Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation that is not fully reversible. It is an incurable disease with improvement in quality of life (QOL) as a major focus area for management. This study assesses the QOL of COPD patients and the factors affecting it.
Materials and Methods:
All 124 patients diagnosed with COPD in a larger cross-sectional study to determine the prevalence of COPD were assessed for their QOL using St. George's respiratory questionnaire for COPD patients (SGRQ-C). Spirometry was performed to assess lung function and diagnose COPD. Chronic lung disease (CLD) severity index was used to assess the severity of symptoms and the Medical Research Council questionnaire was used to assess the severity of dyspnea. Sociodemographic data regarding the patients were also recorded.
Results:
Patients with COPD showed significantly reduced health-related quality of life (HRQOL). CLD estimate for severity of lung disease and the Medical Research Council assessment for dyspnea and the duration of illness showed a highly significant positive correlation with HRQOL. There was a statistically significant negative correlation between lung function and SGRQ-C score. Increasing age, increased quantum of smoking, and lower socioeconomic status were correlated with poorer HRQOL. No association between QOL and education, body mass index (BMI), and gender was observed.
Conclusion:
This study showed that Indian patients with COPD had reduced HRQOL. Poor lung function, increased disease duration and smoking, and worsening symptoms impacted HRQOL negatively.
KEY WORDS: Chronic obstructive pulmonary disease, India, quality of life, St. George's respiratory questionnaire for COPD patients
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a major public health problem. Across the world, as of 2010, COPD affected 329 million people or nearly 5% of the world's population.[1] In 2012, it ranked as the third leading cause of death, killing over 3 million people.[2] COPD is a noncurable disease, which progressively reduces breathing capacity and impairs patients’ ability to carry out activities of daily living, thereby adversely affecting health-related quality of life (HRQOL).[3]
Quality of life (QOL) is an important aspect for measuring the impact of chronic diseases. HRQOL measurement facilitates the evaluation of efficacy of medical interventions and also the detection of groups at risk of psychological or behavioral problems.[4] Many studies have been conducted across the world to study the HRQOL of COPD patients and the factors affecting it using both generic and disease-specific questionnaires.[3,5,6,7,8] However, studies from India and other developing nations are far fewer in number.
More importantly, most of the studies have been conducted in a hospital-based setting. This may be acceptable in developed nations where awareness and health care-seeking behavior is good but becomes important in developing countries such as India where people have poor health care-seeking behavior.[9,10] In COPD where the initial stages show none or few symptoms, patients may not approach hospitals in the early stages and they may be missed in hospital settings leading to an overall result which shows worse QOL. In recent times, care for patients with COPD has increasingly moved from hospitals to primary care.[11] COPD is a disease, which is mostly treated in home-based settings; so, it is better to assess the HRQOL of patients in a similar setting. Since HRQOL is an individual's own perception, it may be affected in a hospital-based setting. Also, patients may approach the health care provider because of exacerbation, which may further affect the results as QOL worsens during exacerbation.[12]
Taking these points into consideration, we decided to assess the HRQOL of COPD patients at their homes. This was made possible as this study was part of a larger study conducted by the same authors where we determined the prevalence of COPD in a spirometry-based cross-sectional study. The study conducted had the following objectives: 1) To assess the QOL of COPD patients using St. George's respiratory questionnaire for COPD patients (SGRQ-C) questionnaire 2) To determine the factors associated with the QOL of COPD patients. In order to understand the complexity of living with COPD, it is important that we understand which factors, in addition to physical functioning and complaints, are associated with HRQOL.
MATERIALS AND METHODS
This study was part of a larger community-based cross-sectional studyin which 1,220 subjects (aged ≥40 years) were studied to determine the prevalence of COPD in the rural and urban areas of Aligarh, Uttar Pradesh, India. The urban and rural field areas under the Department of Community Medicine of Jawaharlal Nehru Medical College were chosen as study areas. The study subjects were selected using systematic random sampling. Subjects were informed about the nature and consequences of the study and their consent was taken. All those above 40 years of age and who gave consent were included in the study. All those who refused spirometry or were not fit for it (those with recent myocardial infarction, stroke, eye surgery, thoracic/abdominal surgery, hemoptysis, known thoracic, aortic, or cerebral aneurysm, or uncontrolled hypertension) were excluded from the study. Diagnosis and staging were performed on the basis of GOLD standard.[13] Spirometry was conducted using a portable medical international research (MIR) SPIROLAB II spirometer (MIR Co., Italy). Spirometry was conducted as per the American Thoracic Society standards.[14] Of the 1,220 subjects studied, 124 were diagnosed with COPD (a prevalence of 10.2%). All the subjects diagnosed with COPD were assessed for their HRQOL using the SGRQ-C questionnaire.
SGRQ is a standardized, self-administered questionnaire for measuring impaired health and perceived HRQOL in airways disease. The SGRQ-C is a shorter version derived from the original version [St. George's respiratory questionnaire (SGRQ)] following a detailed analysis of data from large studies in COPD.[15] It contains 40 items compared with the original 50, with 76 weighted responses that cover three domains: Symptoms, activity, and impact.[16] In addition to the domain scores, a total score is calculated. Each item has an empirically derived weight. The SGRQ-C is scaled from 0 to 100; with 0 representing the best HRQOL. This instrument has been demonstrated to be valid, reliable, and responsive among patients with COPD.[16]
The chronic lung disease (CLD) severity index was used to quantify respiratory symptoms.[17] This is a short six-item questionnaire, which evaluates dyspnea, wheezing, and productive cough. Raw scores were added and transformed to a scale from 0 (normal) to 100 (most severe). The Medical Research Council (MRC) five-point scale for breathlessness was used to assess dyspnea.[18]
Patients were inquired about their duration of illness, smoking status, and duration of smoking. Pack years of smoking were calculated for smokers. The height and weight were recorded to calculate body mass index (BMI).
Sociodemographic information was also collected from every patient, which included age, sex, education, socioeconomic status, occupation, and area of residence (rural or urban). Socioeconomic status was assessed using standard of living index (SLI). SLI was used in the National Family health Survey (NFHS)-2 and was created by assigning scores to a range of 30 household goods and assets, including the type of housing and toilet facilities, fuel used for cooking, and ownership of durable goods.[19]
Statistical analysis
Data entry and statistical analysis were performed using the Statistical Package for the Social Sciences (SPSS) software, version 17.0 (SPSS, Chicago, IL, USA). The mean and standard deviation of HRQOL scores were calculated. Relationship between HRQOL scores and continuous variables were assessed using Spearman's correlation coefficient (r). For assessing the relationship between categorical variables and HRQOL scores, Kruskal-Wallis test was used. P value of < 0.05 was considered statistically significant.
RESULTS
The patients’ demographic and clinical profiles are shown in Table 1. The mean age of COPD patients was 61 years. Out of the total 124 diagnosed cases of COPD, 86 (69.4%) were males, 76 (61.3%) were from rural areas, 68 (54.8%) were practicing Hinduism, 102 (82.3%) were illiterate, all 38 (30.6%) females were homemakers, 80 (65.5%) were either current or past smokers with a mean pack years of smoking of 56 [Table 1].
Table 1.
Demographic and clinical profiles of study subjects
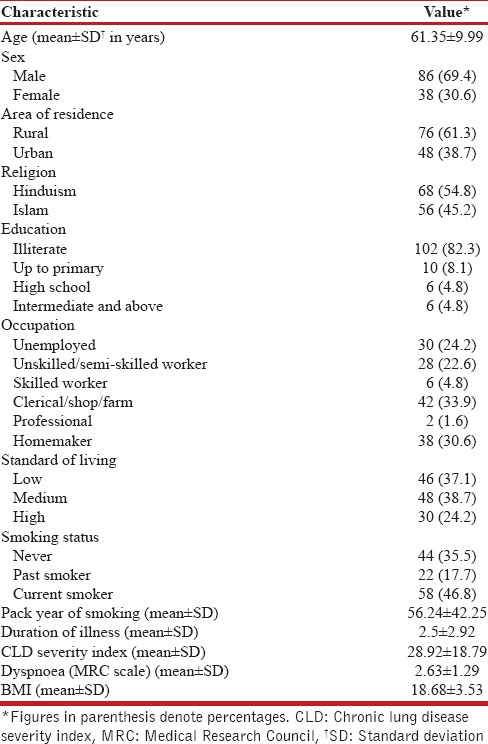
The mean BMI of patients was 18.9 kg/m2. Clinical characteristics showed a mean duration of illness of 2.5 years, a mean CLD index of 29, and a dyspnea severity score of 2.6 [Table 1].
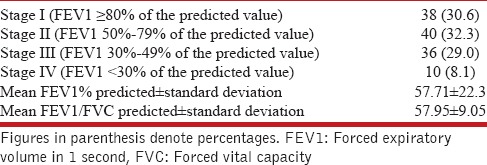
Spirometry showed that 38 (30.6%) subjects were GOLD Stage I, 40 (32.3%) were Stage II, 36 (29.0%) were Stage III, and 10 (8.1%) were Stage IV [Table 2].
Table 2.
Spirometry results of the study subjects
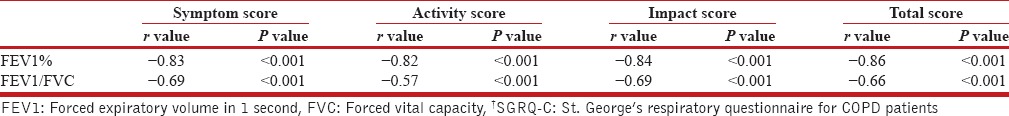
The mean symptom, activity, impact, and total score observed were 49.54, 41.47, 33.53, and 38.89, respectively. The scores showed significant impairment in all three domain measures, i.e., symptoms, activity, and impact, when compared with reference values [Table 3]. Significant negative correlation was found between lung function as measured by spirometry and QOL scores across all domains [Table 4].
Table 3.
Quality of life scores of COPD† patients
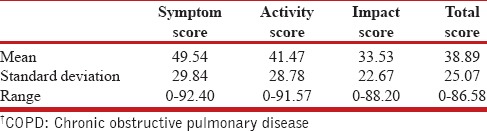
Table 4.
Correlation of lung function with SGRQ-C† scores
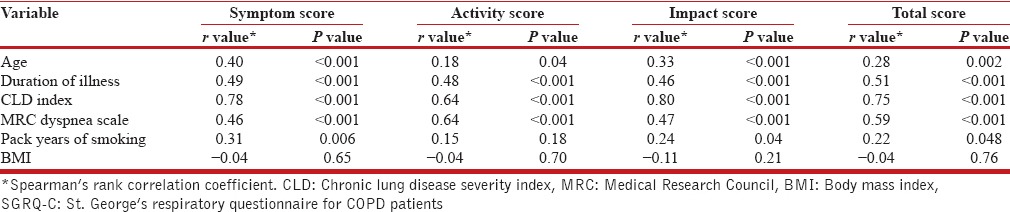
Age, duration of illness, CLD index, dyspnea grade, and exposure index had a statistically significant positive correlation with QOL scores across all domains. Pack years of smoking had a statistically significant positive correlation across all domains of QOL scores except the domain of activity. BMI was not found to have a statistically significant correlation with QOL scores [Table 5].
Table 5.
Correlation of continuous variables with SGRQ-C scores
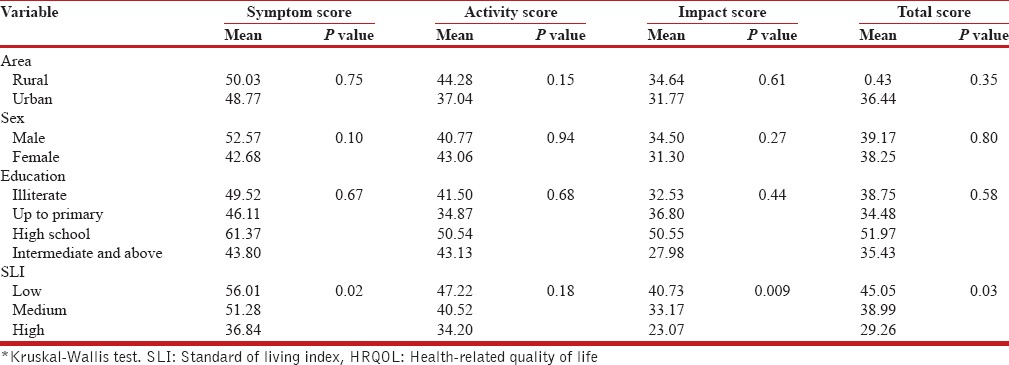
Standard of living was found to have a statistically significant association with QOL scores except the activity domain. Area of residence, education, and gender did not affect the QOL scores in a statistically significant manner [Table 6].
Table 6.
Association of HRQOL with categorical variables*
DISCUSSION
The study showed an impaired QOL among 124 COPD patients using a disease-specific questionnaire (SGRQ-C). QOL was impaired across all domains; however, symptom domain was the most affected while impact domain was the least affected. This study highlights that Indian COPD patients suffer somewhat similar reductions in QOL as do COPD patients from other countries, as reported previously.[3,5,8,20,21,22,23,24] These scores were lower than some other studies conducted in India.[25,26,27] This could be due to the fact that these studies were conducted in a hospital-based setting compared to a home-based setting in our study. Since HRQOL is an individual's own perception, it may be affected in a hospital-based setting. In our study, 78 of the 124 patients were suffering from Stage I or Stage II disease with many of them diagnosed for the first time; this was possible because of the community-based cross-sectional nature of our study. In COPD where the initial stages show none or few symptoms, patients may not approach hospitals in the early stages and may be missed leading to an overall result, which shows worse QOL. Also, the patients in hospitals may be there because of exacerbation, which may lead to worsening of QOL.[12] COPD is a disease, which is mostly treated in home-based settings; so, it is better to assess their HRQOL in a similar setting.
Lung functions as measured by forced expiratory volume in 1 s (FEV1) and ratio of FEV1 and forced vital capacity (FVC), i.e., FEV1/FVC showed that the poorer the lung function, the lower the patient's QOL. This association was anticipated and has been reported in multiple studies.[20,27,28,29] As grading COPD in various stages of severity is based on FEV1%, these findings also indicate that severe stages of COPD are having poorer QOL. Dignani et al. have also reported that the advancing stages of COPD lead to worsening of QOL.[30] Also, all the domains of QOL were impacted by deteriorating lung function. As lung function deteriorates daily, the activity is hampered leading to poor QOL. HRQOL showed significant correlation with CLD scores and dyspnea. Similar results have been reported in earlier studies.[23,27,29,31]
Smoking had a significant correlation with QOL score. As pack years of smoking increased QOL worsened. Various authors have reported similar results.[23,27,32] Smoking is a known etiological agent for COPD and increased exposure leads to severe stages of disease leading to poor QOL. Smoking has also been shown to independently impact QOL in a negative way regardless of the presence of COPD.[21] Authors have reported that smoking cessation has been shown to improve QOL scores and a reduction in symptoms related to COPD.[33] This highlights the necessity for active interventions by health professionals to help COPD patients quit smoking as a primary tool for the adequate management of COPD and the patient's QOL.
The duration of illness impacted QOL in a negative way. Longer the duration of the disease, worse was the QOL. Other authors have also reported similar findings.[23,28] BMI was not found to impact the QOL of COPD patients. Previous studies have shown varied results in this regard. Some have shown that underweight patients have worse health status than patients of normal weight;[32] similar to us, some have mentioned no association[34] while others have shown that overweight patients have worse QOL.[35]
Among sociodemographic variables, age and socioeconomic status had a significant impact on QOL. With increasing age, QOL worsened. However, the results by other authors in this regard are mixed. Some have shown results similar to us,[20,23,32] with many reporting no correlation between age and QOL.[29,34] Some have even reported that younger patients had worse health status.[35] Other authors have also found poor socioeconomic status to be adversely affecting QOL.[36] The reason can be poor care-seeking attitude and compliance with treatment as COPD requires regular and costly treatment, which poor people may find difficult to afford.
Area of residence, gender, and education did not impact QOL in a significant manner. Gender has been shown to impact QOL in many studies with females reporting poor QOL.[20,31] However, similar to us, some other authors have shown that gender plays no role in the QOL of COPD patients.[29,37] Education has been reported to impact QOL scores but was it was not so in this study.[20,32] The reasons for these are not apparent from our data but may be due to the different social structure and appreciation of education among the Indian population. This is an area that warrants further research.
The limitations of this study were its small sample size. Also, one major drawback is that we did not look for other comorbidities, which may also impact QOL as has been shown in previous studies.[20,32]
CONCLUSION AND RECOMMENDATIONS
QOL is impaired in patients with COPD and it worsens with increasing severity of the disease. Worsening lung function, increasing age and duration of illness, severity of symptoms, worsening dyspnea, and lower socioeconomic state led to decreased QOL in COPD patients. As COPD is a slowly progressive illness, which is incurable and the amount of improvement in lung function is minimal we need to increase our focus on potentially more treatable aspects of QOL, which may lead to a much more effective care of COP patients. While evaluating of COPD patients, due importance needs to be given to QOL measurement similar to that given to pulmonary function test.
There is a need for further research to assess the impact of social and family support and pulmonary rehabilitation program on QOL of COPD patients in India. One major reason for COPD among females in developing nations such as India is the exposure to biomass fuels. In particular, for female patients the impact of pattern of biomass fuel exposure on QOL needs to be studied.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). The Top 10 Causes of Death. Fact Sheet No. 310. 2014. [Last accessed on 2014 Dec 15]. Available from: http://www.who.int/mediacentre/factsheets/fs310/en/
- 3.Jones PW, Prince M, Wijkstra PJ, Patel V, Saxena S, Maj M, et al. Quality of life in patients with chronic obstructive pulmonary disease. Eur Respir Mon. 2006;38:375–86. [Google Scholar]
- 4.Hawthorne G, Richardson J, Osborne R. The Assessment of Quality of Life (AQoL) instrument: A psychometric measure of health-related quality of life. Qual Life Res. 1999;8:209–24. doi: 10.1023/a:1008815005736. [DOI] [PubMed] [Google Scholar]
- 5.Arne M, Lundin F, Boman G, Janson C, Janson S, Emtner M. Factors associated with good self-rated health and quality of life in subjects with self-reported COPD. Int J Chron Obstruct Pulmon Dis. 2011;6:511–9. doi: 10.2147/COPD.S24230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones PW. Activity limitation and quality of life in COPD. COPD. 2007;4:273–8. doi: 10.1080/15412550701480265. [DOI] [PubMed] [Google Scholar]
- 7.Altenburg WA, Bossenbroek L, de Greef MH, Kerstjens HA, ten Hacken NH, Wempe JB. Functional and psychological variables both affect daily physical activity in COPD: A structural equations model. Respir Med. 2013;107:1740–7. doi: 10.1016/j.rmed.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Tsiligianni I, Kocks J, Tzanakis N, Siafakas N, van der Molen T. Factors that influence disease-specific quality of life or health status in patients with COPD: A review and meta-analysis of Pearson correlations. Prim Care Respir J. 2011;20:257–68. doi: 10.4104/pcrj.2011.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011;377:505–15. doi: 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makinen M, Waters H, Rauch M, Almagambetova N, Bitran R, Gilson L, et al. Inequalities in health care use and expenditures: Empirical data from eight developing countries and countries in transition. Bull World Health Organ. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- 11.Schermer T, van Weel C, Barten F, Buffels J, Chavannes N, Kardas P, et al. Prevention and management of chronic obstructive pulmonary disease (COPD) in primary care: Position paper of the European Forum for Primary Care. Qual Prim Care. 2008;16:363–77. [PubMed] [Google Scholar]
- 12.Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, et al. IMPAC Study Group. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: A 2 year follow up study. Thorax. 2004;59:387–95. doi: 10.1136/thx.2003.008730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. [Last accessed on 2014 Jan 14]. Available from: http://www.goldcopd.com .
- 14.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 15.Schünemann HJ, Griffith L, Jaeschke R, Goldstein R, Stubbing D, Austin P, et al. A comparison of the original chronic respiratory questionnaire with a standardized version. Chest. 2003;124:1421–9. doi: 10.1378/chest.124.4.1421. [DOI] [PubMed] [Google Scholar]
- 16.Jones PW, Forde Y. Division of Cardiac and Vascular Science. UK: St George's, University of London; [Last accessed on 2013 Mar 10]. St George's Respiratory Questionnaire for COPD Patients (SGRQ-C) Manual 2008. Available from: http://www.healthstatus.sgul.ac.uk/SGRQ_download/SGRQ-C%20Manual%202008.pdf . [Google Scholar]
- 17.Selim AJ, Ren XS, Fincke G, Rogers W, Lee A, Kazis L. A symptom-based measure of the severity of chronic lung disease: Results from the Veterans Health Study. Chest. 1997;111:1607–14. doi: 10.1378/chest.111.6.1607. [DOI] [PubMed] [Google Scholar]
- 18.Stenton C. The MRC breathlessness scale. Occup Med (Lond) 2008;58:226–7. doi: 10.1093/occmed/kqm162. [DOI] [PubMed] [Google Scholar]
- 19.Mumbai: International Institute for Population Sciences (IIPS); 2000. International Institute for Population Sciences (IIPS) and Macro International. National family Health Survey (NFHS-2) 1998-99; pp. 40–1. [Google Scholar]
- 20.Ferrer M, Alonso J, Morera J, Marrades RM, Khalaf A, Aguar MC, et al. Chronic obstructive pulmonary disease stage and health-related quality of life: The Quality of Life of Chronic Obstructive Pulmonary Disease Study Group. Ann Intern Med. 1997;127:1072–9. doi: 10.7326/0003-4819-127-12-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 21.Prigatano GP, Wright EC, Levin D. Quality of life and its predictors in patients with mild hypoxemia and chronic obstructive pulmonary disease. Arch Intern Med. 1984;144:1613–9. [PubMed] [Google Scholar]
- 22.Huijsmans RJ, de Haan A, ten Hacken NN, Straver RV, van’t Hul AJ. The clinical utility of the GOLD classification of COPD disease severity in pulmonary rehabilitation. Respir Med. 2008;102:162–71. doi: 10.1016/j.rmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 23.Miravitlles M, Molina J, Naberan K, Cots JM, Ros F, Llor C. EVOCA study. Factors determining the quality of life of patients with COPD in primary care. Ther Adv Respir Dis. 2007;1:85–92. doi: 10.1177/1753465807086097. [DOI] [PubMed] [Google Scholar]
- 24.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Oga T. Stages of disease severity and factors that affect the health status of patients with chronic obstructive pulmonary disease. Respir Med. 2000;94:841–6. doi: 10.1053/rmed.2000.0804. [DOI] [PubMed] [Google Scholar]
- 25.Sarkar SK, Basuthakur S, Das SK, Das A, Das S, Choudhury S, et al. Evaluation of correlation of BODE index with health-related quality of life among patients with stable COPD attending a tertiary care hospital. Lung India. 2015;32:24–8. doi: 10.4103/0970-2113.148434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumar S, Matreja PS, Gupta AK, Singh A, Garg P. To assess the quality of life (QOL) of caregivers and patients suffering from chronic obstructive pulmonary disease (COPD) J Aller Ther. 2012;S2:003. [Google Scholar]
- 27.Shavro SA, Ezhilarasu P, Augustine J, Bechtel JJ, Christopher DJ. Correlation of health-related quality of life with other disease severity indices in Indian chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2012;7:291–6. doi: 10.2147/COPD.S26405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andenaes R, Kalfoss MH, Wahl A. Psychological distress and quality of life in hospitalized patients with chronic obstructive pulmonary disease. J Adv Nurs. 2004;46:523–30. doi: 10.1111/j.1365-2648.2004.03026.x. [DOI] [PubMed] [Google Scholar]
- 29.Engstrom CP, Persson LO, Larsson S, Sullivan M. Health-related quality of life in COPD: Why both disease-specific and generic measures should be used. Eur Respir J. 2001;18:69–76. doi: 10.1183/09031936.01.00044901. [DOI] [PubMed] [Google Scholar]
- 30.Dignani L, Toccaceli A, Lucertini C, Petrucci C, Lancia L. Sleep and quality of life in people with COPD: A descriptive-correlational study. Clin Nurs Res. 2015 doi: 10.1177/1054773815588515. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 31.Martín A, Rodríguez-González Moro JM, Izquierdo JL, Gobartt E, de Lucas P. VICE Study Group. Health-related quality of life in outpatients with COPD in daily practice: The VICE Spanish Study. Int J Chron Obstruct Pulmon Dis. 2008;3:683–92. doi: 10.2147/copd.s4791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hesselink AE, van der Windt DA, Penninx BW, Wijnhoven HA, Twisk JW, Bouter LM, et al. What predicts change in pulmonary function and quality of life in asthma or COPD? J Asthma. 2006;43:513–9. doi: 10.1080/02770900600856954. [DOI] [PubMed] [Google Scholar]
- 33.Papadopoulos G, Vardavas CI, Limperi M, Linardis A, Georgoudis G, Behrakis P. Smoking cessation can improve quality of life among COPD patients: Validation of the clinical COPD questionnaire into Greek. BMC Pulm Med. 2011;11:13. doi: 10.1186/1471-2466-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Miguel Díez J, Izquierdo Alonso JL, Rodríguez González-Moro JM, de Lucas Ramos P, Bellón Cano JM, Molina París J. Quality of life with chronic obstructive pulmonary disease: The influence of level of patient care. Arch Bronconeumol. 2004;40:431–7. [PubMed] [Google Scholar]
- 35.Moy ML, Reilly JJ, Ries AL, Mosenifar Z, Kaplan RM, Lew R, et al. Multivariate models of determinants of health-related quality of life in severe chronic obstructive pulmonary disease. J Rehabil Res Dev. 2009;46:643–54. doi: 10.1682/JRRD.2008.09.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McSweeny AJ, Grant I, Heaton RK, Adams KM, Timms RM. Life quality of patients with chronic obstructive pulmonary disease. Arch Intern Med. 1982;142:473–8. [PubMed] [Google Scholar]
- 37.Medinas-Amorós M, Alorda C, Renom F, Rubí M, Centeno J, Ferrer V, et al. Quality of life in patients with chronic obstructive pulmonary disease: The predictive validity of the BODE index. Chron Respir Dis. 2008;5:7–11. doi: 10.1177/1479972307082329. [DOI] [PubMed] [Google Scholar]


