
| Joint | Muscular | Mixed | Joint | Muscular | Mixed | |
| Cervical flexion posture while using a smartphone (°) | 12.82±10.96 | 14.81±6.91 | 4.00±5.44 | 29.92±13.55** | 30.63±12.31** | 20.83±8.23** |
| Lateral flexion (Rt.) (°) | 4.75±1.3 | 4.67±1.23 | 4.40±1.49 | 5.14±1.25 | 4.81±0.96 | 4.69±1.16 |
| Lateral flexion (Lt.) (°) | 68.06±7.54 | 67.78±6.03 | 71.33±6.86 | 60.45±6.14** | 57.22±6.35** | 66.11±7.06 |
| Rotation (Rt.) (°) | 69.21±8.22 | 68.70±4.70 | 74.33±11.67 | 63.41±7.15* | 58.41±6.89** | 63.89±3.87 |
| Rotation (Lt.) (°) | 62.41±8.26 | 56.67±9.88 | 53.00±4.00 | 54.55±11.07** | 47.62±8.98* | 53.33±12.62 |
| Cervical flexion (°) | 74.53±8.92 | 72.59±6.24 | 75.00±6.15 | 71.59±9.76 | 64.92±7.91* | 72.78±3.38 |
| Cervical extension (°) | 41.57±5.18 | 37.22±4.08 | 39.33±3.59 | 35.15±9.87** | 30.48±4.02** | 39.44±11.08 |
| Cervical protrusion (cm) | 43.52±6.11 | 40.19±5.58 | 42.33±3.43 | 37.65±8.36** | 33.73±4.85** | 40.00±9.28 |
Values are mean ± SD. *significant difference, p < 0.05. **significant difference, p < 0.01
Among the 100 participants, 58 teenagers were diagnosed as having TMDs with joint problems, 30 had TMDs with muscular problems, and 12 suffered from TMDs with mixed problems. In more detail: the normal group included 36 teenagers with joint problems, 9 with muscular problems, and 5 with mixed problems, while the addiction group had 22 teenagers with joint problems, 21 with muscular problems, and 7 with mixed problems (Table 5).
Table 5. Diagnostic profile of TMDs according to smartphone addiction.
| Normal group | Addiction group | Total | |
|---|---|---|---|
| Joint problem | 36 (72%) | 22 (44%) | 58 |
| Muscular problem | 9 (18%) | 21 (42%) | 30 |
| Mixed problem | 5 (10%) | 7 (14%) | 12 |
Values are numbers of subjects. Pearson’s χ2 test, p = 0.004 **
DISCUSSION
The term ‘smartphone’ is generally used to characterize a wireless telephone with a specially computerized system that enables its users to communicate, send e-mails, and access the internet in real-time. The number of smartphone users has sharply increased from 5 million in 2010 to more than 40.12 million in 2014, indicating an extremely high penetration rate (79.6%) in Korea. The sharply increasing number of users is considered to be closely related to the convenience and multifunctionality of smartphones and the well-established internet infrastructure in Korea1). The National Information Agency (NIA) has reported that SNS using a smartphone was recently considered as an essential means of communication by 74.1% of the Korean population, as evidenced by daily usage of Kakao talk®, the most popular application for social networking in Korea, with over 500 million text messages sent daily in the country alone18). However, as the numbers of smartphone users have rapidly increased, physical, psychological, and even social issues have also been identified in conjunction with excessive smartphone use.
Smartphone addiction was defined as the excessive, uncontrollable and damaging use of a smartphone with neurotic dependency upon the smartphone and its related services, subsequently leading to a state of being enslaved to it2). A recent NIA survey suggested that the smartphone was more addictive than other digital media due to its higher addiction rate compared to other devices. Furthermore, the Korean government revealed that about one in five teenagers (18.4%) is addicted to his or her smartphone, a rate that is twice as high as that seen in adults (9.1%). Addicted teenagers use their smartphones with a daily usage frequency of 23 times, and duration of 7.3 hours4).
Interestingly, the upper cervical discomfort frequently observed in smartphone-addicted teenagers is considered an emerging problem among many educators and clinicians. Several studies have suggested the possible effects of smartphone usage on craniocervical mobility and habitual posture10, 11). However, previous findings still remain insufficient for determining the smartphone’s specific impact on teenagers. Moreover, considering the proposed role of poor craniocervical posture on the initiation and progression of TMDs in previous studies, it is also clinically important to clarify the effect of smartphone usage in TMDs19). No study has examined the relationship between smartphone use and TMDs. To the best of our knowledge, this topic has not yet been investigated.
To date, several questionnaires have been developed to identify smartphone addiction. In December 2013, the SAS-SV for adolescents was published, and it has several advantages over other questionnaires. First, the SAS-SV was developed using a process in which the participants completed the questionnaire and then receive a consultation from a clinical psychologist. Second, the cut-off value was determined based on the consultation results. Third, the inventory has a high sensitivity (0.867 for boys, 0.875 for girls) and a high specificity value (0.893 for boys and 0.886 for girls). Fourth, the 33 questions that were used in the original SAS were deemed inefficient for assessing teenagers due to the large number of questions; the SAS also has limitations in diagnosing addiction because no cut-off values were suggested. Fifth, the cut-off value for the Smartphone Addiction Proneness Scale (SAPS), which consists of 15 questions, was suggested through a statistical method but not via consultation with psychologist. Moreover, this cut-off value did not exhibit gender differences. Therefore, the SAS-SV was considered to be a more appropriate tool for evaluating smartphone addiction, especially among teenagers.
This study revealed that the addicted teenagers used their smartphones in a more flexed craniocervical posture. This postural alteration is thought to be closely related to the compact size of smartphones, which likely attracts the eyes of users closer to its screen. Interestingly, a recent study also reported that populations that used a relatively small screen adopted a head and neck posture with greater neck flexion20). In addition, a different study revealed that the usage of a tablet PC by children not only resulted in a more frequently misaligned posture but also altered the muscle tone in the trapezius and cervical vertebra erector muscles to a greater extent than that observed when the children used a desktop computer21). Longer daily usage durations and increased frequencies result in more craniocervical posture changes8, 22). Many studies have demonstrated that the load on the cervical spine is dramatically increased in a flexed head posture23). The cervical load increases from about 10 pounds in the neutral position to 60 pounds at 60 degrees23). Therefore, the excessive cervical load of a more flexed posture might cause considerable damage to the tissues that support the head and neck, including the muscles, ligaments, and joints, subsequently predisposing the addicted teenagers to craniocervical dysfunction and pain.
This study found that the cervical range of motion of the smartphone-addicted teenagers significantly decreased in almost every direction. This finding suggests that smartphone addiction has a deleterious influence on craniocervical mobility. Several other studies have also found that cervical motion range is decreased in visual display terminal (VDT) workers24,25,26). So et al. found that 20 minutes of smartphone usage caused a significant decrease in the median frequency of electromyogram (EMG) activity in the cervical erector spinae and the upper trapezius11). They suggested that these findings indicate fatigue in the cervical muscles responsible for maintaining an erect cervical posture, which likely caused the more flexed cervical posture and imbalanced tones between the cervical muscles after prolonged usage of a smartphone. Interestingly, Nakazawa et al. reported that physical symptoms, including neck and back pain, became more prevalent with daily exposure to digital media for periods longer than 3 hours27). Therefore, the limited cervical range of motion of addicted teenagers might be the result of a disturbance in cervical muscles caused by poor habitual posture.
This study showed that there was no significant difference in the resting posture between teenagers with and without smartphone addiction. In this study, a cephalogram was used to measure the exact craniocervical posture to exclude the possibility of methodological errors from different thicknesses of soft tissue in photometric analysis and tense posture produced by the attachment of a transducer for three-dimensional motion analysis22). However, even though each subject was instructed to assume the resting posture, it was hard to define the exact posture that represented the resting condition using the cephalostat because the posture had a tendency to vary easily due to environmental conditions and the patient’s emotional state. Moreover, a widely accepted method for determining the representative resting posture has not been available until recently. Therefore, the findings of this study regarding resting posture appear to be limited by possible methodological shortcomings.
Although TMDs are commonly found in teenagers, this study identified a significant difference in the TMD diagnostic profile between the normal and the smartphone addiction groups. TMD patients with smartphone addiction had a significantly higher proportion of myogenous TMDs than those without addiction. Interestingly, additional comparisons of craniocervical function according to subdiagnosis of TMD showed that smartphone addiction caused the most significant alteration in craniocervical function among all the TMD groups, except for the mixed group. These findings suggest that excessive use of a smartphone may influence the development and progression of TMDs, especially muscular problems. Many studies have found that poor habitual posture, such as a forward or flexed head posture, has an adverse effect on TMD occurrence14, 19, 28). Fricton et al. reported that myogenous TMD patients were frequently plagued by poor postures, such as a forward head posture (85% of patients) or round shoulders (82%)29). Furthermore, another study also suggested that there is a significant association between neck pain and temporomandibular symptoms30). Subjects with cervical muscle pain showed a significantly greater decrease in the median frequency of EMG in the cervical erector spinae and the upper trapezius after 20 minutes of smartphone use11). The same study also reported that the pressure-pain threshold in painful subjects was significantly decreased in the measured cervical muscles11). Moreover, the severity of the neck disability had a strong positive correlation with the daily duration of smartphone usage and the average one-time usage duration10). Overall, smartphone addiction among teenagers may have contributed to the onset and progression of myogenous symptoms among TMDs. However, it was difficult for the detailed effect of smartphone addiction to be clarified in this study due to excessively diverse symptoms, and the subsequent variety of subdiagnoses.
Previous studies have revealed that daytime clenching frequently occurs while concentrating on something31). Furthermore habitual clenching is considered as one of the most important causes of TMDs32). Accordingly, smartphone addiction may cause excessively prolonged contraction of masticatory muscles including the masseter and temporalis muscles. In addition, prolonged and repeated noxious stimuli during cervical muscle fatigue are known to trigger central sensitization33). Recent studies have shown that central sensitization might be closely related to myogenous TMDs, possibly by secondary hyperalgesia or referred pain of masticatory muscles33). Overall, fatigue of cervical muscles due to prolonged smartphone usage may play a causal role in the development and progression of myogenous TMDs.
Finally, this study suggests that teenagers should be properly instructed on smartphone usage to preserve craniocervical function and also to prevent myogenous TMDs. Fortunately, the American Academy of Pediatrics and the Canadian Society of Pediatrics published guidelines in 2014 that suggests parents restrict children between 6–18 years of age to no more than 2 hours of digital media, such as a computer or smartphone, a day34). It will be necessary to clarify the detailed effect of smartphone addiction on the initiation of myogenous TMDs by analyzing the interaction between craniocervical and masticatory muscles while using a smartphone.
Appendix 1
Smartphone Addiction Scale—Short Version Questionnaire
REFERENCES
- 1.Nielsen Korea and KT Economic Management Research Institute: Oct. 2014.
- 2.Lee WJ: An exploratory story on addictive use of smartphone: Developing SAUS (smartphone addictive use scale). J Convergence Info Tech, 2013, 8: 403–407. [Google Scholar]
- 3.National Information Society Agency: 2011 Internet Addiction Survey. Seoul: National Information Society Agency, 2012, pp 118–119. [Google Scholar]
- 4.Ministry of Science, ICT and Future planning: 2012.
- 5.Park C, Park YR: The conceptual model on smartphone addiction among early childhood. Int J Soc Sci Humanit, 2014, 4: 147–150. [Google Scholar]
- 6.Kim H: Exercise rehabilitation for smartphone addiction. J Exerc Rehabil, 2013, 9: 500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korpinen L, Pääkkönen R: Physical symptoms in young adults and their use of different computers and mobile phones. Int J Occup Saf Ergon, 2011, 17: 361–371. [DOI] [PubMed] [Google Scholar]
- 8.Kim SH, Kim KU, Kim JS: Changes in cervical angle according to the duration of computer use. J Korean Soc Phys Med, 2013, 7: 179–187. [Google Scholar]
- 9.Bae SS, Kim BJ, Lee KH: A study of muscle imbalance of head, cervical and shoulder region. J Korean Soc Phys Ther, 2001, 13: 769–776. [Google Scholar]
- 10.Lee JI, Song HS: The correlation analysis between hours of smartphone use and neck pain in the Gachon university students. Acupunct, 2014, 31: 99–109. [Google Scholar]
- 11.So YJ, Woo YK: Effects of smartphone use on muscle fatigue and pain and, cervical range of motion among subjects with and without neck muscle pain. Phys Ther Korea, 2014, 21: 28–37. [Google Scholar]
- 12.Wright EF, Domenech MA, Fischer JR, Jr: Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc, 2000, 131: 202–210. [DOI] [PubMed] [Google Scholar]
- 13.Evcik D, Aksoy O: Correlation of temporomandibular joint pathogenesis, neck pain and postural differences. J Phys Ther Sci, 2000, 12: 97–100. [Google Scholar]
- 14.Zonnenberg AJ, Van Maanen CJ, Oostendorp RA, et al. : Body posture photographs as a diagnostic aid for musculoskeletal disorders related to temporomandibular disorders (TMD). Cranio, 1996, 14: 225–232. [DOI] [PubMed] [Google Scholar]
- 15.Kwon M, Kim DJ, Cho H, et al. : The smartphone addiction scale: development and validation of a short version for adolescents. PLoS ONE, 2013, 8: e83558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D’Attilio M, Epifania E, Ciuffolo F, et al. : Cervical lordosis angle measured on lateral cephalograms; findings in skeletal class II female subjects with and without TMD: a cross sectional study. Cranio, 2004, 22: 27–44. [DOI] [PubMed] [Google Scholar]
- 17.Swinkels RA, Swinkels-Meewisse IE: Normal values for cervical range of motion. Spine, 2014, 39: 362–367. [DOI] [PubMed] [Google Scholar]
- 18.Han HH: The effect of smartphone addiction on mental health and physical health in college students; Moderating effect of self-efficacy, parent-child relationships, and friendship. A thesis for a doctorate, 2015.
- 19.Sonnesen L, Bakke M, Solow B: Temporomandibular disorders in relation to craniofacial dimensions, head posture and bite force in children selected for orthodontic treatment. Eur J Orthod, 2001, 23: 179–192. [DOI] [PubMed] [Google Scholar]
- 20.Bababekova Y, Rosenfield M, Hue JE, et al. : Font size and viewing distance of handheld smart phones. Optom Vis Sci, 2011, 88: 795–797. [DOI] [PubMed] [Google Scholar]
- 21.Straker LM, Coleman J, Skoss R, et al. : A comparison of posture and muscle activity during tablet computer, desktop computer and paper use by young children. Ergonomics, 2008, 51: 540–555. [DOI] [PubMed] [Google Scholar]
- 22.Kim YG, Kang MY, Kim JW, et al. : Influence of the duration of smartphone usage on flexion angles of the cervical and lumbar spine and on reposition error in the cervical spine. Phys Ther Kor, 2013, 20: 10–17. [Google Scholar]
- 23.Hansraj KK: Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int, 2014, 25: 277–279. [PubMed] [Google Scholar]
- 24.Yoo WG, An DH: The relationship between the active cervical range of motion and changes in head and neck posture after continuous VDT work. Ind Health, 2009, 47: 183–188. [DOI] [PubMed] [Google Scholar]
- 25.Yoo WG, Park SY, Lee MR: Relationship between active cervical range of motion and flexion-relaxation ratio in asymptomatic computer workers. J Physiol Anthropol, 2011, 30: 203–207. [DOI] [PubMed] [Google Scholar]
- 26.Yoo WG: Comparison of cervical range of motion and cervical FRR between computer users in their early and late 20s in Korea. J Phys Ther Sci, 2014, 26: 753–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakazawa T, Okubo Y, Suwazono Y, et al. : Association between duration of daily VDT use and subjective symptoms. Am J Ind Med, 2002, 42: 421–426. [DOI] [PubMed] [Google Scholar]
- 28.Nishiyama A, Kino K, Sugisaki M, et al. : A survey of influence of work environment on temporomandibular disorders-related symptoms in Japan. Head Face Med, 2012, 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fricton JR, Kroening R, Haley D, et al. : Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol, 1985, 60: 615–623. [DOI] [PubMed] [Google Scholar]
- 30.Ciancaglini R, Testa M, Radaelli G: Association of neck pain with symptoms of temporomandibular dysfunction in the general adult population. Scand J Rehabil Med, 1999, 31: 17–22. [DOI] [PubMed] [Google Scholar]
- 31.Mizumori T, Kobayashi Y, Inano S, et al. : No effect of conscious clenching on simple arithmetic task in healthy participants. J Prosthodont Res, 2011, 55: 189–192. [DOI] [PubMed] [Google Scholar]
- 32.Michelotti A, Cioffi I, Festa P, et al. : Oral parafunctions as risk factors for diagnostic TMD subgroups. J Oral Rehabil, 2010, 37: 157–162. [DOI] [PubMed] [Google Scholar]
- 33.Woolf CJ: Central sensitization: implications for the diagnosis and treatment of pain. Pain, 2011, 152: S2–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rowan C: 10 Reasons why handheld devices should be banned for children under the age of 12. March, 2014. American Academy of Pediatrics and the Canadian Society of Pediatrics, (AAP 2001/13, CPS 2010).