Abstract
Abnormal nocturnal behavior can have many causes, including primary sleep disorder, nocturnal seizures, and underlying medical or neurological disorders. A 79-year-old woman with type 2 diabetes was admitted for evaluation of abnormal nocturnal behavior. Every night at around 04:30 she was observed displaying abnormal behavior including leg shaking, fumbling with bedclothes, crawling around the room with her eyes closed, and non-responsiveness to verbal communication. Polysomnography with 20-channel electroencephalography (EEG) was performed. EEG showed that the posterior dominant rhythm was slower than that observed in the initial EEG, with diffuse theta and delta activities intermixed, and no epileptiform activity. The serum glucose level was 35 mg/dL at that time, and both the EEG findings and clinical symptoms were resolved after an intravenous injection of 50 mL of 50% glucose. These results indicate that nocturnal hypoglycemia should be considered as one of the possible etiologies in patients presenting with abnormal nocturnal behavior.
Citation:
Yang KI, Kim HK, Baek J, Kim DE, Park HK. Abnormal nocturnal behavior due to hypoglycemia in a patient with type 2 diabetes. J Clin Sleep Med 2016;12(4):627–629.
Keywords: abnormal nocturnal behavior, hypoglycemia
INTRODUCTION
Abnormal nocturnal behavior can be caused by various conditions, including primary sleep disorder, nocturnal seizures, and underlying medical or neurological disorder. These can be differentiated by the clinical presentation, associated medical conditions, and polysomnography (PSG) with extended electroencephalography (EEG).1 We report the case of a patient with type 2 diabetes who presented with abnormal nocturnal behavior due to hypoglycemia and describe the EEG findings during an ictal episode.
REPORT OF CASE
A 79-year-old woman with type 2 diabetes was admitted for evaluation of abnormal nocturnal behavior. Her medication regimen consisted of 28 IU of insulin glargine once a day, 500 mg of metformin twice a day, and 4 mg of glimepiride before breakfast and 2 mg before dinner. Other medications were not significant. Her spouse had witnessed her nocturnal behavior during the 2 months prior to admission. Every night at around 04:30 she was observed to display abnormal behavior such as shaking of legs, fumbling with bedclothes in a strange manner, crawling around the room with her eyes closed, and non-responsiveness to verbal communication. However, after waking later in the morning she could not remember these episodes. Her spouse fed her chocolate, thinking these behaviors might be due to hypoglycemia, which resulted in the symptoms improving 15 minutes later.
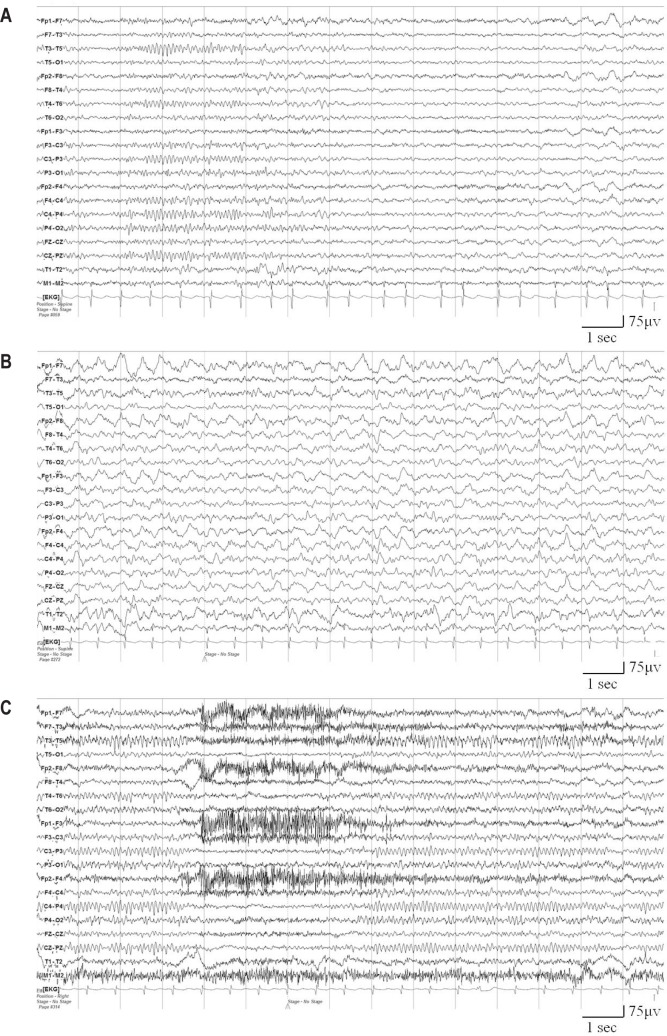
On admission, there was no evidence of any focal neurological deficit. Her glycated hemoglobin level was 7.7%, and the findings of other blood chemistry tests were unremarkable. Brain magnetic resonance imaging and abdominal computed tomography scanning did not show any abnormal findings. Video-PSG with 20-channel EEG monitoring (COMET PSG, Twin 4.5.2 software, Grass Technologies, Warwick, RI) was performed at 21:20. Two hours later she awoke spontaneously from stage 1 sleep, and video monitoring demonstrated her habitual behavior. During an episode she muttered incoherently and did not respond to verbal commands. EEG performed before an episode showed repetitive microarousal during stage 1 sleep and with the sleep stage shifting between brief periods of wakefulness and stage 1 sleep lasting several minutes. EEG during an episode showed that the posterior dominant rhythm was slower than that observed in the initial EEG, with diffuse theta and delta activities intermixed, and no epileptiform activity. The serum glucose level was 35 mg/dL at that time. An intravenous injection of 50 mL of 50% glucose terminated the patient's abnormal behaviors, with normal verbal communication now being possible, and with EEG recordings that were consistent with normal waking background activity (Figure 1).
Figure 1. Electroencephalography (EEG) findings.
(A) EEG performed before an episode shows normal waking background activities and stage 1 sleep. (B) During an episode the posterior dominant rhythm was slower than that observed in the initial EEG, with diffuse theta and delta activities intermixed, and no epileptiform activity. (C) The EEG findings returned to normal waking background activity after 1 and 2 minutes of intravenous glucose application.
After adjusting medication dosages to 14 IU of insulin glargine once a day, 500 mg of metformin twice a day, and 4 mg of glimepiride before breakfast, no additional episodes occurred during 1-year follow-up.
DISCUSSION
There have been previous reports of abnormal nocturnal behavior due to hypoglycemia, but no report from PSG with extended EEG performed during an episode. A patient with an insulinoma was reported to display abnormal behavior in the early morning at approximately 04:00,2 which was similar to the time of episodes in our patient. The habitual symptoms of the present case reportedly occurred around 04:30, but they occurred around midnight during the present sleep investigation. We speculate that the abnormal behavior appeared depending on the blood glucose level after dinner upon administering insulin glargine. In another study, sleepwalking was observed in a type 1 diabetic patient who had changed from 70/30 human insulin to a regimen of a basal bolus of glargine and lispro.3 Nocturnal hypoglycemia and sleepwalking resolved after the insulin glargine dosage was reduced. The symptoms in the present case also improved after adjusting the medication regimen. Type 2 diabetic patients who receive insulin become as susceptible to hypoglycemia as patients with type 1 diabetes,4 resulting in their also being at a risk of developing nocturnal hypoglycemia, which can cause abnormal behavior during sleep.
The present case showed abnormal EEG changes in a sleep state that are similar to those seen during daytime hypoglycemia, and the same blood glucose threshold as that in insulin-dependent diabetes.5,6 Decreased alpha activity was concomitant with increased theta activity, and a further lowering of blood glucose levels led to accentuation of the EEG changes and the occurrence of delta activity. These changes were probably due to glucose deprivation in brain neurons, or neuroglycopenia, since the EEG findings normalized after intravenous glucose injection. This intervention also improved her clinical condition.
The clinical history of the present case resembles that of a conversion disorder. However, ictal EEG findings are very important for distinguishing between a true epileptic episode, a conversion disorder, and a pathological condition. In the present case, abnormal EEG changes without epileptiform discharges and low blood glucose level were recorded during the abnormal nocturnal behavior. No additional episodes occurred during a 1-year follow-up after adjusting the diabetes medication of the patient.
The findings in this case indicate that nocturnal hypoglycemia should be considered in patients presenting with nocturnal abnormal behavior.
DISCLOSURE STATEMENT
This was not an industry supported study. This work was supported by the Soonchunhyang University Research Fund. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Provini F, Chokroverty S. Movement and behavioral disorders during sleep. Introduction. Sleep Med. 2011;12(Suppl 2):S2. doi: 10.1016/j.sleep.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 2.Suzuki K, Miyamoto M, Miyamoto T, Hirata K. Insulinoma with early-morning abnormal behavior. Intern Med. 2007;46:405–8. doi: 10.2169/internalmedicine.46.6071. [DOI] [PubMed] [Google Scholar]
- 3.Bell DS. Nocturnal hypoglycaemia presenting as somnambulism. Diabetologia. 2010;53:2066–7. doi: 10.1007/s00125-010-1842-5. [DOI] [PubMed] [Google Scholar]
- 4.Leese GP, Wang J, Broomhall J, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care. 2003;26:1176–80. doi: 10.2337/diacare.26.4.1176. [DOI] [PubMed] [Google Scholar]
- 5.Pramming S, Thorsteinsson B, Stigsby B, Binder C. Glycaemic threshold for changes in electroencephalograms during hypoglycaemia in patients with insulin dependent diabetes. Br Med J (Clin Res Ed) 1988;296:665–7. doi: 10.1136/bmj.296.6623.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tallroth G, Lindgren M, Stenberg G, Rosen I, Agardh CD. Neurophysiological changes during insulin-induced hypoglycaemia and in the recovery period following glucose infusion in type 1 (insulin-dependent) diabetes mellitus and in normal man. Diabetologia. 1990;33:319–23. doi: 10.1007/BF00403327. [DOI] [PubMed] [Google Scholar]