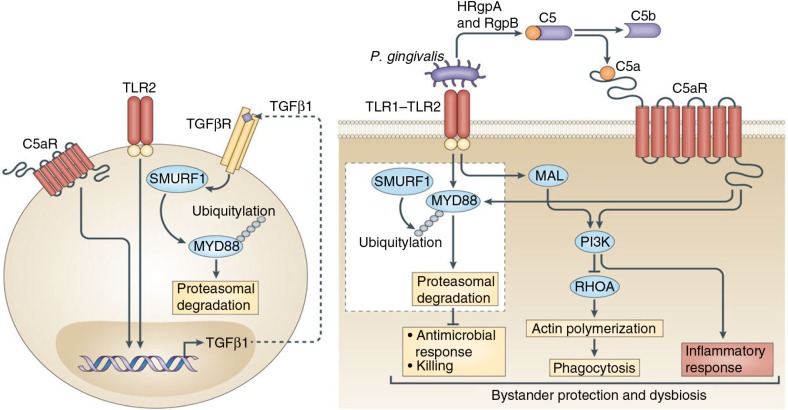
Fig. 1.
Porphyromonas gingivalis subverts neutrophils to evade killing while causing dysbiotic inflammation. P. gingivalis expresses ligands that activate the TLR2–TLR1 receptor complex (TLR2/1) and Arg-specific gingipains (HRgpA and RgpB gingipains), which cleave complement C5 and generate high local concentrations of C5a ligand. The ability of P. gingivalis to co-activate C5aR and TLR2 in human neutrophils results in a subversive crosstalk that leads to ubiquitylation and proteasomal degradation of the TLR2 adaptor MyD88, thereby blocking an antimicrobial response that would otherwise clear the pathogen. The proteolysis of MyD88 requires C5aR/TLR2-dependent release of the cytokine TGF-β1, which mediates ubiquitination of MyD88 via the E3 ubiquitin ligase Smurf1 (enlarged inset). In addition, the C5aR–TLR2 crosstalk activates PI3K, which inhibits phagocytosis by blocking the activity of RhoA GTPase and hence actin polymerization. PI3K signaling, moreover, induces the production of inflammatory cytokines. In contrast to MyD88, a second TLR2 adaptor, Mal, participates in this immune subversion strategy by acting upstream of PI3K. Together, these functionally integrated pathways, as controlled by P. gingivalis, offer ‘bystander’ protection to otherwise susceptible species in polymicrobial communities and promote dysbiotic inflammation and periodontal bone loss in relevant animal models. (From Ref. 20. Used with permission.)