Although many lymphomas can be reliably classified according to the World Health Organization Classification of 20081, the differentiation between nodal marginal zone lymphoma (NMZL) and follicular lymphoma (FL) is problematic in some cases. In fact, NMZL is often diagnosed by exclusion, resulting in heterogeneity in the diagnostic category of NMZL. New markers for NMZL have been described, but they have not yet been tested in combination.2,3 In this study, we compared multiple immunohistochemical markers for their use in distinguishing NMZL from FL. From the results obtained, we constructed an algorithm that combines these markers to help distinguish between FL and NMZL. Notably, this algorithm also contains a category of “B-cell lymphoma, unclassifiable”, thus underlining the difficulty that remains in distinguishing NMZL from FL.
For the initial test series, we selected 47 patients with FL with a chromosomal rearrangement of BCL2, and 44 patients with a diagnosis of NMZL or probable NMZL, from the archive of the Department of Pathology at the Radboud university medical center (Nijmegen, the Netherlands). For all NMZLs, BCL2 translocations were excluded using fluorescent in-situ hybridization with split-signal probes. Patient characteristics are described in Online Supplementary Table S1. For a diagnosis of NMZL, the following diagnostic criteria were used: 1) effaced architecture of the lymph node, due to a small B-cell proliferation with a follicular, marginal zone, or diffuse growth pattern, 2) either centrocytoid or more round cells with intermingled centroblasts, 3) a mature B-cell immunophenotype with expression of BCL2, 4) in cases with a follicular/ nodular growth pattern, signs of follicular colonization (presence of BCL2 negative cells and high Ki67 staining), 5) not fitting a diagnosis of chronic lymphocytic leukemia/small lymphocytic lymphoma, mantle cell lymphoma, or lymphoplasmacytic lymphoma. Expression of germinal center markers was not considered an exclusion criterion for a diagnosis of NMZL in this study.
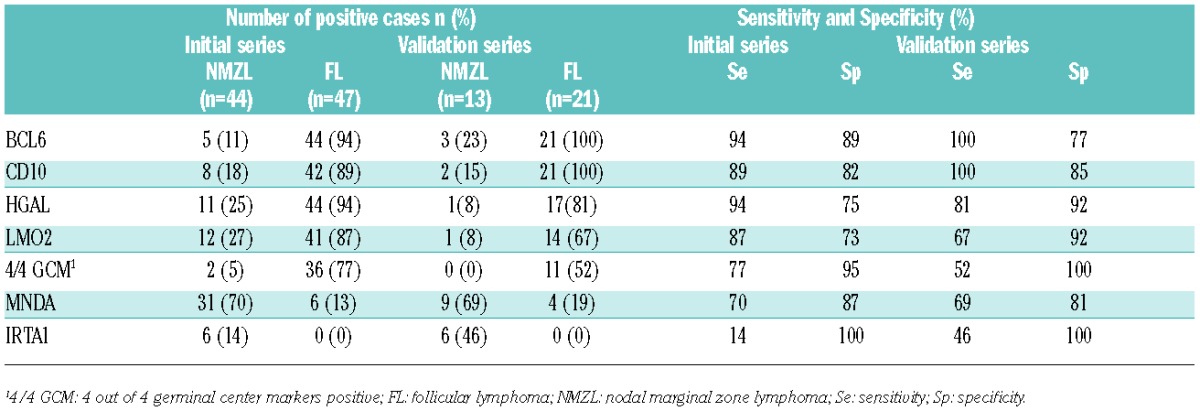
As expected, immunohistochemistry showed significant differences between NMZL and FL (Table 1). Overall, FLs were positive for germinal center markers (CD10, BCL6, LMO2, HGAL) and negative for MNDA and IRTA1 (Online Supplementary Figure S1). NMZLs mostly showed an opposite pattern with positivity for MNDA in approximately two thirds of cases, IRTA1 staining in approximately one fifth of cases and usually no staining with germinal center markers. However, all germinal center markers were positive in a subset of NMZLs, and similarly, FLs with expression of MNDA were also identified (Online Supplementary Figure S2).
Table 1.
Immunohistochemistry results.
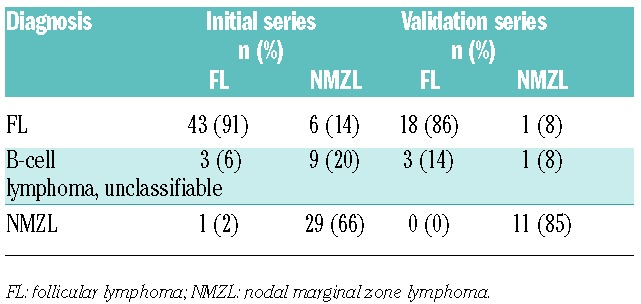
Based on the immunohistochemistry results, a combination of markers were used to design an algorithm that helped to distinguish NMZL from FL (Figure 1). This algorithm was built empirically, allowing inclusion of a category of “B-cell lymphoma, unclassifiable” to prevent contamination of the NMZL category. As expected, this algorithm classified most lymphomas according to their original diagnosis (Table 2). However, in the initial test series, one case of FL was classified as NMZL, and 6 cases of NMZL were classified as FL by the algorithm; a significant proportion of cases (13%) were considered “B-cell lymphoma, unclassifiable” by the algorithm. Most (75%) of these unclassifiable cases had an original diagnosis of NMZL.
Figure 1.
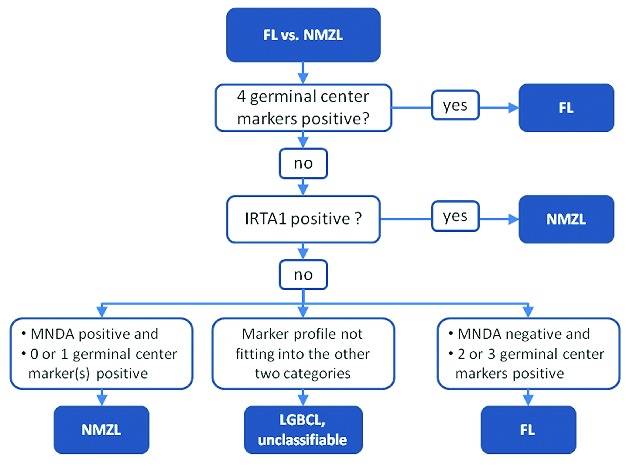
Immunohistochemical algorithm for separation of nodal marginal zone lymphoma (NMZL) from follicular lymphoma (FL). The algorithm starts at the top with a lymphoma that is considered to be either FL or NMZL. If all four germinal center markers (BCL6, CD10, LMO2, HGAL) are positive, a diagnosis of FL is made. If not, IRTA1 expression is determined. If IRTA1 is positive, a diagnosis of NMZL is made. If IRTA1 is negative, MNDA and germinal center markers are used to divide the remaining cases into three categories: NMZL for MNDA positive cases with positivity for none or only one germinal center marker, FL for MNDA negative cases with expression of 2 or 3 germinal center markers and low-grade B-cell lymphoma, unclassifiable for cases that do not fit into either of these two categories.
Table 2.
Algorithm results.
To validate the algorithm, a second validation group of 21 FLs and 13 NMZLs, collected from the archive of the Department of Pathology at the Hospital del Mar (Barcelona, Spain) was stained for the same markers as the initial group. Overall, staining results were comparable to those in the test group, with a high sensitivity of BCL6 for FL and a high specificity of IRTA1 for NMZL (Table 1); CD10 expression had a higher sensitivity in comparison to the test group, but a lower specificity. LMO2 and HGAL were less sensitive but more specific.
In this validation group, the algorithm gave a concordant classification as either NMZL or FL in 85% of cases (Table 2). No follicular lymphoma was misclassified as NMZL, and only one NMZL was misclassified as FL. Four cases (12%) were considered unclassifiable, three of which had an original diagnosis of FL and one with an original diagnosis of NMZL.
The algorithm was designed based on a comparison of NMZLs with FLs with a translocation involving BCL2. However, because a BCL2 translocation can be demonstrated relatively easily, the actual problem we are faced with in daily practice is the separation of NMZL from FL without a BCL2 translocation. FLs with and without a BCL2 translocation might be different from each other, as has been suggested by one gene expression study4, and also by a recent comparative genomic hybridization study.5 In the latter study, genetic aberrations in FLs without a BCL2 translocation bore more resemblance to those in NMZL than those in FLs with a BCL2 translocation. To address this problem, we tested a small series of 6 FLs without a BCL2 translocation, which were all classified as FL by the algorithm. This supports the idea that this algorithm also applies to FLs without a BCL2 translocation, but confirmation of this theory will require the study of a larger series.
Thus far, the majority of the markers in the algorithm has only been described in single studies. Kanellis and colleagues reported expression of MNDA in 75% of NMZLs versus 5% of FLs.2 In our series, a less pronounced, but similar difference was observed, with MNDA expression in NMZL and FL in 70% and 15%, respectively. In accordance with Falini and colleagues6, IRTA1 also discriminated between NMZL and FL in our series. However, in the study carried out by Falini et al.,73% of NMZLs expressed IRTA1, compared to only 21% in our study. This difference could be caused by a difference in interpretation. In our case, faint IRTA1 expression was quite frequently observed in NMZLs, but also in some FLs. As the reproducibility of the scores assigned to these cases proved to be very poor amongst different observers, a case was only considered positive if 30% or more of the cells showed moderate or strong expression of IRTA1. This aforementioned approach produced a strong improvement in the diagnostic value of IRTA1 in our series, and explains the small proportion of NMZLs positive for IRTA1.
Expression of the germinal center markers HGAL and LMO2 in lymphomas has been described by Natkunam et al., whose work showed expression in the majority of FLs and only very rare expression in NMZL.7–10 For both markers, they detected only a single case of NMZL that was positive.7,8 In our series, we observed more frequent expression of both LMO2 and HGAL in NMZL. We believe this could be caused by differences in inclusion criteria between our study and previous studies. In the study effected by Salama et al., which contains the largest majority of NMZLs previously studied for LMO2 and HGAL, cases were excluded from the NMZL group if they expressed germinal center markers9, which explains why expression of germinal center markers was not detected in NMZLs in their study. A recent study by Dyhdalo and colleagues reported LMO2 staining in 2 out of 25 NMZLs, of which one case also expressed BCL6.11 In our study, expression of germinal center markers was not considered an exclusion criterion. We made this choice because, in our experience, typical cases of NMZL do occasionally express germinal center markers and expression of CD10 and BCL6 in NMZL has been previously reported.12–14
The FLs that were used to build the algorithm were all required to have a BCL2 break, which, together with morphology, ensured that the diagnosis of FL was correct. Thus, misclassification of FL with a BCL2 break as NMZL has been excluded. Unfortunately, no markers for NMZL can compare with the BCL2 translocation for FL. Therefore, the NMZL group can still be expected to be more heterogeneous than the FL group, with some cases representing FL or other lymphomas rather than NMZL. Indeed, when looking at the initial and validation series together, ‘NMZLs’ were quite frequently considered FL (in 12%) or unclassifiable (in 18%) by the algorithm. This illustrates the difficulty that remains in the definition and diagnosis of NMZL; the lack of both an accurate definition and of positive diagnostic markers for NMZL result in a heterogeneous diagnostic category.
The ultimate question is: what is the gold standard? For this study we have used the combination of morphology and phenotyping for follicular colonization as defining criteria for NMZL. The addition of extensive immunohistochemistry, including new markers, might help to create a better gold standard for NMZL. At present, however, it is very difficult to compare different strategies to diagnose NMZL, due to the fact that as of yet no perfect positive marker for NMZL is available. Hopefully, elucidation of the pathogenesis of NMZL will provide us with better positive markers for NMZL. The results from this study could assist in achieving this goal; the addition of extensive immunohistochemistry to conventional criteria for NMZL will help to establish smaller, but potentially more homogeneous study groups, facilitating studies into the pathogenesis of NMZL.
Acknowledgments
The authors would like to thank dr. Roncador for providing the MNDA antibody.
Footnotes
Funding: this work was supported by grants from Instituto de Salud Carlos III FEDER (PT13/0010/0005), the “Xarxa de Bancs de Tumors sponsored by Pla Director d’Oncologia de Catalunya (XBTC)”.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer; 2008. [Google Scholar]
- 2.Kanellis G, Roncador G, Arribas A, et al. Identification of MNDA as a new marker for nodal marginal zone lymphoma. Leukemia. 2009; 23(10):1847–1857. [DOI] [PubMed] [Google Scholar]
- 3.Falini B, Tiacci E, Pucciarini A, et al. Expression of the IRTA1 receptor identifies intraepithelial and subepithelial marginal zone B cells of the mucosa-associated lymphoid tissue (MALT). Blood. 2003; 102(10):3684–3692. [DOI] [PubMed] [Google Scholar]
- 4.Leich E, Salaverria I, Bea S, et al. Follicular lymphomas with and without translocation t(14;18) differ in gene expression profiles and genetic alterations. Blood. 2009;114(4):826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krijgsman O, Gonzalez P, Ponz OB, et al. Dissecting the gray zone between follicular lymphoma and marginal zone lymphoma using morphological and genetic features. Haematologica. 2013; 98(12):1921–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falini B, Agostinelli C, Bigerna B, et al. IRTA1 is selectively expressed in nodal and extranodal marginal zone lymphomas. Histopathology. 2012;61(5):930–941. [DOI] [PubMed] [Google Scholar]
- 7.Natkunam Y, Lossos IS, Taidi B, et al. Expression of the human germinal center-associated lymphoma (HGAL) protein, a new marker of germinal center B-cell derivation. Blood. 2005;105(10):3979–3986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Natkunam Y, Zhao S, Mason DY, et al. The oncoprotein LMO2 is expressed in normal germinal-center B cells and in human B-cell lymphomas. Blood. 2007;109(4):1636–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salama ME, Lossos IS, Warnke RA, Natkunam Y. Immunoarchitectural patterns in nodal marginal zone B-cell lymphoma: a study of 51 cases. Am J Clin Pathol. 2009;132(1):39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Younes SF, Beck AH, Lossos IS, Levy R, Warnke RA, Natkunam Y. Immunoarchitectural patterns in follicular lymphoma: efficacy of HGAL and LMO2 in the detection of the interfollicular and diffuse components. Am J Surg Pathol. 2010;34(9):1266–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyhdalo KS, Lanigan C, Tubbs RR, Cook JR. Immunoarchitectural patterns of germinal center antigens including LMO2 assist in the differential diagnosis of marginal zone lymphoma vs follicular lymphoma. Am J Clin Pathol. 2013;140(2):149–154. [DOI] [PubMed] [Google Scholar]
- 12.Naresh KN. Nodal marginal zone B-cell lymphoma with prominent follicular colonization - difficulties in diagnosis: a study of 15 cases. Histopathology. 2008;52(3):331–339. [DOI] [PubMed] [Google Scholar]
- 13.Wang E, West D, Kulbacki E. An unusual nodal marginal zone lymphoma with bright CD10 expression: a potential diagnostic pitfall. Am J Hematol. 2010;85(7):546–548. [DOI] [PubMed] [Google Scholar]
- 14.Traverse-Glehen A, Felman P, Callet-Bauchu E, et al. A clinicopathological study of nodal marginal zone B-cell lymphoma. A report on 21 cases. Histopathology. 2006;48(2):162–173. [DOI] [PubMed] [Google Scholar]


