Abstract
Objective: To evaluate if addition of educational cartoon to pediatric bowel preparation instructions improves the quality of bowel preparation and patient experience. Methods: Patients were randomized to control group receiving standard bowel preparation instructions or intervention group receiving additional educational cartoon. To objectively rate bowel preparation, a blinded endoscopist completed numeric Ottawa score (0-14, with 0 being best). The family also completed a questionnaire rating the bowel preparation process. Results: Data from 23 patients were analyzed. Mean Ottawa score in the intervention group compared with controls was not significantly different (mean scores 3.73 and 3.33, respectively; P = .384). Level of education was significantly correlated with better Ottawa score in the overall population (ρ = −.462, P = .026) and within the control group (ρ = −.658, P = .02). Both groups of patients reported positive experience with bowel preparation. Conclusion: There may be benefit to further investigation of this educational cartoon in parents with less than college level education or non-English-speaking families in larger population of patients.
Keywords: patient education, bowel preparation, colonoscopy, pediatrics
Introduction
Colonoscopy is a routine diagnostic procedure performed on children to assess for a variety of gastroenterological conditions. Effective bowel preparation to clean the colon prior to the study is essential. Numerous studies have looked at safety and efficacy of different bowel preparation protocols. There is no standard bowel preparation regimen, but it is agreed that success of the procedure depends highly on the quality of the bowel preparation. Residual fluid or stool in the colon impedes the endoscopist’s ability to view the mucosal lining, visually assess for pathologic lesions or abnormalities, and in some cases complete the procedure.1
Potential barriers to successfully completing the bowel preparation regimen have been previously identified as ease of administration, palatability of the preparation, the volume of preparation that must be consumed, restrictions of activities to complete the preparation, and adverse effects of nausea, vomiting, bloating, and/or abdominal pain.1,2 Additionally, we suspect that incomplete understanding regarding the importance of the completeness of bowel preparation might also contribute to decreased compliance. Abbott reported that noncompliant patient behavior may be attributable to confusion, disappointment, misunderstanding, and fear and that compliance increases when the patient understands the rationale for the procedure, the preparation for the procedure, and the potential complications.3
St Christopher’s Hospital for Children, located in North Philadelphia, serves a diverse pediatric patient population, with a significant proportion of socioeconomically disadvantaged individuals who may have limited health literacy. Feedback from endoscopists and nursing staff indicated that, in general, bowel preparation quality was not ideal and compromised the ability to visualize mucosal lining. Parents also stated they had difficulties following the bowel preparation regimen as prescribed.
Based on these observations, we hypothesized that implementation of an instructional cartoon directed at pediatric patients and their parents highlighting the importance of an adequate bowel preparation prior to colonoscopy would improve the quality of the bowel preparation and parent/patient experience with the preparation process.
Methods
The study was a prospective randomized single blinded pilot investigation to evaluate the efficacy of an informational cartoon developed by our group that highlights key points and importance of bowel preparation prior to colonoscopy. This study was conducted in the outpatient clinic setting in the Section of Gastroenterology, Hepatology, and Nutrition at St Christopher’s Hospital for Children in Philadelphia, PA, from October 2011 to June 2013.
Participants: Inclusion/Exclusion Criteria
The inclusion criteria were as follows: children ages 7 to 14 years, followed at the St Christopher’s Hospital for Children Gastroenterology clinic (main campus), undergoing elective, outpatient, first time colonoscopy for any indication (including diarrhea, abdominal pain, failure to thrive). Exclusion criteria were as follows: non-English speaking, admitted to the inpatient service, seen at the satellite clinic, and previous history of undergoing a colonoscopy.
As this was a pilot study, our target sample size was 15 patients in each group. We anticipated that with groups of this size, we would be able to establish trends in the data that would suggest benefit to a larger study. We enrolled 27 total subjects and acquired data on 23.
Study Design
Patients were considered for the study if a decision was made at their clinic appointment to schedule a colonoscopy for any indication and the inclusion criteria were met. After consent and assent were obtained, patients were randomized to 1 of 2 groups. The control group received the standard verbal and written bowel preparation instructions by the office nurse at their clinic appointment prior to colonoscopy. The clinic uses a bowel preparation regimen that includes a low residue diet, PEG-3350 (238 g in 1.5 L sports drink 1 day prior to procedure), and bisacodyl (10 mg daily for 2 days prior to procedure). The intervention group received the standard bowel preparation instructions plus the 1-page informational cartoon. Our research coordinator reviewed the cartoon with the family at the office visit, and the families then took the cartoon home with them. Patients in both groups were instructed to contact the office if they had questions about the bowel preparation. On the day of the procedure, the parent filled out a questionnaire to collect demographic information and answer questions about the bowel preparation experience. The endoscopist assigned an Ottawa scale score to quantify the quality of the bowel preparation.
Intervention
Our group developed the content of the 1-page color cartoon, and independent artists were consulted to create the artwork. The cartoon (Figure 1) depicts a child experiencing the progression of scheduling, preparing for, and undergoing a colonoscopy. This includes the appointment at his gastroenterologist’s office when the procedure is explained, the diet he must follow prior to the procedure, the consumption of the bowel preparation, and the events on the day of the procedure. The message of the cartoon highlights that a successful colonoscopy depends on following the diet and bowel preparation regimen prescribed by the doctor before the procedure.
Figure 1.
Bowel preparation cartoon. The cartoon underscores the importance of diet and the bowel preparation regimen prior to successful colonoscopy.
Rating Scale
We adapted the Ottawa rating scale,4 which has been validated in adult studies to assess the quality of bowel preparation.1 This scale assesses fluid cleanliness and fluid volume separately. Cleanliness is assessed for the right colon, the mid colon, and the rectosigmoid individually, and the fluid value is a global value for the entire colon. The score has a range from 0 (perfect) to 14 (solid stool in each colon segment and lots of fluid).
Parent Questionnaire
On the day of the procedure, the parent completed a questionnaire. Demographic information was collected, including patient’s date of birth, gender, race and ethnic group, and highest level of education completed by the parent. The parents were asked if they understood why it was important to complete the bowel preparation, if they understood the directions for completing the preparation, how much of the preparation their child was able to complete, and how satisfied they were with the experience of preparing for the colonoscopy.
Randomization and Blinding
Each patient was randomly assigned to either the control or intervention group by a computer-generated randomization program. The endoscopist, office nurse, and endoscopy staff were blinded to the group assignment. The authors developed the cartoon. It was drawn and created by an independent group of artists who had no role in the study design, collection, or interpretation of data.
Outcome Measure
The primary outcome measure was the total Ottawa score, indicating quality of the bowel preparation. Secondary outcomes included reported understanding of and compliance with the bowel preparation and overall experience with the process of learning about and completing the bowel preparation.
Statistical Methods
Statistical analysis was performed with the SPSS 19. The Mann–Whitney U test was used to compare the means between groups for the total Ottawa score, for which data were not normally distributed. A 2-way ANOVA was used to check for interaction between education level and treatment group. Correlations were assessed with the Spearman rank correlation (ρ). The difference between groups was considered significant if the P value was ≤.05. Data from enrolled participants not undergoing colonoscopy were not included in data analysis.
Ethical Considerations
Written informed consent by the parents or legal guardian of all patients was obtained and assent obtained from the patient. The Institutional Review Board of Drexel University College of Medicine approved the study protocol.
Results
Twenty-seven patients were enrolled in our study (Figure 2). Four patients did not complete the study. Two patients needed to complete their bowel preparation as inpatients. One patient did not meet inclusion criteria due to age (17 years) and was excluded after randomization. One patient did not keep her scheduled colonoscopy appointment. Data from 23 patients were analyzed. Of the patients who completed the study, 12 patients were in the control group and 11 were in the intervention group. Table 1 depicts the demographic information of each group, which was similar between groups.
Figure 2.

Patient recruitment and randomization.
Table 1.
Demographic Dataa.
| Control Group | Intervention Group | ||
|---|---|---|---|
| Mean age (years) | 10.26 | 10.42 | 10.09 |
| Enrolled | 23 | 12 | 11 |
| Boys | 13 | 6 | 7 |
| Girls | 10 | 6 | 4 |
| African American | 7 | 4 | 3 |
| Latino/Hispanic | 10 | 4 | 6 |
| Caucasian | 6 | 4 | 2 |
Distribution of 23 enrolled subjects by age, gender, and race.
Outcome Measures
The primary outcome measure was total Ottawa score, which did not differ significantly between control and intervention groups (mean scores 3.33 and 3.73, respectively; P = .384).
Level of education of the parent was inversely correlated with Ottawa score, both in the overall study population (ρ = −.462, P = .026) and in the control group (ρ = −.658, P = .02; Figure 3). This correlation was not significant within the intervention group. Although the difference in Ottawa score between patients of parents with college level education and those with less than college education was greater in the control group than in the intervention group, a 2-way ANOVA failed to detect a significant interaction between intervention group and education level (P = .25 for the interaction); therefore, it is not possible to assert that this pattern is reliable.
Figure 3.
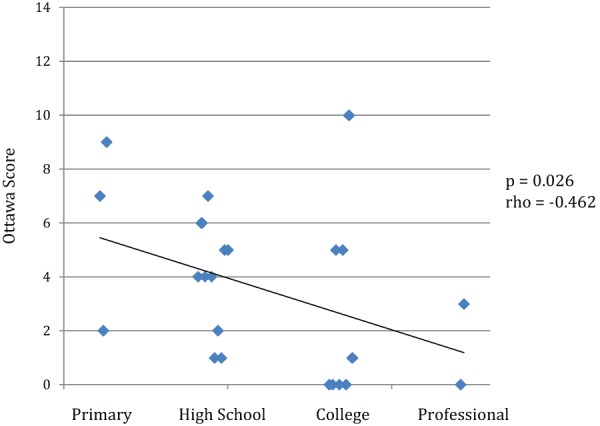
Ottawa scores by level of education.
Secondary measures were analyzed from our survey data. Hundred percent of parents responded that they understood why it was important to take the preparation. Twenty-two of 23 patients (96%) responded that they understood all the directions regarding how to complete the bowel preparation. Twenty of 23 parents (87%) responded that their child took more than 90% of the preparation, and 100% of the parents responded that their child took at least 50% of the preparation. Twenty-one of 23 patients (91%) reported that they were very satisfied with the experience of preparing for the colonoscopy. One parent reported being somewhat satisfied and one parent reported being not satisfied. Both these patients were randomized to the control group.
Discussion
A recent review article of bowel preparation regimens and their efficacy in the pediatric population by Hunter and Mamula1 described a range of success with various bowel preparation regimens. One study reported that as much as 37% of patients required repeat examination because of inadequate bowel preparation. Repeating the study is costly and poses additional safety hazards for the patient, including risks of repeating the procedure and repeated exposure to anesthesia, a significant concern particularly in the pediatric population.
A study of adult colonoscopies by Lebwohl et al5 found that suboptimal preparation was statistically more likely in Medicaid patients when compared with non-Medicaid patients. In another study, compliance with printed instructions in patients sent home from the emergency department was found to be only 36%,6 which may have been due to functional illiteracy of patients who were unable to comprehend written instructions.7 The National Institutes of Health recommends that written materials distributed to patients be geared to a fourth- to eighth-grade reading level to maximize information disseminated to patients with limited health literacy.8
McDermott9 was the first to describe the use of cartoons as visual aids for medical and health education of adults and children in 1989. Delp and Jones7 then published a study in 1996 comparing outcomes of adult patients who received printed discharge instructions with and without cartoon drawings. They demonstrated improved comprehension of and compliance with instructions in patients who received the cartoon drawings. Their findings were even more pronounced when they compared education level of the patients. In a study by Shaikh et al,10 which looked at a demographic of financially disadvantaged adult patients with low level of education, the patients who received an educational pamphlet demonstrated superior bowel preparation quality. Another adult study of inpatients by Rosenfeld et al demonstrated improved quality of bowel preparation by providing patients with a short counseling session and written materials regarding the preparation.11 In 2012, Tae et al published a study of adult patients undergoing colonoscopy in Korea and found improved quality of bowel preparation in patients who received cartoon visual aids.12
We hypothesized that adding an educational cartoon to highlight the importance of taking the bowel preparation to the standard verbal and written teaching instructions would improve the outcome of bowel preparation in children. However, these results showed that objective quality of bowel preparation was not improved when a supplemental educational cartoon was used. The study was designed with an initial premise (based on anecdotal reports) that in the patient population at St Christopher’s Hospital for Children, the overall quality of bowel preparation was only fair. This was perceived as a problem requiring further brainstorming to solve. However, in our study population, we found that the objective quality of bowel preparation to be good overall, regardless of which group the patient was assigned. Therefore, with bowel preparation that was already good, it may have been difficult to improve on it in a clinically meaningful way by adding to the teaching that is already being provided by the office nurse.
We also hypothesized that parents of patients who were randomized to the intervention group would report increased understanding about why the bowel preparation process was important, would report higher compliance, and would report increased satisfaction with the process when compared with controls. We found that, overall, all the patients enrolled in the study responded to the survey questions positively. Survey data were collected from the parents and not from the child directly. Anecdotally, our research coordinator reported that patients who received the cartoon seemed very engaged in the process of learning about colonoscopy preparation.
The primary limitation to this study was the small sample size, which may not reflect the challenges in the greater patient population. One barrier to enrollment was exclusion of non-English-speaking patients, for whom the addition of a visual learning aid may be of greater benefit as this subgroup represents a significant portion of patients seen in the gastroenterology clinic at St Christopher’s Hospital for Children. Translating the cartoon into other languages including Spanish would potentially include those families who would benefit most. Outpatient colonoscopies are also scheduled at several satellite offices, which were unable to recruit patients due to lack of availability of appropriately trained staff to enroll patients and teach the cartoon.
The most significant finding was the overall negative correlation between level of education of the parent and the Ottawa score (which corresponds to a positive association between education and quality of bowel preparation, since the Ottawa scale has 0 as the ideal). This correlation was also seen in the control group, but not the intervention group. In the intervention group, receiving the cartoon equalized the average Ottawa scores between higher and lower education levels, but did not improve the scores to the level of the highly educated parents in the control group. We made an assumption that the parent completing the questionnaire was the same parent helping the child with bowel preparation at home.
Conclusion
Quality of bowel preparation was good in the overall study population. Objective quality of bowel preparation was not improved when a supplemental educational cartoon was used in this pilot study. Small sample size was a limitation of this study.
We believe this initial pilot study has provided insight into the role of parental education on quality of bowel preparation prior to colonoscopy in children. There may be benefit to further investigation of educational cartoons specifically in parents with less than college level education or non-English-speaking families in a larger population of patients. Future studies should also focus on logistical and resource barriers beyond education to adequate bowel preparation. Further studies could also assess the impact of educational cartoons on the child’s experience and understanding of bowel preparation, distinct from a parent’s experience.
Practice Implications
Communication and counseling surrounding bowel preparation is critical to success of colonoscopy in children. Parental education may play a role in the quality of bowel preparation. Validation of novel patient education tools to improve patient comprehension and adherence should be a priority.
Acknowledgments
We thank Hilarie and Joe Staton for cartoon artwork.
Footnotes
Authors’ Note: The funding sources did not play any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the report for publication.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: NASPGHAN In-Office Member Grant and Drexel University College of Medicine PHEC Grant.
References
- 1. Hunter A, Mamula P. Bowel preparation for pediatric colonoscopy procedures. J Pediatr Gastroenterol Nutr. 2010;51:254-261. [DOI] [PubMed] [Google Scholar]
- 2. Fatima H, Johnson CS, Rex DK. Patients’ description of rectal effluent and quality of bowel preparation at colonoscopy. Gastrointest Endosc. 2010;71:1244-1252e2. [DOI] [PubMed] [Google Scholar]
- 3. Abbott SA. The benefits of patient education. Gastroenterol Nurs. 1998;21:207-209. [DOI] [PubMed] [Google Scholar]
- 4. Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59:482-486. [DOI] [PubMed] [Google Scholar]
- 5. Lebwohl B, Wang TC, Neugut AI. Socioeconomic and other predictors of colonoscopy preparation quality. Dig Dis Sci. 2010;55:2014-2020. [DOI] [PubMed] [Google Scholar]
- 6. Vukmir RB, Kremen R, Ellis GL, DeHart DA, Plewa MC, Menegazzi J. Compliance with emergency department referral: the effect of computerized discharge instructions. Ann Emerg Med. 1993;22:819-823. [DOI] [PubMed] [Google Scholar]
- 7. Delp C, Jones J. Communicating information to patients: the use of cartoon illustrations to improve comprehension of instructions. Acad Emerg Med. 1996;3:264-270. [DOI] [PubMed] [Google Scholar]
- 8. Abrams MA, Dreyer BP, eds. Plain Language Pediatrics: Health Literacy Strategies and Communication Resources for Common Pediatric Topics. Elk Grove Village, IL: American Academy of Pediatrics; 2009. [Google Scholar]
- 9. McDermott TJ. Cartooning: a humorous approach to medical and health education. J Biocommun. 1989;16:20-27. [PubMed] [Google Scholar]
- 10. Shaikh AA, Hussain SM, Rahn S, Desilets DJ. Effect of an educational pamphlet on colon cancer screening: a randomized, prospective trial. Eur J Gastroenterol Hepatol. 2010;22:444-449. [DOI] [PubMed] [Google Scholar]
- 11. Rosenfeld G, Krygier D, Enns RA, Singham J, Wiesinger H, Bressler B. The impact of patient education on the quality of inpatient bowel preparation for colonoscopy. Can J Gastroenterol. 2010;24:543-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tae JW, Lee JC, Hong SJ, et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastrointest Endosc. 2012;76:804-811. [DOI] [PubMed] [Google Scholar]



