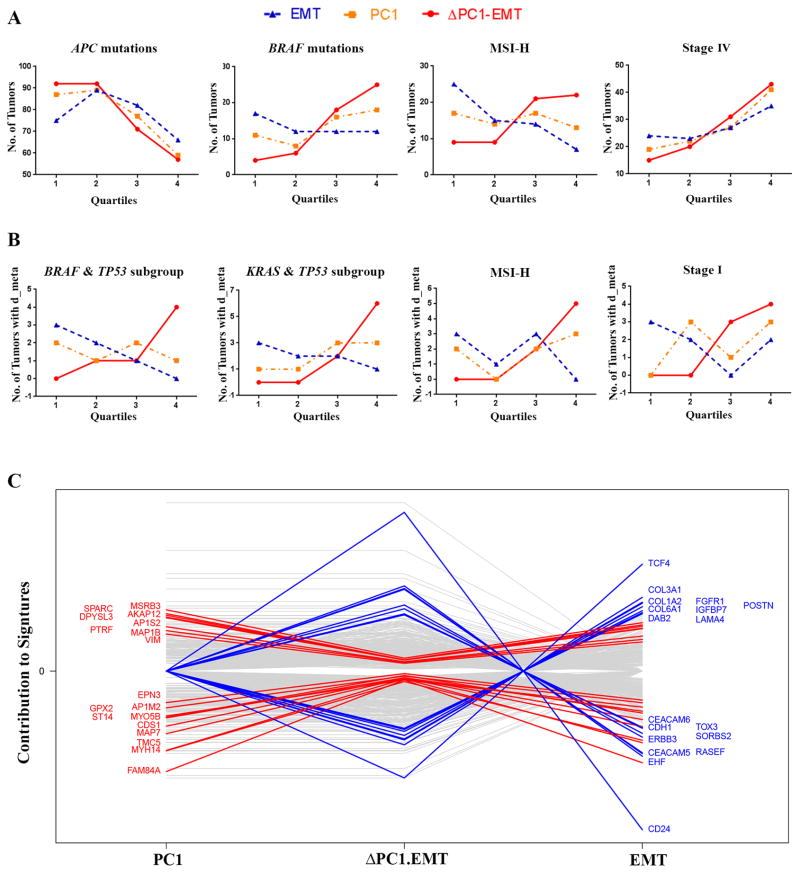
Figure 3. ΔPC1.EMT identified several subgroups of CRC and appeared to have propensity to measure non-EMT components of CRC.
(A and B) Analysis of quartile trends (from low 1st to high 4th quartiles) of ΔPC1.EMT, PC1 and EMT scores on the Moffitt468 dataset (for all patients). (A) The ΔPC1.EMT score trended well (relative to PC1 and EMT) with APC truncated mutation (downward) and BRAF V600E (upward), and with tumors identified as MSI-H (upward) and Stage IV (upward). See Supplementary Figure S9 for Stage I-III patients. (B) In the subgroups of combined mutations (KRAS&TP53 or BRAF&TP53) as well as in MSI-H and Stage I cases, ΔPC1.EMT and EMT trended in opposite directions with respect to the number of patients with distant metastases (d_meta). (C) Weighted analysis of individual genes contributing to PC1 and EMT vs. ΔPC1.EMT signatures on five datasets (PETACC3, ALMAC, LNCC, GEO41258, and GSE14333) datasets suggests that ΔPC1.EMT was represented by more non-EMT components when compared with the other two scores. The genes that were the most changed from EMT or PC1 to ΔPC1.EMT are highlighted.