Abstract
BACKGROUND
Recently, the Massachusetts Group Insurance Commission (GIC) prioritized research on the implications of a clause expressly prohibiting the denial of health insurance coverage for transgender-related services. These medically necessary services include primary and preventive care as well as transitional therapy.
OBJECTIVE
To analyze the cost-effectiveness of insurance coverage for medically necessary transgender-related services.
DESIGN
Markov model with 5- and 10-year time horizons from a U.S. societal perspective, discounted at 3 % (USD 2013). Data on outcomes were abstracted from the 2011 National Transgender Discrimination Survey (NTDS).
PATIENTS
U.S. transgender population starting before transitional therapy.
INTERVENTIONS
No health benefits compared to health insurance coverage for medically necessary services. This coverage can lead to hormone replacement therapy, sex reassignment surgery, or both.
MAIN MEASURES
Cost per quality-adjusted life year (QALY) for successful transition or negative outcomes (e.g. HIV, depression, suicidality, drug abuse, mortality) dependent on insurance coverage or no health benefit at a willingness-to-pay threshold of $100,000/QALY. Budget impact interpreted as the U.S. per-member-per-month cost.
KEY RESULTS
Compared to no health benefits for transgender patients ($23,619; 6.49 QALYs), insurance coverage for medically necessary services came at a greater cost and effectiveness ($31,816; 7.37 QALYs), with an incremental cost-effectiveness ratio (ICER) of $9314/QALY. The budget impact of this coverage is approximately $0.016 per member per month. Although the cost for transitions is $10,000–22,000 and the cost of provider coverage is $2175/year, these additional expenses hold good value for reducing the risk of negative endpoints —HIV, depression, suicidality, and drug abuse. Results were robust to uncertainty. The probabilistic sensitivity analysis showed that provider coverage was cost-effective in 85 % of simulations.
CONCLUSIONS
Health insurance coverage for the U.S. transgender population is affordable and cost-effective, and has a low budget impact on U.S. society. Organizations such as the GIC should consider these results when examining policies regarding coverage exclusions.
KEY WORDS: transgender health, cost-effectiveness analysis, budget impact analysis, preventive care, health law, health insurance coverage
INTRODUCTION
U.S. health insurance plans categorically deny transgender enrollees coverage for medically necessary services such as transition-related and preventive care.1
In 2013, the Commonwealth of Massachusetts Group Insurance Commission (GIC), the state’s administrator of employment-based health benefits to 420,000 subscribers, prioritized research on whether the cost-effectiveness of providing benefit coverage for transgender enrollees would support the removal of exclusions of coverage for transition-related services. Current evidence indicates that transition-related care is medically necessary and effective for transgender patients.2 , 3 Furthermore, recent changes in federal and state laws may place health insurer accreditation status at risk based on absence of coverage for transition-related care.4 , 5 Since negative health outcomes are associated with denial of these services, it may be in payers’ financial interests to cover transgender health benefits.2 Payers could increase net monetary benefit and avoid noncompliance with regulations by offering coverage in accordance with guideline-recommended care.3
The American College of Physicians' position on the health care of transgender persons is that all services should be covered as they would for other beneficiaries, and that coverage should not discriminate on the basis of gender identity.6 However, health insurance policies frequently prohibit coverage for transgender people under a clause expressly prohibiting coverage for transitional care, or based on carriers’ contract interpretation.7 Transgender exclusions result in denial of coverage when subscriber gender marker and physiology are incongruent.8
In 2014, the U.S. Department of Health and Human Services lifted a 33-year ban on coverage of transitional care for Centers for Medicare and Medicaid Services (CMS) beneficiaries, citing that existing literature demonstrates the efficacy, safety, and effectiveness of “sex reassignment surgery” and that “exclusions of coverage are not reasonable.”4 , 5 This stance stemmed from the U.S. Department of Justice’s interpretation of Title VII of the Civil Rights Act that sex discrimination prohibitions extend to health benefits of transgender people.9 This federal decision could influence how public and commercial payers define medically necessary services.
The most effective approach to transition uses individualized treatment plans,10 which may require hormone replacement therapy (HRT), mastectomy, phalloplasty, vaginoplasty, psychotherapy, or other services.8 The prevalence of sex reassignment surgery is 1:100,000 population, or approximately 3000–9000 in the U.S.4 , 8 In 2001, 866 male-to-female (MTF) primary surgeries (bottom surgery) and 336 female-to-male (FTM) primary surgeries (top surgery) were documented in the U.S., and the prevalence has likely increased since then, despite considerable under-reporting.4 , 8 , 11 These procedures are costly to uninsured patients. In addition, many costs for gender-specific preventive care (i.e., prostate screening, mammograms) are not covered by insurance if a patient legally changes their sex on their birth certificate.11 , 12 According to Gorton et al., providing insurance coverage would appear cost-effective,2 whereas negative outcomes associated with denial of coverage could be costly to payers because of increased morbidity.13 For instance, studies by Lundstrom and by Kuiper and Cohen-Kettenis estimated that suicidality in transmen dropped from 20 % to 1 % after treatment.14 , 15 No studies, however, have measured the economic benefit of health insurance coverage to transgender enrollees for medically necessary and preventive services.
Our objective was to analyze the cost-effectiveness of health insurance coverage for medically necessary and preventive services compared to no coverage in the U.S. adult transgender population. This study was designed from a U.S. societal perspective and evaluated outcomes over 5- and 10-year periods.16 We hypothesized that provider coverage is cost-effective.
METHODS
Study Design
Using a Markov model, we compared the cost-effectiveness of health insurance for provider coverage (i.e., access to primary, secondary, and tertiary services provided by a physician and/or advanced practitioner) of medically necessary services in the U.S. adult transgender population.17 , 18 Model parameters were extracted from the National Transgender Discrimination Survey (NTDS) of adults,1 and provider costs for transition-related care were extracted from the Healthcare Bluebook.19 Costs were adjusted to 2013 U.S. dollar values and discounted at 3 % along with utilities, and analyzed over 5 and 10 years.16
The analysis was conducted from a U.S. societal perspective. Effectiveness was measured as quality-adjusted life years (QALYs) derived from EuroQol Group EQ-5D index scores.20 Patient costs in the provider coverage arm were considered along with probabilities for negative outcomes and any associated costs for psychiatric rehabilitation. Patients in the provider coverage arm were assumed to receive individualized transition therapy.7 With no health benefit, patients were assumed to have lower upfront costs, but higher risks for negative outcomes, long-term costs, and lower life expectancy.
Model
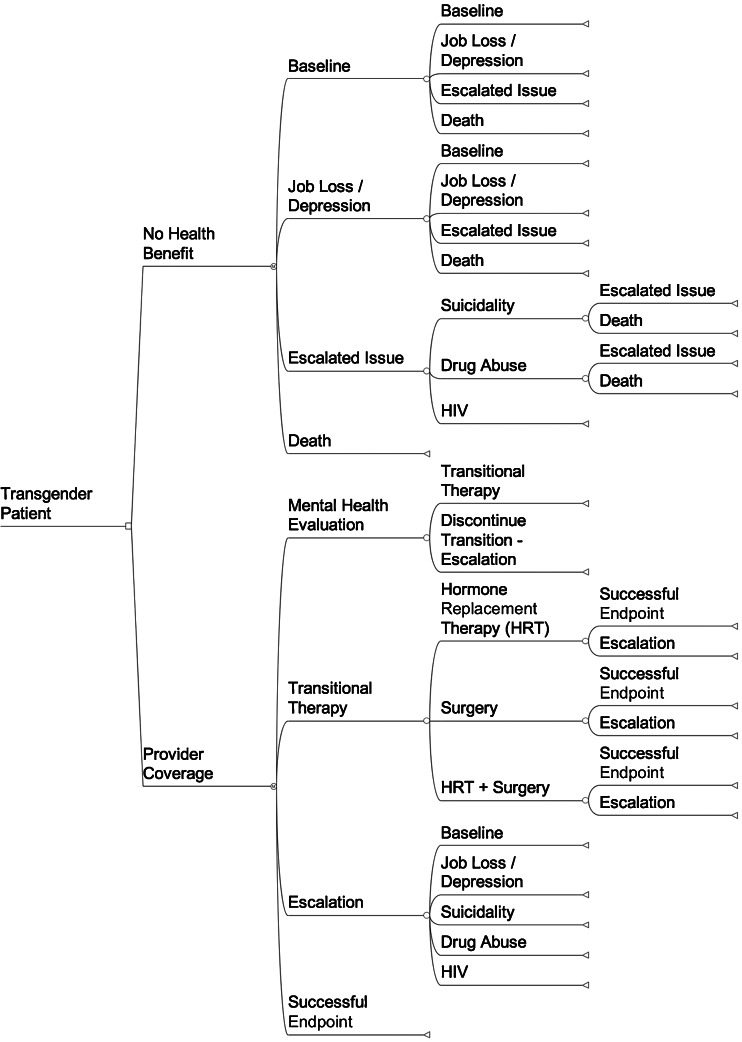
The Markov model (Fig. 1) was built using TreeAge (TreeAge Software, Inc., Williamstown, MA, USA; 2009). With provider coverage, 100 % of patients were modeled to have authorized transitional therapy care in accordance with the World Professional Association for Transgender Health (WPATH) standards of care.3
Figure 1.
A simplified Markov diagram comparing no health benefit to provider coverage of medically necessary services for the U.S. transgender population.
Patients could experience a continuous progression of outcomes in escalating stages over 1-year cycles for up to 10 years. Patients in escalated states required costly rehabilitation to cycle through job loss/depression in order to return to a preferable baseline state. Patients who cycled into escalated states had increased risk of drug abuse, suicidality, and HIV.21 The risk of death included all-cause mortality22 and specific mortality rates from suicide and drug overdose.23 – 25 Following transitional therapy, the model included costs for provider coverage to reduce negative outcomes.
No Health Benefit
The structure of the no health benefit arm accounted for denial of coverage to transgender patients for medically necessary and preventive care, as well as adverse implications. Patients began either at baseline or a job loss/depression state according to the unemployment rate associated with anti-transgender bias.1 Patients at baseline and in the job loss/depression state were modeled as having high rates of escalating issues, including death.1 Alternatively, patients at baseline accrued no cost.
Provider Coverage
Patients with health insurance with provider coverage could navigate through transitional therapy or denial. Patients denied coverage following a mental health evaluation transitioned to baseline or escalated states. This sub-tree accounted for variations in policy and practice, including barriers raised through insurance claims and coding processes. For example, if a female-to-male (FTM) patient changed his legal gender marker and then submitted billing for a Pap smear, coverage was modeled as denied based on his gender marker despite the provider’s adherence to WPATH guidelines.
Provider coverage was modeled as having higher costs and improved quality of life. The model also incorporated probabilities for negative health outcomes. Most patients were assumed to receive a full range of services indicated by WPATH, including reconstructive procedures.3 , 7
Assumptions
The model included several assumptions. First, provider coverage paid for the following procedural combinations: surgery, HRT, surgery and HRT, discontinued transition, and costs associated with baseline prevalence of job loss/depression. Second, costs for provider coverage were equivalent to reimbursed rates for procedural diagnosis-related groups (DRGs). Third, transitional therapy would maintain its baseline utility.
Data Collection
Data were collected from a systematic review of over 30 randomized controlled trials, observational data, and case series detailing types of gender-confirming care, whether transphobic-related events triggered negative outcomes, and the existence of a defined outcome for each related state. Many probabilities were from the NTDS (Table 1).1
Table 1.
Probabilities for the cost-effectiveness analysis
| Probabilities | Base Case | Range for Sensitivity Analyses | Source |
|---|---|---|---|
| No Health Benefits | |||
| Baseline | 0.74 | 0.629–0.851 | 1 |
| Baseline | 0.7 | 0.595–0.805 | 1 |
| Job Loss/Depression* | 0.199 | 0.169–0.229 | 1 |
| Escalation | 0.1 | 0.085–0.115 | 1 |
| Suicidality* | 0.82 | 0.697–0.943 | 1 |
| HIV | 0.048 | 0.039–0.053 | 1 |
| Drug Abuse | 0.13 | 0.1105–0.1495 | 1 |
| Death | 0.00012 | 0.000102–0.000138 | 22 |
| Active | 0.26 | 0.221–0.299 | 1 |
| Baseline | 0.58 | 0.493–0.667 | 1 |
| Active | 0.26 | 0.221–0.299 | 1 |
| Escalation | 0.13 | 0.1105–0.1495 | 1 |
| Suicidality* | 0.739 | 0.628–0.849 | 1 |
| HIV | 0.101 | 0.086105–0.116495 | 1 |
| Drug Abuse | 0.16 | 0.136–0.184 | 1 |
| Death* | 0.00012 | 0.000102–0.000138 | 22 |
| Death | 0.00012 | 0.000102–0.000138 | 22 |
| Suicidality | |||
| Job Loss/Depression* | 0.47 | 0.399–0.541 | 1 |
| Suicidality | 0.33 | 0.281–0.380 | 24 |
| Drug Abuse | 0.08 | 0.068–0.092 | 1 |
| Death | 0.12 | 0.102–0.138 | 24 |
| Drug Abuse | |||
| Job Loss/Depression* | 0.383 | 0.326–0.441 | 1 |
| Drug Abuse | 0.448 | 0.381–0.515 | 1 |
| HIV | 0.026 | 0.022–0.030 | 1 |
| Suicidality | 0.14 | 0.119–0.161 | 23–25 |
| Death | 0.0017 | 0.0014–0.0019 | 23–25 |
| Provider Coverage | |||
| Mental Health Evaluation | |||
| Denied Coverage | 0.07 | 0.059–0.081 | 1 |
| HRT | 0.62 | 0.527–0.713 | 1 |
| Escalation | 0.66 | 0.412–0.841 | 1 |
| Surgery* | 0.31 | 0.264–0.357 | 1 |
| Escalation | 0.0895 | 0.076–0.103 | 23 |
| MTF | 0.5 | Assumed | |
| w/HRT | 0.8 | 0.68–0.92 | 1 |
| w/no HRT* | 0.2 | 0.17–0.23 | 1 |
| FTM | 0.5 | Assumed | |
| w/HRT | 0.69 | 0.586–0.793 | 1 |
| w/no HRT* | 0.03 | 0.025–0.034 | 1 |
* Represents a remainder so that all probabilities add up to 1.0; FTM female-to-male transition, HRT hormone replacement therapy, MTF male-to-female transition
Costs
Transition costs were gathered from the GIC public record and the literature (Table 2).11 Existing DRGs weighted by procedural prevalence were used for initial and incremental costs of services. Thus, costs were reflective of the most common procedures (e.g. mastectomy) compared to rare procedures (e.g. phalloplasty).11 , 17 There were no costs attributed to baseline state or death. Depression, suicidality, and drug abuse states resulted in rehabilitative costs.26 – 28 The U.S. cost of illness for HIV was extracted from Walensky et al.29
Table 2.
Costs for the cost-effectiveness analysis
| State | Cost Type | ICD-9 Code | Base Case Costs ($) | Range for Sensitivity Analyses | Source |
|---|---|---|---|---|---|
| Baseline | n/a | n/a | Anchor | ||
| Job Loss – Depression | Annual | 311 | 565.06 | 63.00–3781.10 | 28 |
| Attempted Suicide | Annual | 296 | 21,671.00 | 18420.35–24921.65 | 27 |
| HIV (generic therapy) | Annual | 042 | 11,600.00 | 9860.00–13340.00 | 29 |
| Drug & Substance Abuse | Annual | 304 | 11,448.00 | 9730.80–13165.20 | 26 |
| Cost for Mental Health Evaluation | Fixed | n/a | 2175.00 | 1848.75–2501.25 | 19 |
| HRT | Fixed | n/a | 4350.00 | 3697.50–5002.50 | 19 |
| Surgery | |||||
| MTF w/HRT | Fixed | n/a | 22,025.00 | 18721.25–25328.75 | 19 |
| MTF w/o HRT | Fixed | n/a | 17,675.00 | 15023.75–20326.25 | 19 |
| FTM w/HRT | Fixed | n/a | 14,658.00 | 12459.30–16856.70 | 19 |
| FTM w/o HRT | Fixed | n/a | 10,308.00 | 8761.80–11854.20 | 19 |
| Cost for Continuous Coverage | Annual | n/a | 2175.00 | 1848.75–2501.25 | 19 |
| Death | n/a | n/a | Anchor |
FTM female-to-male transition, HRT hormone replacement therapy, MTF male-to-female transition
Cost of provider coverage was dependent on combinations of surgery and HRT. HRT was a fixed cost. The MTF group represented combinations of penectomy, breast augmentation, labiaplasty, and vaginoplasty. The FTM represented combinations of mastectomy, hysterectomy, abdominoplasty, and genital augmentation. Under provider coverage, there was an annual cost of $2175 associated with medically necessary services and preventive care.
Other treatment costs were based on DRGs. Escalated states following baseline were based on employment status. The NTDS found that 78 % of respondents who successfully transitioned reported improved job performance.1 Conversely, respondents who experienced job loss were 70 % more likely to abuse substances than employed respondents. HIV rates among the transgender population were 400 % higher than in the general population, and doubled with unemployment.
Utilities
QALYs were extracted from U.S.-based sources (Table 3). Baseline utility was taken as the U.S. average according to Sullivan et al.20 This index also provided utilities for depression (ICD-9 311) and suicidality (assumed as ICD-9 296). Utility for HIV was referenced from Wu et al., and Coffin et al. provided utility data for drug abuse.30 , 31 Surgery had a disutility.32 Benefit coverage for transition and successful endpoints were weighted as 0.867 QALYs, given primary preferences for these outcomes aligned with the U.S. population average.30 , 31
Table 3.
Utilities for the cost-effectiveness analysis
| Utilities | ICD-9 Code | Base Case Utility | Range for Sensitivity Analyses | Source |
|---|---|---|---|---|
| Baseline* | n/a | 0.867 | 0.737–0.997 | 20 |
| Job Loss – Depression | 311 | 0.732 | 0.622–0.842 | 20 |
| Attempted Suicide | 296 | 0.693 | 0.589–0.797 | 20 |
| HIV | 042 | 0.800 | 0.680–0.920 | 31 |
| Drug & Substance Abuse | 304 | 0.800 | 0.730–0.900 | 30 |
| Hormone Replacement Therapy (HRT) | n/a | 0.867 | 0.737–0.997 | Assumed |
| Surgery (transition utility from baseline) | n/a | −0.155 | −0.178 to −0.132 | 32 |
| End-State | n/a | 0.867 | 0.737–0.997 | Assumed |
| Death | n/a | 0.0 | 0.0–0.0 | Anchor |
*The benefit of having transitional therapy is no disutility from baseline status
Sensitivity Analyses
Univariate and multivariate sensitivity analyses were used to test model uncertainty. These sensitivity analyses were performed by varying all base case estimates by reported distributions (e.g., confidence intervals, standard deviations) or by varying estimates ±15 % of the mean when distributions were not reported.
In one particular univariate analysis, the probability of patients starting in job loss/depression ranged from 0–29.9 % in the provider coverage arm, since the model assumed some baseline prevalence of depression or unemployment not negated by transition therapy, leading to downstream escalations.
A Bayesian multivariate probabilistic sensitivity analysis applied distributions for each variable to characterize uncertainty on all parameters simultaneously using 10,000 Monte Carlo simulations. Beta distributions were used for probabilities and utilities (i.e., values of 0.0–1.0), and gamma distributions were used for costs (i.e., positive values).
Budget Impact Analysis
The budget impact of transgender coverage was measured relative to the total U.S. population, thereby gauging equity of absorbing costs of coverage in a small population.33 Budget impact was calculated on a per-member-per-month basis for an approximate 2014 U.S. population of 320 million (U.S. Census Bureau, 2014). The calculation assumed that following implementation of blanket provider coverage, there would be an influx of about 30,000 transgender persons seeking transitional care in the first 5 years (i.e., 6000/year taken as the midpoint of 3000–9000 procedures per year according to Walsham).32 The additional cost would be the difference in cost of benefit coverage from the model.
RESULTS
Expected Cost and Effectiveness
Provider coverage resulted in higher cost and greater effectiveness, and was cost-effective relative to no health benefits at 5 and 10 years from a willingness-to-pay (WTP) threshold of $100,000/QALY (Table 4). These results were driven by the cohort without health benefits, which had less favorable outcomes, including depression, HIV, and death. The 5-year incremental cost effectiveness ratio (ICER) was greater than that at 10 years, since upfront costs for transitional therapy were not yet offset by costly long-term endpoints of excluded coverage (e.g., HIV, drug abuse).
Table 4.
Expected results of the base case cost-effectiveness analysis
| Cost (USD 2013) | Δ Cost | Health Utility (QALYs) | Δ Utility | ICER ($/QALY) | |
|---|---|---|---|---|---|
| 5-Year Time Horizon | |||||
| No Health Benefit | 10,712.00 | 3.71 | |||
| Provider Coverage | 21,326.00 | 10,614.00 | 3.98 | 0.27 | 39,311.11 |
| Male-to-Female (MTF)* | 22,545.00 | 11,833.00 | 3.98 | 0.27 | 43,825.93 |
| Female-to-Male (FTM)* | 20,107.00 | 9395.00 | 3.98 | 0.27 | 34,796.30 |
| 10-Year Time Horizon | |||||
| No Health Benefit | 23,619.00 | 6.49 | |||
| Provider Coverage | 31,816.00 | 8197.00 | 7.37 | 0.88 | 9314.77 |
| Male-to-Female (MTF)* | 33,034.00 | 9415.00 | 7.37 | 0.88 | 10,698.86 |
| Female-to-Male (FTM)* | 30,597.00 | 6978.00 | 7.37 | 0.88 | 7929.55 |
(*) Compared to no health benefit; QALY quality-adjusted life year
The 5-year budget impact analysis determined a cost of $0.016 per member per month, meaning that if U.S. society assumed the role of paying an additional $10,614 for each person seeking benefit coverage, the U.S. population could absorb these costs for just cents per month.
Sensitivity and Threshold Analyses
Variations in expected values of all cost, probability, and utility estimates did not change expected results. Univariate sensitivity analyses indicated that the model was most sensitive to (1) probability of suicidal death, (2) probability of drug abuse, and (3) utilities of baseline, depression, and drug abuse. However, univariate and two- and three-way sensitivity analyses did not alter results.
The results did not change in sensitivity analysis of patients with provider coverage starting at a baseline with job loss or depression. The maximum probability of 29.9 % job loss/depression produced a 10-year ICER of only $20,942/QALY.
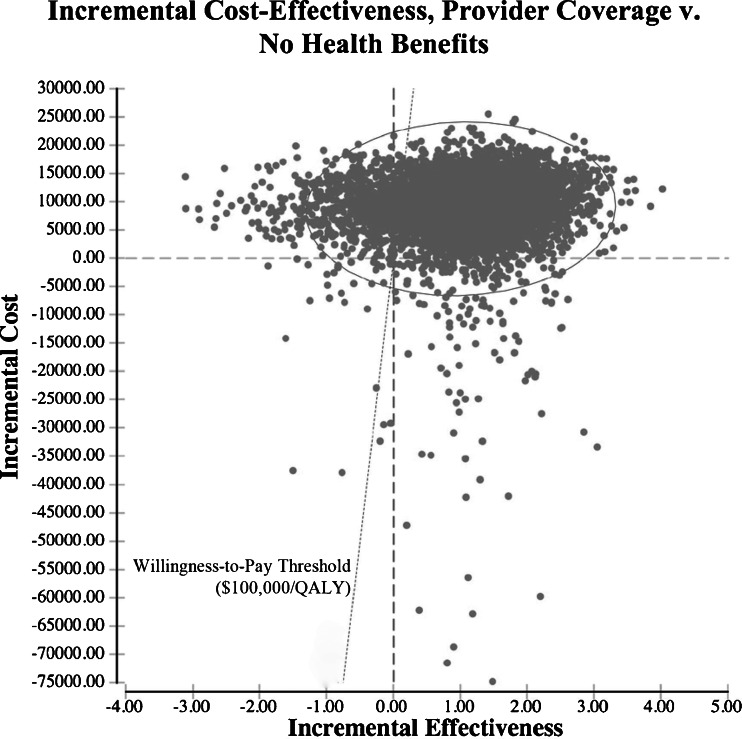
The probabilistic sensitivity analysis showed that provider coverage was cost-effective compared to no health benefit in 8477 of 10,000 Monte Carlo simulations at a mean ICER of $8655/QALY (median ICER of $8593/QALY). In 389 of these simulations, provider coverage dominated the alternative (Fig. 2).
Figure 2.
A scatter plot of a Bayesian multivariate probabilistic sensitivity analysis measuring the incremental cost-effectiveness ratios (ICERs) of 10,000 Monte Carlo simulations. Under no health benefit, people who are transgender navigate issues such as employment discrimination and depression, which can escalate to more severe health states such as suicidality, drug abuse, and HIV, according to the 2011 National Transgender Discrimination Survey. A lack of provider coverage under this arm increases the risk of these issues. In the other arm, provider coverage improves access to primary and preventive care, as well as medically necessary services that in most cases lead to transitional therapy such as hormone replacement therapy and surgery. The majority of people with provider coverage achieve preferred health states with greater utility, at an increased cost per year of about $2175. The risks of escalated issues such as depression and suicidality still exist for the provider coverage arm, since not all people qualify for all benefits, and transitional therapy does not completely insulate against these issues.
DISCUSSION
These findings suggest that the removal of transgender exclusions is affordable and efficient with respect to the U.S. population. Provider coverage is a cost-effective policy at a willingness-to-pay threshold of $100,000/QALY. The ICER of provider coverage for medically necessary services and preventive care at 10 years is about $9300/QALY, which suggests that this policy would be comparatively efficient on a per-patient basis. Even at 5 years, this type of program still holds good value. These findings appear robust to model uncertainty according to sensitivity analyses. In addition, the results of the budget impact analysis imply that this policy is affordable, with a cost of only about $0.016 per member per month.
This case presents an economical coverage policy that can be likened to patients in the U.S. facing similar challenges of access to necessary care, such as those with rare diseases who have access to necessary health technology as a result of the Orphan Drug Act of 1983.34 For instance, cystic fibrosis (CF) affects a population of only 30,000 individuals in the U.S., but has evolved into a successfully treatable chronic disease with the availability of new pharmaceuticals.35 While the cost of ivacaftor for CF ($300,000/year) is neither affordable nor efficient (ICER > $ 1million/QALY), this act makes it available to CF patients.36 By the absorption of the cost of ivacaftor across the U.S. population for people who are uninsured or have annual incomes less than $150,000, the budget impact is only about $0.05 per member per month.37
While justice, legality, and a desire to avoid discrimination should drive decisions about benefit coverage, this case for the transgender population also appears economically attractive. The budget impact analysis calculates the expected value of costs for a state with an average population of 700 instances of transition therapy each year. Thus, if state governments require that payers offer coverage, insurance companies need to account for approximately $7.5 million per state. While cost-effective on a societal level, there is some upfront investment required of payers. A return-on-investment (ROI) calculation for this figure shows that it would take a payer approximately 63 years to break even on an investment in this type of benefit program.
However, legal and administrative barriers can hinder the implementation of new policy informed by these results. First, commercial payers are accustomed to negotiating contracts and benefit packages in ways that may resist change. It may be difficult to instantaneously adopt changes in provider coverage when exclusions are enforced by a third party or if state law defines health services to exclude transgender benefits.38 Fortunately, transgender exclusions were recently removed by states, commercial payers, and CMS.4 , 7
According to the Human Rights Commission, 57 of the approximately 200 major employers offering at least one transgender-inclusive health care coverage plan were law firms, possibly reflecting the growing legal consensus that transgender exclusions are discriminatory in practice.7 , 39 At least 17 major insurance carriers administer or provide coverage for at least one employer or student plan offering transgender benefits (e.g., Aetna, Cigna, Harvard Pilgrim, United Healthcare, and Blue Cross Blue Shield Massachusetts).40 Additionally, numerous public employers offer provider coverage (e.g., University of California, University of Michigan, City of Minneapolis, City of New York, and City of San Francisco).15 , 40 However, most U.S. health insurance policies still contain transgender exclusions, even though treatment of gender identity disorder is neither cosmetic nor experimental.40 , 41
This study has several limitations. First, data were lacking on whether transition-related therapy completely prevents negative endpoints such as depression/suicidality, or whether a baseline prevalence still exists. Second, some data in this analysis were representative not of the transgender population, but of the general population. Third, no empirical evidence exists on the time-dependency of escalated issues, so expert opinion guided transition probabilities. Fourth, no true health utilities were available for outcomes triggered by anti-transgender bias.11 Fifth, some costs were derived from an ad hoc survey of provider affiliates to the GIC. Although these results should be widely applicable to most institutions, some insurance carriers have third-party payers or self-payers that could change the relevance of these results. Sixth, while depression and job loss are grouped together in the model, there may be some element of exclusivity in these two states that cannot be well-discerned by health utility. Seventh, HIV and drug abuse represent two of many possible negative outcomes; the choice to highlight these in the model was based on reported prevalence in the NTDS.
Finally, this study did not include children or adolescents, and focused on an adult-only population, based on the age of respondents in the NTDS. According to de Vries et al., young adults experience alleviation of gender dysphoria and improvement in psychological functioning following gender reassignment.42 Given this promise, the field could benefit from additional outcomes research among youth.
Another challenge of this study involves the premise that outcomes research is able to justify transgender benefit coverage. QALYs in this study come from societal preferences for chronic conditions. People are not asked to consider a state of being for a transgender person who is depressed or HIV-positive, for example, nor are transgender individuals represented. According to Lyons et al., there is a stigma attached to the inclusion of transgender-stratified preferences and outcomes in trials and observation,43 which speaks to the broader issue of gaining consensus within U.S. society in accepting that unique services covered by transgender benefits are as necessary as care for people not seeking a transition.
By removing transgender exclusions, society could change the trajectory of health for all transgender persons. It is worth considering that other costly surgeries (e.g., breast reduction;, spinal fusion for chronic back pain), procedures (e.g., in vitro fertilization), and health technologies (e.g., drugs such as sildenafil citrate for erectile dysfunction) that consensus dictates as not medically necessary are still covered by payers. Overall, payers may provide the motivation for progress in a field when there is the potential of reimbursement for improved performance. This concept could be likened to poor outcomes of phalloplasty in MTF transitions: surgeons might invest in trials that improve outcomes of these complicated procedures if they knew they would be reimbursed.44 A law protecting transgender benefit coverage is not only medically necessary, but is morally imperative.
Ultimately, removing a clause expressly prohibiting coverage for medically necessary care in the transgender population is economical at a U.S. societal level. State laws that define “health services,” thereby dictating benefit exclusions, should be amended to reflect contemporary medical evidence.4 , 38 , 45 Affiliated contracting agencies and bodies should remove their corresponding exclusions given that provider coverage is affordable, efficient, and equitable.
ACKNOWLEDGMENTS
The authors wish to thank Dolores Mitchell at the Commonwealth of Massachusetts Group Insurance Commission.
William Padula’s time for this study was supported in part by an AHRQ F32 National Research Service Award (1 F32 HS023710-01) as well as an unrestricted University of Chicago Medicine Small Grant in Diversity Research. Shiona Heru was supported by a merit fellowship from Western New England University School of Law in affiliation with the Gender and Sexuality Center.
This study was presented as a poster at the Annual Meeting of the Society of Medical Decision Making in Miami, Florida, in October 2014.
Compliance with Ethical Standards
Conflict of Interest
The Authors have no conflicts of interest to declare. Authorship of this manuscript follows ICMJE guidelines; each author is associated with conceptualization, writing, final approval, and accountability for the work.
REFERENCES
- 1.Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at Every Turn: a Report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011. [Google Scholar]
- 2.Gorton RN. Transgender Medicine. San Francisco: Lyon-Martin Health Services; 2010. [Google Scholar]
- 3.Coleman E, Bockting W, Bozter M, Cohen-Kettenis P, DeCurpere G, Feldman J, et al. Standards of care for health of transsexual, transgender, and gender nonconforming people. Int J Transgenderism. 2011;13(4):165–232. doi: 10.1080/15532739.2011.700873. [DOI] [Google Scholar]
- 4.Departmental Appeals Board Appellate Division. Transsexual Surgery. Washington, D.C.2014. Report No.: Docket No. A-13-87, Decision No. 2576.
- 5.Notice of Proposed Regulations: MassHealth. The Commonwealth of Massachusetts. Executive Office of Health and Human Services. Public Notice, 130 CMR 405.000, 130 CMR 406.000, 130 CMR 410.00-AOH, 130 CMR 410.000-COH, 130 CMR 415.000, 130 CMR 423.000, 130 CMR 424.000, 130 CMR 433.000 (October 8, 2014); Public Notice, 130 CMR 450.000 (September 12, 2014).
- 6.Daniel H, Butkus R. Lesbian, gay, bisexual, and transgender health disparities: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015 doi: 10.7326/M14-2482. [DOI] [PubMed] [Google Scholar]
- 7.Friedman K, Robinson A, Fidas D, Cooper L, Leibowitz E. In: Transgender-Inclusive Healthcare Coverage and the Corporate Equality Index. Fidas DGJ, Wilson A, editors. Washington, D.C: Human Rights Campaign Foundation; 2013. [Google Scholar]
- 8.Walsham K. De-gendering health insurance: a case for a federal insurance nondiscrimination act. 24 Hastings Women's Law J. 2013 Winter;197:12.
- 9.Macy v. Department of Justice, U.S. Equal Employment Opportunity Commission, Appeal No. 0120120821, (2012 Apr 20).
- 10.Primary Care Protocol for Transgender Patient Care. San Francisco: Center of Excellence for Transgender Health, University of California, Department of Family and Community Medicine; 2011 Apr.
- 11.Horton M. Cost of Transgender Health Benefits. Out and Equal Workplace Summit. 2008 Sep; Retrieved from: http://www.tgender.net/taw/thbcost.html. Accessed on 17 Sept 2015.
- 12.Herman JL. The Cost of Employment Discrimination against Transgender Residents of Massachusetts. The Williams Institute, UCLA School of Law. 2011.
- 13.Lundström B. Gender Dysphoria: a Social-Psychiatric Follow-Up Study of 31 Cases not Accepted for Sex Reassignment. Gothenburg, Sweden: University of Gothenburg; 1981. [Google Scholar]
- 14.Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav. 1988;17(5):439–457. doi: 10.1007/BF01542484. [DOI] [PubMed] [Google Scholar]
- 15.Lundstrom B, Pauly I, Walinder J. Outcome of sex reassignment surgery. Acta Psychiatr Scand. 1984;70(4):289–294. doi: 10.1111/j.1600-0447.1984.tb01211.x. [DOI] [PubMed] [Google Scholar]
- 16.Lipscomb J, Weinstein MC, Torrance GW. Time preference. In: Gold M, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. pp. 214–235. [Google Scholar]
- 17.Beck JR, Pauker SG. The Markov process in medical prognosis. Med Decis Mak. 1983;3:419–458. doi: 10.1177/0272989X8300300403. [DOI] [PubMed] [Google Scholar]
- 18.Luce B, Manning WG, Siegel JE, Lipscomb J. Estimating costs in cost-effectiveness analysis. In: Gold M, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. pp. 176–213. [Google Scholar]
- 19.Healthcare Bluebook. Brentwood, TN: CAREOperative; 2015.
- 20.Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Mak. 2006;26:410–420. doi: 10.1177/0272989X06290495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorton RN, Buth J, Spade D. Medical Therapy and Health Maintenance for Transgender Men: A Guide for Health Care Profiders. San Francisco: Lyon-Martin Health Services; 2005. [Google Scholar]
- 22.Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: Final data for 2005. National Vital Statistics Reports; vol 56 no 10. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- 23.Cochran SD, Mays VM. Mortality risks among persons reporting same-sex sexual partners: evidence from the 2008 General Social Survey-National Death Index data set. Am J Public Health. 2015;105(2):358–364. doi: 10.2105/AJPH.2014.301974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dhejne C, Lichtenstein P, Boman M, Johansson AL, Langstrom N, Landen M. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One. 2011;6(2) doi: 10.1371/journal.pone.0016885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lombardi E. Enhancing transgender health care. Am J Public Health. 2001;91(6):869–872. doi: 10.2105/AJPH.91.6.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bishai D, Sindelar J, Ricketts EP, Huettner S, Cornelius L, Lloyd JJ, et al. Willingness to pay for drug rehabilitation: implications for cost recovery. J Health Econ. 2008;27(4):959–972. doi: 10.1016/j.jhealeco.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Czernin S, Vogel M, Fluckiger M, Muheim F, Bourgnon JC, Reichelt M, et al. Cost of attempted suicide: a retrospective study of extent and associated factors. Swiss Med Wkly. 2012;142:w13648. doi: 10.4414/smw.2012.13648. [DOI] [PubMed] [Google Scholar]
- 28.Padula WV, Allen RR, Nair KV. Determining the cost of obesity and its common comorbidities from a commercial claims database. Clin Obes. 2014;4(1):53–58. doi: 10.1111/cob.12041. [DOI] [PubMed] [Google Scholar]
- 29.Walensky RP, Sax PE, Nakamura YM, Weinstein MC, Pei PP, Freedberg KA, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158(2):84–92. doi: 10.7326/0003-4819-158-2-201301150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Ann Intern Med. 2013;158(1):1–9. doi: 10.7326/0003-4819-158-1-201301010-00003. [DOI] [PubMed] [Google Scholar]
- 31.Wu AW, Jacobson KL, Frick KD, Clark R, Revicki DA, Freedberg KA, et al. Validity and responsiveness of the Euroqol as a measure of health-related quality of life in people enrolled in an AIDS clinical trial. Qual Life Res. 2002;11(3):273–282. doi: 10.1023/A:1015240103565. [DOI] [PubMed] [Google Scholar]
- 32.Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care. 2011;49(4):385–392. doi: 10.1097/MLR.0b013e31820292b3. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value Health. 2014;17(1):5–14. doi: 10.1016/j.jval.2013.08.2291. [DOI] [PubMed] [Google Scholar]
- 34.Reaves ND. A model of effective health policy: the 1983 Orphan Drug Act. J Health Soc Policy. 2003;17(4):61–71. doi: 10.1300/J045v17n04_04. [DOI] [PubMed] [Google Scholar]
- 35.Strausbaugh SD, Davis PB. Cystic fibrosis: a review of epidemiology and pathobiology. Clin Chest Med. 2007;28(2):279–288. doi: 10.1016/j.ccm.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 36.Whiting P, Al M, Burgers L, Westwood M, Ryder S, Hoogendoorn M, et al. Ivacaftor for the treatment of patients with cystic fibrosis and the G551D mutation: a systematic review and cost-effectiveness analysis. Health Technol Assess (Winchester, England) 2014;18(18):1–106. doi: 10.3310/hta18180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schultz NM, Malone DC. PSY14 - a probabilistic budget impact analysis of cystic fibrosis therapy on health plan pharmacy budgets. Value Health. 2014;17(3):A226. doi: 10.1016/j.jval.2014.03.1319. [DOI] [Google Scholar]
- 38.Massachusetts General Law 118E §64. 2012.
- 39.Rosenbaum S. Insurance discrimination on the basis of health status: an overview of discrimination practices. Law J Med Ethics. 2009;37:103–109. doi: 10.1111/j.1748-720X.2009.00423.x. [DOI] [PubMed] [Google Scholar]
- 40.Coleman SC, et al. Hidden Costs, Value Lost: Uninsurance in America. Washington, DC: Institute of Medicine; 2003. [Google Scholar]
- 41.Meyer W, III, Bockting WO, Cohen-Kettenis P, Coleman E, Diceglie D, Devor H, et al. The Harry Benjamin international gender dysphoria association's standards of care for gender identity disorders, sixth version. J Psychol Hum Sex. 2002;13(1):1–30. doi: 10.1300/J056v13n01_01. [DOI] [Google Scholar]
- 42.de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704. doi: 10.1542/peds.2013-2958. [DOI] [PubMed] [Google Scholar]
- 43.Lyons T, Shannon K, Pierre L, Small W, Krusi A, Kerr T. A qualitative study of transgender individuals' experiences in residential addiction treatment settings: stigma and inclusivity. Subst Abuse Treat Prev Policy. 2015;10:17. doi: 10.1186/s13011-015-0015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nexon D, Ubl SJ. Implicaitons of health reform for the medical technology industry. Health Aff (Millwood) 2010;29(7):1325–1329. doi: 10.1377/hlthaff.2010.0436. [DOI] [PubMed] [Google Scholar]
- 45.Mass. Legis. Serv. Ch. 151 (H.B. 6100) (Ch. 118G §1). 1996.