Abstract
Tumors of the upper trachea are typically treated by tracheal resection and reconstruction via neck incision under general anesthesia. In recent years, non-intubated thoracic surgery has been widely applied for the treatment of lung diseases due to its advantages including quick postoperative recovery. In this article, we describe the application of non-intubated tracheal resection and reconstruction in one patient for the treatment of a mass in upper trachea.
Keywords: Video-assisted thoracoscopic surgery (VATS), surgery, tracheal mass, non-intubated anesthesia, resection, reconstruction
Introduction
The surgical treatment of tracheal tumors is highly challenging (1). Tracheal resection and reconstruction under general anesthesia is typically applied, during which tracheal intubation and mechanical ventilation is often required. In recent years, non-intubated thoracic surgery has been widely applied for the treatment of lung diseases due to its advantages including fewer surgery-associated complications and quicker postoperative recovery (2). In our center, up to 1,400 non-intubated lung surgeries including lobectomy, segmentectomy, and lung volume reduction surgery have been performed since 2011 (3). In this article, we describe the application of non-intubated tracheal resection and reconstruction in one patient for the treatment of a mass in upper trachea.
Case presentation
Patients
A 44-year-old non-smoking female patient was presented to our center due to progressively aggravated dyspnea for over three months and the accompanying cough. Chest computed tomography (CT) showed a mass located at the right upper section of the trachea and at the thoracic vertebrae T2, about 5 cm away from carina. The mass could be clearly seen under contrast-enhanced CT, with a size of 1.4 cm × 1.3 cm × 1.2 cm (Figure 1). Bronchofiberscopy showed that there was a spherical mass inside the trachea, and the tumor almost complete blocked the trachea. Since the shortness of breath and dyspnea were gradually worsening, bronchofiberscopic resection of tracheal tumor was performed to alleviate the respiratory symptoms. The postoperative pathology confirmed that the lesion was an adenoid cystic carcinoma (Figures 2,3). Postoperative chest CT indicated that there was still about 1 cm of residual tumor inside the trachea (Figure 4). In order to achieve satisfactory effectiveness of radical treatment, we further discussed the disease condition and treatment protocol with the patient and her family and with other colleagues in our department and then decided to carry out non-intubated resection of tracheal mass and reconstruction of trachea.
Figure 1.
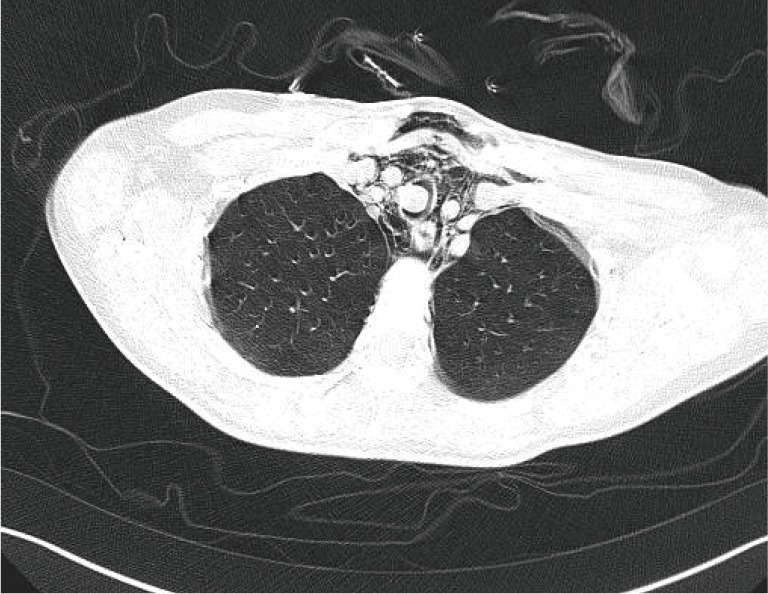
Preoperative CT showed that a mass was located inside the upper trachea at the entrance to the rib cage and blocked the tracheal lumen; emphysema in the mediastinal area could be observed. CT, computed tomography.
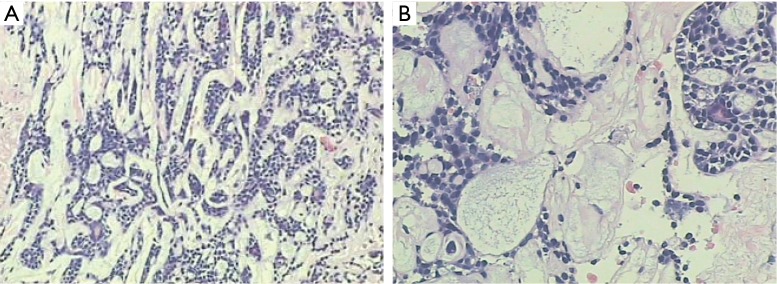
Figure 2.
Pathology result showed that tumor was located outside the tracheal cartilage and was morphologically consistent with tumors arising from salivary gland. The tumor was judged to be an adenoid cystic carcinoma (magnification, ×200).
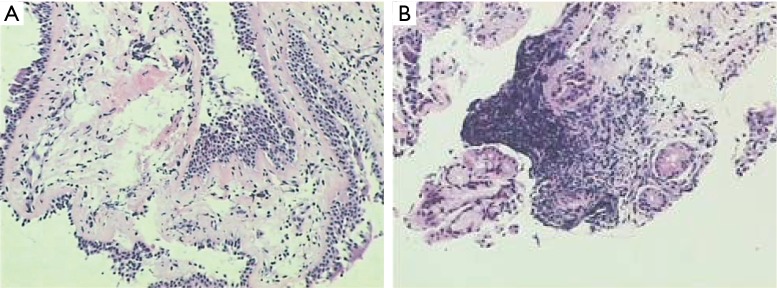
Figure 3.
Multiple specimens were collected at sites 1 and 5 cm away from the tumor, 1 cm under the glottis, and at the carina. Five bronchial mucosal specimens were sent for pathologic examination, which showed submucosal edema and infiltration of many lymphocytes; while chronic inflammation was identified, no tumor was found (magnification, ×200).
Figure 4.

Chest CT following interventional therapy showed that most of the tumor was resected after interventional therapy with bronchoscopic electrocautery; however, tumor tissue still could be found at the basal part, which could be a clue in the judgment of resection margin after radical treatment. CT, computed tomography.
Anesthesia
Intravenous anesthesia plus cervical plexus local anesthesia were applied. Also, 40% oxygen was delivered using a laryngeal mask at a rate of 3.5 mL/min. The patient remained awake throughout the surgery. The depth of anesthesia was measured using the EEG bispectral index during the surgery. Finally, devices for tracheal intubation and mechanical ventilation were also prepared to prevent emergency situation (e.g., airway obstruction) and ensure the surgical safety.
Surgical process
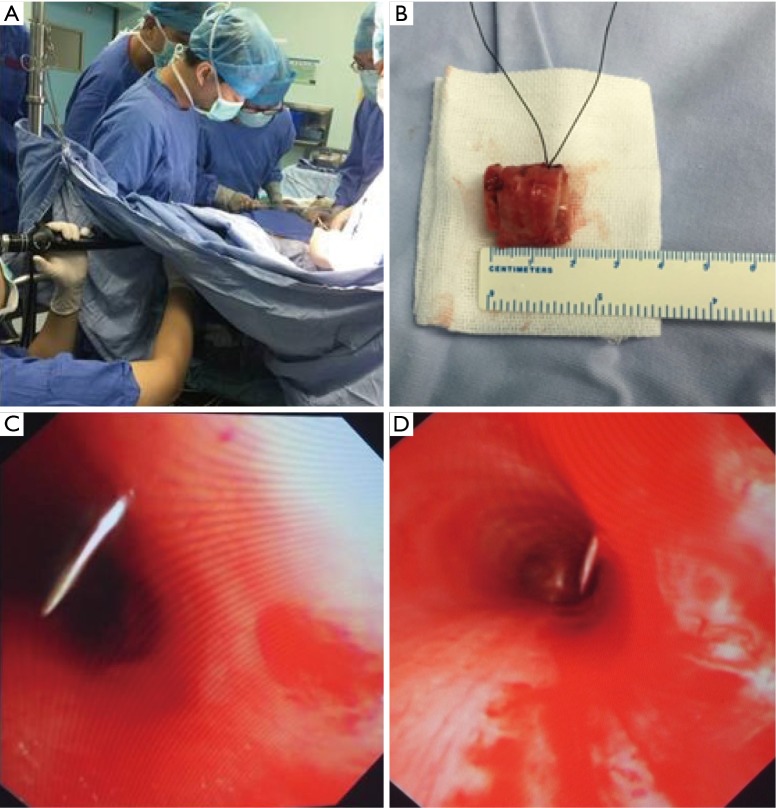
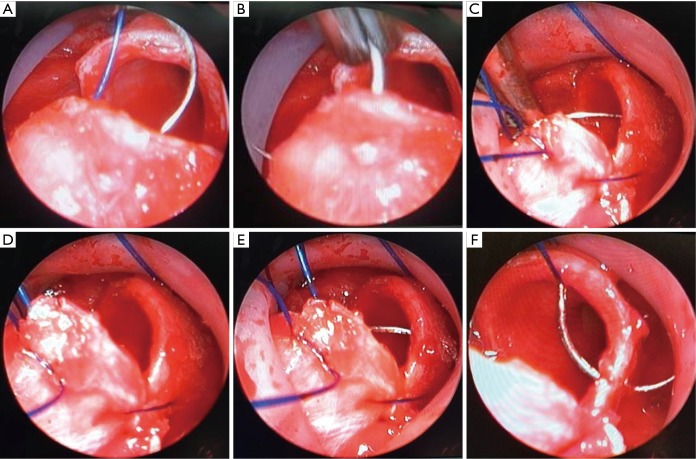
The patient was asked to take a neck hyperextension position and the laryngeal mask airway was used. A 3-cm arc incision was made in the neck (Figure 5). The trachea was carefully dissociated to avoid any injury to the recurrent laryngeal nerve (Figure 6). The resection scope was decided by bronchofibroscopy (Figure 7). The dissociated trachea was 4 cm in length. The tracheal mass was resected about 1 cm away from the tumor edge, and the length of the resected part was 2 cm. Intra-operative frozen section analysis showed that the surgical margin was negative. After the reconstruction of the tracheal stump by continuous suture using 2–0 Prolene sutures, anastomotic leak test was performed using sterile saline (Figure 8). Oxygen was delivered through a nasal cannula to prevent hypoxemia. The neck incision was closed after it was confirmed that there was no anastomotic leak or active bleeding. The operation lasted 120 min. The intraoperative blood loss was 10 mL. The patient’s vital signs remained stable throughout the operation. Two hours after the surgery, the patient became ambulatory inside the ward; and 3 hours later, normal diets were fed. A second chest CT was performed 6 months after the surgery, and no tumor-related sign was found (Figure 9).
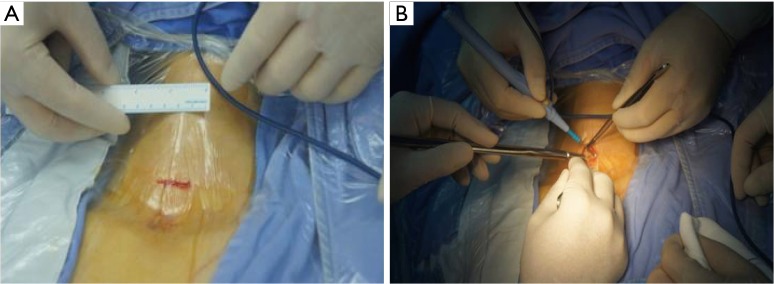
Figure 5.
Selection of surgical incisions: a 3.5-cm “collar” incision (with incision protector) was made 2 cm above the suprasternal notch.
Figure 6.
Surgical step: tissues near the trachea were released with the assistance of mediastinoscope.
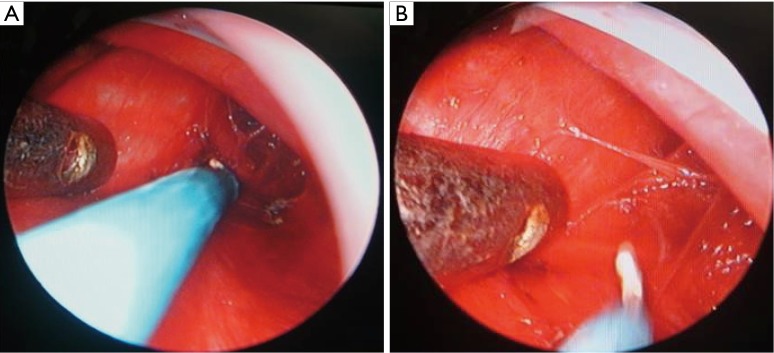
Figure 7.
Surgical step: the resection margins at the upper and lower ends of the trachea were decided based on preoperative imaging and intraoperative fibrobronchoscopy.
Figure 8.
Surgical step: intraoperative pathological frozen-section analysis showed that the resection margins at both the upper and lower ends of trachea were negative, and no carcinoma was found in the tracheal tissue specimens. Tracheal end-to-end anastomosis and reconstruction were then performed. The distal and proximal tracheal anastomoses were continuously sutured using 3–0 Prolene sutures.
Figure 9.

Postoperative fibrobronchoscopy showed that the anastomoses were patent. No obvious twisting, stricture, or active bleeding was in the trachea.
The length of trachea to be resected was about 2 cm. The tumor did not invade the adjacent tissues, blood vessels, or nerves.
The postoperative recovery was good, and the wound healing was satisfactory. The postoperative pathology of the paraffin-embedded surgical specimens showed same results as the in homogenized and frozen specimens. The patient was discharged on the third postoperative day. Postoperative chest CT showed that the anastomoses grew well and the trachea was patent.
Postoperative conditions
Postoperative chest X-ray showed that the operated lung was well re-expanded and there was no sign of pneumothorax. The patient had no postoperative symptoms such as nausea and vomiting but complained of mild pain at the surgical site. Non-steroidal anti-inflammatory drugs and ambroxol were administered to alleviate the symptom. There was no surgery-related complication. On day 3, the patient was discharged. During the 6-month follow-up, the patient had good general conditions and did not complain of any respiratory symptom.
Postoperative diagnosis
The mass was pathologically diagnosed as adenoid cystic carcinoma of the trachea invading the bronchial wall. The mass was sized 1.4 cm × 1.3 cm × 1.2 cm, and it had protruded into the tracheal lumen. The stump was pathologically confirmed to be negative.
Discussion
Primary ACC is usually managed by circumferential tracheal resection with primary anastomosis performed under an open surgical technique. In this case, the lesion presented in the upper portion of the trachea, and the tumor was removed via a transcervical surgical method. We selected this method as a result of the tumor location, high chance of recurrence from residual tumor, and the non-intubated anesthesia experience in our institution. According to our experiences, non-intubated video-assisted thoracoscopic surgery (VATS) surgeries have many advantages (3).
Traditional anesthesia for trachea procedures offers distinct challenges and requires careful coordination between the surgical and anesthesia teams during airway excision and anastomosis. In our institution, anatomic VATS under spontaneous breathing anesthesia has shown promising results (3). Therefore, we chose spontaneous respiration intravenous anesthesia with spontaneous breathing for endotracheal tumor resection and reconstruction. This method significantly benefits the patient by eliminating the negative effects generally caused by endotracheal intubation allowing the patient a fast recovery (4).
However, the non-intubated procedure should be avoided in patients with the following conditions: (I) low cardiac output due to aortic stenosis, hypertrophic cardiomyopathy, severe arrhythmia, mitral stenosis, or complete atrioventricular block; (II) American Society of Anesthesiologists (ASA) score >3; (III) BMI >25 kg/m2; (IV) pulmonary insufficiency (FEV1<60% expected value) and/or poorly controlled asthma; (V) severe pleural adhesions; (VI) heart failure, abnormal anatomical structures, or spinal cord and peripheral nerve diseases; and (VII) low blood volume, hemodynamic instability, or dysfunction of blood coagulation.
During the procedure, endotracheal intubation, thoracoscopic intubation, and mechanical ventilation should also be prepared for the safety consideration. Endotracheal intubation or thoracoscopic intubation should be performed immediately in case the following conditions: (I) the SpO2 was lower than 90%; (II) continuous carbon dioxide retention, along with the development of respiratory acidosis; and (III) sudden uncontrollable bleeding (5).
In conclusion, tracheal resection and reconstruction under spontaneous breathing anesthesia via a transcervical surgical method is a feasible operation and may provide an alternative method for the treatment of upper tracheal tumors.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Grillo HC. Development of tracheal surgery: a historical review. Part 1: Techniques of tracheal surgery. Ann Thorac Surg 2003;75:610-9. 10.1016/S0003-4975(02)04108-5 [DOI] [PubMed] [Google Scholar]
- 2.Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg 2007;32:346-50. 10.1016/j.ejcts.2007.04.029 [DOI] [PubMed] [Google Scholar]
- 3.Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. 10.1177/1553350614531662 [DOI] [PubMed] [Google Scholar]
- 4.Hung MH, Cheng YJ, Chan KC, et al. Nonintubated uniportal thoracoscopic surgery for peripheral lung nodules. Ann Thorac Surg 2014;98:1998-2003. 10.1016/j.athoracsur.2014.07.036 [DOI] [PubMed] [Google Scholar]
- 5.Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. 10.1016/j.athoracsur.2004.05.083 [DOI] [PubMed] [Google Scholar]