Abstract
Objective
To systematically review previous studies and to assess, via a subgroup meta-analysis, the combined odds ratio (OR) of prognostic factors affecting the success of miniscrew implants (MIs) inserted into the buccal posterior region.
Methods
Three electronic searches that were limited to articles on clinical human studies using MIs that were published in English prior to March 2015 were conducted. The outcome measure was the success of MIs. Patient factors included age, sex, and jaw of insertion (maxilla vs. mandible), while the MI factors included length and diameter. A meta-analysis was performed on 17 individual studies. The quality of each study was assessed for non-randomized studies and quantified using the Newcastle-Ottawa Scale. The meta-analysis outcome was a combined OR. Subgroup and sensitivity analyses based on the study design, study quality, and sample size of miniscrews implanted were performed.
Results
Significantly higher success rates were revealed for MIs inserted in the maxilla, for patients ≥ 20 years of age, and for long MIs (≥ 8 mm) and MIs with a large diameter (> 1.4 mm). All subgroups acquired homogeneity, and the combined OR of the prospective studies (OR, 3.67; 95% confidence interval [CI], 2.10-6.44) was significantly higher in the maxilla than that in the retrospective studies (OR, 2.10; 95% CI, 1.60-2.74).
Conclusions
When a treatment plan is made, these risk factors, i.e. jaw of insertion, age, MI length, and MI diameter, should be taken into account, while sex is not critical to the success of MIs.
Keywords: Subgroup meta-analysis, Miniscrew implant, Success rate, Prognostic factor
INTRODUCTION
Although many studies have investigated the various prognostic factors affecting the success of miniscrew implant (MI) insertion, conflicting results have made the identification of critical factors difficult. For instance, while some studies did not identify any significant differences between the success rates of MIs inserted in the mandible and those inserted in the maxilla,1,2,3 others found that MIs inserted in the maxilla had higher success rates compared to MIs inserted in the man dible.4 Similarly, conflicting results have been reported with respect to sex,2,5,6,7 age,6,7,8 MI length,8,9 and MI diameter.4,10
To identify patterns among the results of different studies, a meta-analysis can be applied. Meta-analyses are able to combine the outcomes of multiple studies into a single quantitative estimate, although statistical heterogeneity remains inevitable because of clinical and methodological differences among the studies. For example, Dalessandri et al.11 performed a meta-analysis to investigate the factors that influence the success rates of temporary skeletal anchorage devices and found that treatment effects based on the patients' sex and age and on the MI insertion site among the studies were heterogeneous, and stated that this heterogeneity made it difficult to form conclusions. Thus, since the results of meta-analyses obtained by combining such heterogeneous effects are prone to errors, it is necessary to specify a procedure to identify or eliminate the source of heterogeneity when evaluating the outcomes obtained from diverse studies. En-masse retraction, canine retraction, and intrusion of posterior teeth are the three most common utilizations of the miniscrew. Clinically, placing the miniscrews in the buccal regions is easier, less variable, and more consistent. Since inconsistent success rates can contribute to the heterogeneity, the present meta-analysis was performed on the success rates of MIs placed in the buccal area only.
The aim of this study was to systematically review previous studies that addressed prognostic factors affecting the success of MIs inserted into the buccal posterior region. Specifically, we assessed the combined odds ratio (OR) of the success of MIs with respect to factors such as sex, age, jaw of insertion (mandible or maxilla), MI length, and MI diameter via a subgroup meta-analysis based on the study design, study quality, and sample size of miniscrews implanted.
MATERIALS AND METHODS
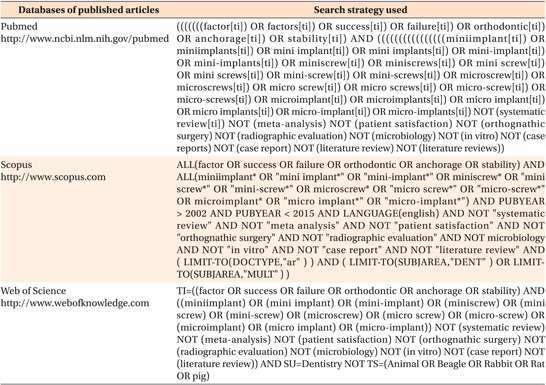
Procedures for the meta-analysis complied with the Cochrane Handbook for Systematic Reviews of Interventions and the PRISMA statement.12 MEDLINE (PubMed), Scopus, and Web of Science electronic searches for articles in English on clinical human studies published from January 2003 to March 2015 were conducted using the following search terms: factor(s), screw(s), implant(s), anchorage, success, stability, miniscrew(s), microimplant(s), and microscrew(s) (Appendix 1). Morrison et al.13 found that language other than English (LOE) studies tend to have lower quality and exaggerated treatment effects than studies in English, and a few LOE studies included in the meta-analysis can not represent all the LOE studies. Hence, the studies were limited to English since LOE studies may impose a bias in systematic review based meta-analyses and the quality of meta-analysis relies mainly on the quality of included studies.13,14 In addition, manual searches of the reference list of electronically detected articles were performed, and a grey literature search was carried out using Google Scholar.
Study selection
The searches and article selection were performed by three independent authors (SBH, EJK, and BK). Two authors (SBH and EJK) independently made a preliminary list of articles by screening the titles and abstracts for the meta-analysis and evaluated the full manuscript of studies with appropriate inclusion criteria to make a decision; Cohen's kappa was 0.88, indicating almost perfect inter-rater agreement. Discordance in article selection was resolved by debate and consultation with another author (BK). As a result, 17 articles were selected for the analyses.
Inclusion criteria
The outcome measure was converted into a dichotomous value: 0 for loosened MIs, and 1 for unloosened MIs. Unloosed MIs were considered successful, while loosened MIs were considered unsuccessful. Five confounding factors were divided into two categories: patient factors and MI factors. The patient factors were age (< 20 years vs. ≥ 20 years), sex (male vs. female), and the jaw of insertion (maxilla vs. mandible), while the MI factors were length (< 8 mm vs. ≥ 8 mm) and diameter (≤ 1.4 mm vs. > 1.4 mm). The following criteria were used to select the articles: 1) studies on the stability of screws and implants when both items were used for orthodontic anchorage; 2) human clinical studies; 3) prospective and retrospective studies; 4) studies on MIs inserted into the posterior buccal region; and 5) studies that reported the success rates of MIs or explicitly included information that would enable a computation of the success rate with regards to any of the five confounding factors.
Exclusion criteria
Exclusion criteria included articles related to the following: (1) systematic review or meta-analysis, (2) patient satisfaction, (3) orthognathic surgery, (4) radiographic evaluation, (5) microbiology, (6) case report, (7) in vitro studies, (8) literature review, (9) only one article from a particular research group, (10) studies based on the five confounding factors that used different dichotomizations (e.g., the age division of < 18 years vs. ≥ 18 years), and (11) studies on MIs inserted into the retromolar pad, lingual side, or palatal side. Since one of the assumptions of the meta-analysis was independence between studies, studies from specific authors were included only once and studies from coauthors of the chosen studies were excluded.
Data extraction
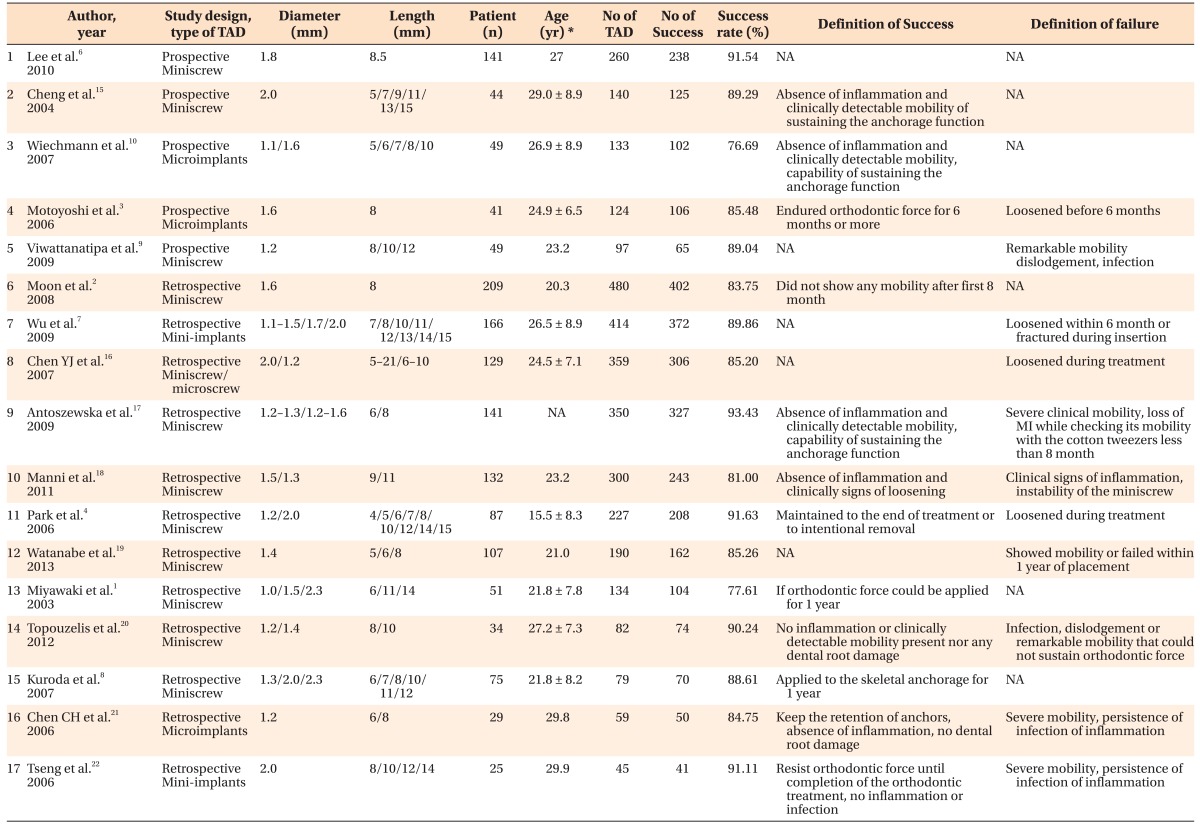
The following information was extracted from the 17 included studies: the first author's name, publication year, study design, type of temporary anchorage device (TAD), diameter and length of the MIs, number of patients, mean age of the patients, number of TADs, number of successes, success rate, definition of success and failure (Table 1).1,2,3,4,6,7,8,9,10,15,16,17,18,19,20,21,22 The ORs of the success of MIs with respect to these factors were directly calculated using the number of stable MIs and the number of inserted MIs for each category. The ORs calculated from the raw data were double-checked by two authors (SBH, HJL). The success of MIs was defined as the absence of clinically detectable mobility when the orthodontic force applied by a clinician was sustained regardless of the predetermined period, as the predetermined period varied between studies (Table 1).1,2,3,4,6,7,8,9,10,15,16,17,18,19,20,21,22
Table 1. General characteristics of the studies included in the meta-analysis.
MI, Miniscrew implant; TAD, temporary anchorage device; NA, not available.
*Mean or mean ± standard deviation.
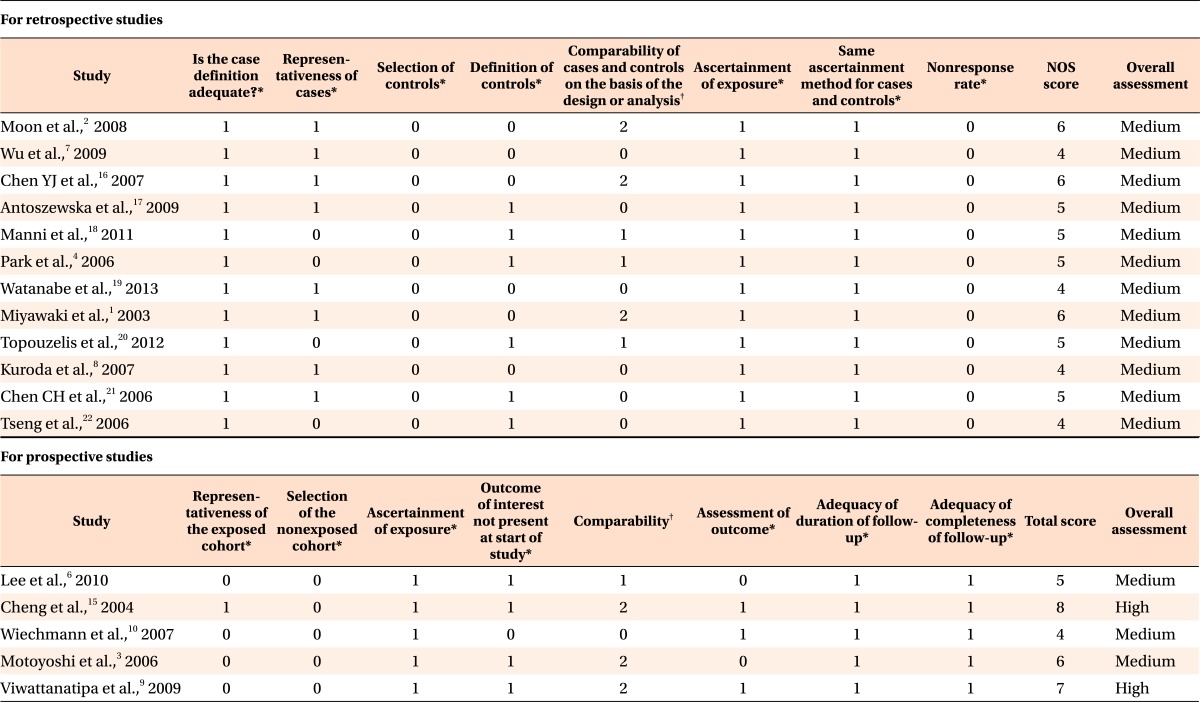
Quality assessment
The quality of the studies was assessed for nonrandomized studies and then quantified using the 9-star Newcastle-Ottawa Scale (NOS),23 which is recommended by the Cochrane collaboration. The study quality was evaluated as being low (0-3 points), medium (4-6 points), or high (7-9 points). The NOS includes eight criteria for evaluating the quality of the included studies (Table 2),1,2,3,4,6,7,8,9,10,15,16,17,18,19,20,21,22 and these criteria are based on the following three categories: subject selection, comparability between groups, and outcome measurement. Any dis agreements were resolved by consensus.
Table 2. Newcastle-Ottawa Scale (NOS) summary assessment of risk of bias.
*Yes=1 point, No=0 point; †number of variables controlled for in analysis (maximum value=2).
Meta-analysis
The outcome of the meta-analysis was expressed as a combined OR since the OR can be used as the effect size for the three major study designs: cross-sectional, prospective, and retrospective.24,25 The OR in each study was defined as the ratio of the odds (success/failure) of the MIs in two categories: patient factors and MI factors. In the jaw, an OR greater than 1 indicates that successful MIs are more likely to be located in the maxilla (jaw = 1), whereas an OR less than 1 indicates that successful MIs are more likely to be located in the mandible (jaw = 0). Heterogeneity was tested by the Cochran Q and I2 statistic; if the p-value of the Q test is greater than 0.10, then no significant heterogeneity exists. It was tentatively suggested that low heterogeneity may be associated with I2 values of less than 30%, while substantial heterogeneity may be associated with I2 values of over 50%; if significant heterogeneity was identified, then additional subgroup and sensitivity analyses were performed and a qualitative review of the study was conducted until the causes of the heterogeneity were clearly determined.
Subgroup meta-analysis
The studies included in the meta-analysis differed in terms of their study design, participant characteristics, and treatment goals. Variability among these studies in a systematic review may be taken as heterogeneity. To investigate the source of the heterogeneity, a subgroup analysis can be used to answer specific questions about particular groups of patients, the type of intervention, or the type of study. In this study, subgroups were created based on the study design (retrospective study vs. prospective study), study quality (medium vs. high), and sample size of miniscrews implanted (< 200 vs. ≥ 200). A meta-analysis was performed for each subgroup, and the results were reported separately.
Sensitivity analysis
A sensitivity analysis is a collective method for verifying the robustness of results. We performed sensitivity analyses to assess the impact of each study on the combined effect size. The meta-analysis was repeatedly performed as follows: a meta-analysis that included all studies except the first study was performed followed by a meta-analysis that included all studies except the second study and so on until each study was excluded once. If the statistical significance of the result was influenced by removing one of the studies, the removed study was reviewed again to confirm the source of the heterogeneity.
Publication bias
Funnel plots have been widely used to detect the potential publication bias of studies in a meta-analysis. However, because the visual interpretation of funnel plots largely depends on the subjective impression of the observer,26 Begg's rank correlation test27 and Egger's linear regression test28 were used as more objective tests to detect publication bias in the present meta-analysis. Significant results (p < 0.05) suggest publication bias. Bias-corrected estimates were calculated using the trim-and-fill method, which accounts for unpublished data by imputing missing studies to yield an unbiased estimate of the effect size.
Meta-analyses and sensitivity analyses were performed using RStudio (ver. 0.96.315; RStudio Inc., Boston, MA, USA) and Comprehensive Meta-Analysis software (ver. 2.0; Biostat, Englewood, NJ, USA).
RESULTS
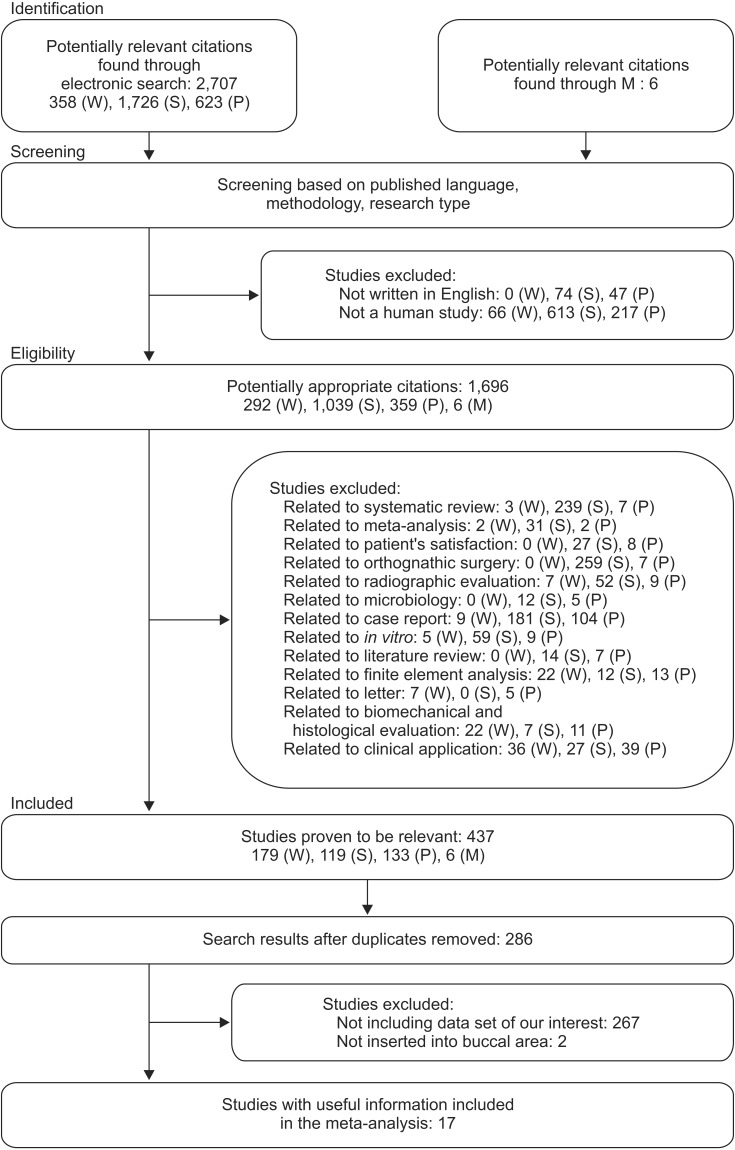
The preliminary electronic search identified 2,707 relevant articles. Articles that were not in English and that were not human clinical studies were excluded. Among the remaining 1,696 articles, additional articles were excluded from based on the aforementioned exclusion criteria. After removing duplicate publications, 286 articles remained and were manually reviewed to determine whether they provided information that would facilitate the computation of the MI success rate with respect to any of the five confounding factors. Finally, 17 articles that satisfied all of the inclusion criteria were selected (Figure 1); a list of the included studies is shown in Table 1.1,2,3,4,6,7,8,9,10,15,16,17,18,19,20,21,22
Figure 1. PRISMA flow diagram of the search strategy for the prognostic factors associated with the success rates of posterior orthodontic miniscrew implants. W, Web of Science; S, Scopus; P, PubMed; M, manual search.
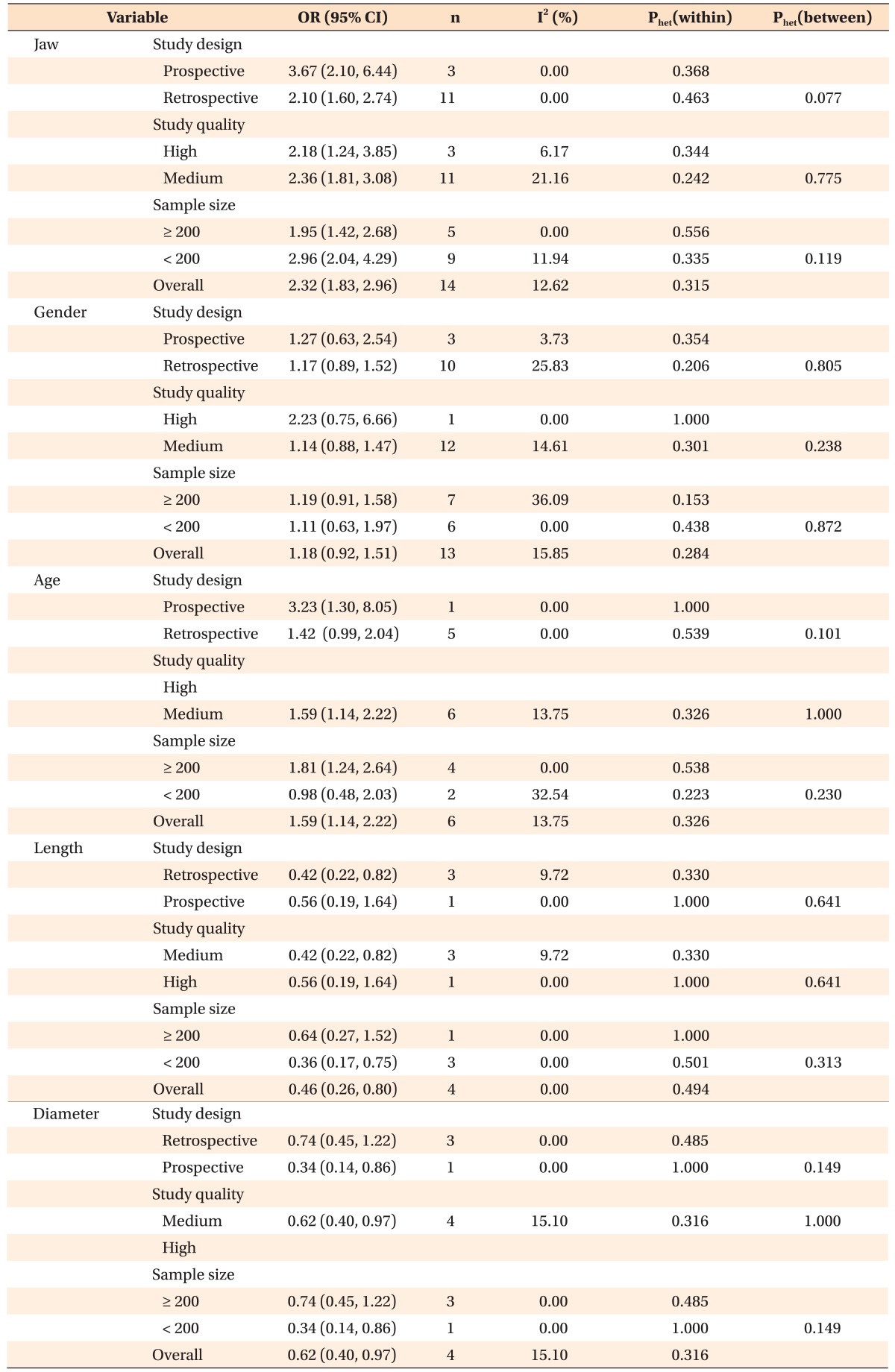
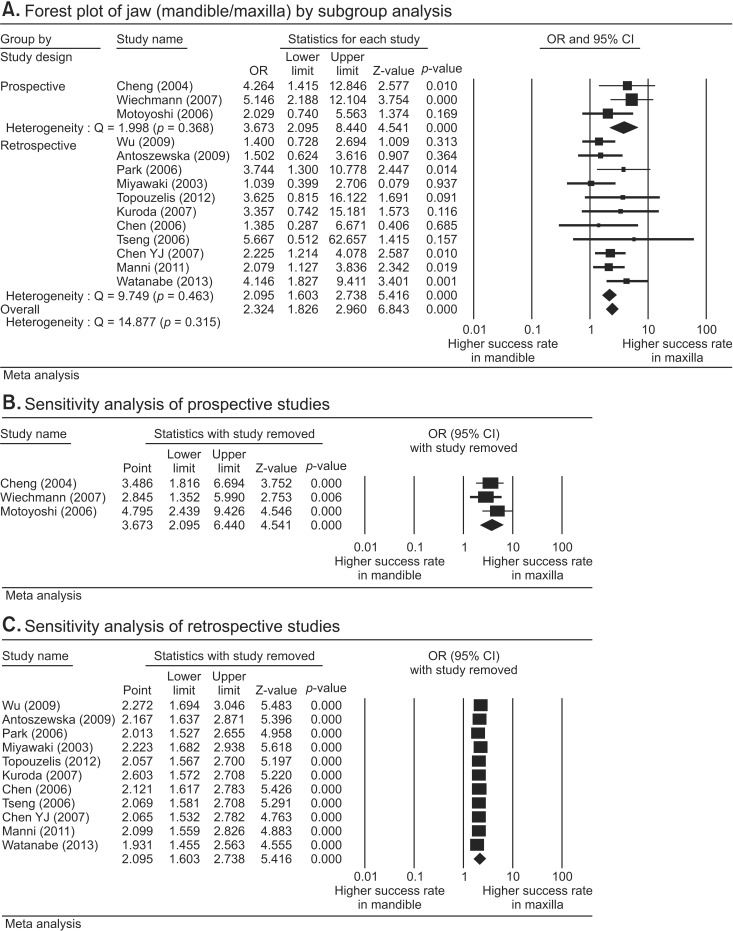
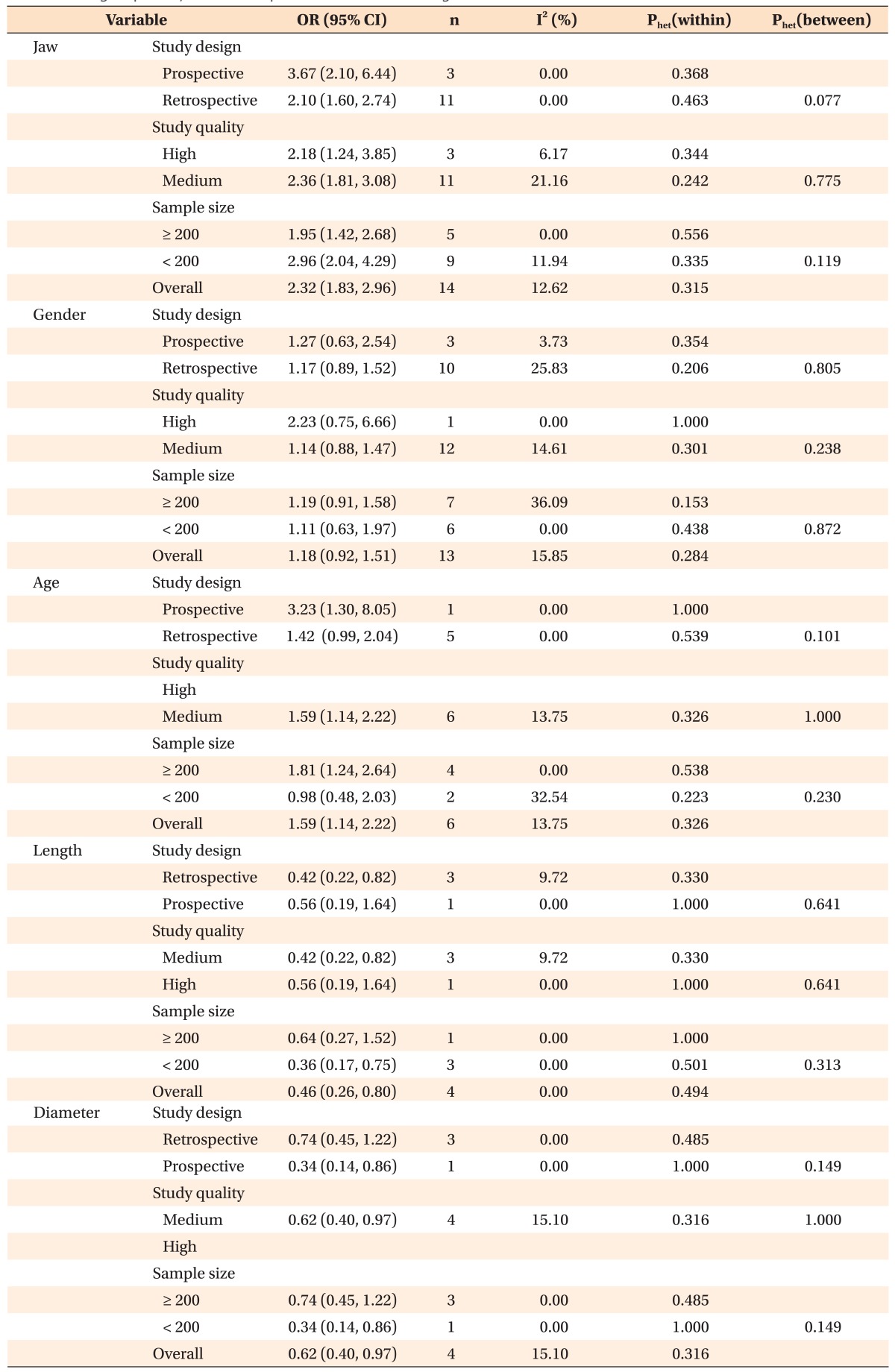
To investigate differences in the MI success rates with regards to the jaw of insertion (maxilla vs. mandible), 14 studies were used; three studies were excluded since they did not provide success rates that specified the jaw of insertion. Given the homogeneity (phet[within] > 0.1) demonstrated by the 14 studies, the combined OR of 2.32 (95% confidence interval [CI], 1.81-4.08) indicated that MIs inserted in the maxilla had a significantly higher success rate (2.32 times higher) compared to MIs inserted in the mandible. The subgroups that were based on the study design, study quality, and sample size each acquired homogeneity (I2 < 25% and phet[within] > 0.1). The combined OR of the prospective studies was higher (OR, 3.67; 95% CI, 2.10-6.44) than that of the retrospective studies (OR, 2.10; 95% CI, 1.60-2.74), and the treatment effects differed between the subgroups (phet[between] = 0.077 < 0.1). The combined OR of high-quality studies (OR, 2.18; 95% CI, 1.24-3.85) was lower than that of medium-quality studies (OR, 2.36; 95% CI, 1.81-3.08), though the treatment effects did not differ between the subgroups (phet[between] > 0.1). The subgroup of five studies with sample sizes of more than 200 MIs had a combined OR of 1.95 (95% CI, 1.42-2.68), while the subgroup of nine studies with sample sizes of less than 200 MIs had a combined OR of 2.96 (95% CI, 2.04-4.29). Consequently, the subgroup meta-analysis revealed significantly higher success rates in the maxilla than in the mandible. Moreover, the sensitivity analysis showed that none of the studies significantly changed the overall results of the subgroup analysis (Table 3, Figure 2).
Table 3. Subgroup analyses with respect to five confounding factors.
Phet(within), heterogeneity within subgroups; Phet(between), heterogeneity between subgroups.
I2 > 50: substantial heterogeneity.
OR, Odds ratio; CI, confidence interval.
Figure 2. A, Forest plot of odds ratios (ORs) for success rates between mandible and maxilla. Homogeneous subgroup of prospective studies showed combined OR of 3.67 (95% confidence interval [CI], 2.10-6.44)*, and homogeneous subgroup of retrospective studies showed a combined OR of 2.10 (95% CI, 1.60-2.74)*. B, In the sensitivity analysis for prospective studies regarding jaw, a significantly higher success rate in the maxilla was shown. C, The sensitivity analysis of retrospective studies regarding jaw showed a higher success rate in the maxilla. *Sig nificance.
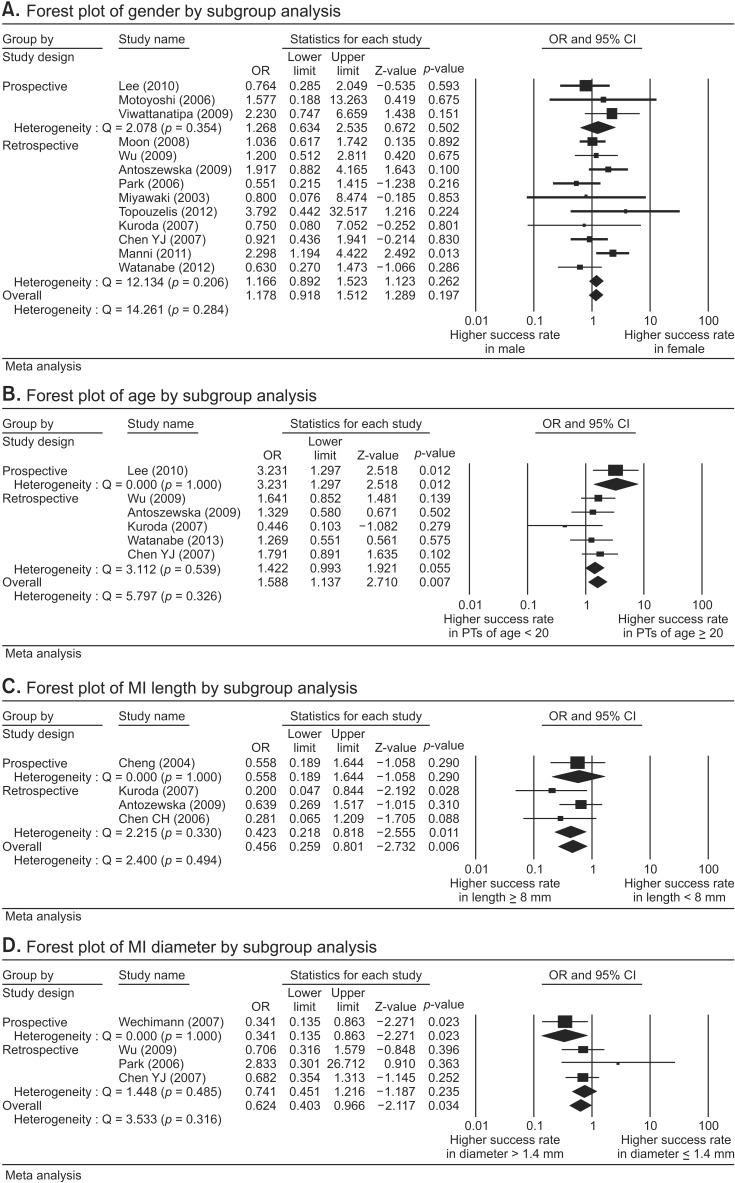
In another meta-analysis investigating the difference in MI success rates according to sex, 13 of the 17 studies were considered; four studies were excluded since they did not provide the success rates according to sex. Given the homogeneity (phet[within] > 0.1) demonstrated by the 13 studies, the combined OR of 1.18 (95% CI, 0.92-1.51) indicated that the success rates were not significantly different between the two sexes. The subgroup of prospective studies showed homogeneity (I2 = 3.73 and phet[within] > 0.1), with a combined OR of 1.27 (95% CI, 0.63-2.54). The subgroup of retrospective studies also showed homogeneity (I2 = 25.83 and phet[within] = 0.206 > 0.1) and had a combined OR of 1.17 (95% CI, 0.89-1.52). Accordingly, no significant sex difference was found with regards to the MI success rate in either subgroup. Similar results were obtained in the subgroup analyses based on study quality and sample size. Furthermore, the sensitivity analyses of the subgroups showed that none of the studies significantly changed the overall results (Table 3, Figure 3A).
Figure 3. Forest plot of odds ratio for success rates. A, Bet ween males and females. The results in both subgroups showed no significant difference in success rates. B, Between age groups. Homogeneous subgroups showed higher success rates in patients aged 20 years and over (≥ 20 years) except subgroup of retrospective studies and studies with small samples. C, Between long miniscrew implants (MIs) (≥8 mm) and short MIs (<8 mm). Long MIs had significantly higher success rates. D, Between large diameter (>1.4 mm) and small diameter (≤1.4 mm) screws. MIs with large diameters had significantly higher success rates.
For the meta-analysis investigating differences in the MI success rates according to patient age, six studies were considered. Most of the excluded studies reported only the mean age and standard deviation, while the study by Moon et al.2 was excluded because of a different age dichotomization (over/under 18 years of age). Additionally, the study by Miyawaki et al.1 was excluded because the number of patients was used to calculate the frequency of the age categories instead of the number of TADs, unlike the other studies included in the present meta-analysis. Based on the homogeneity (phet[within] > 0.1) demonstrated by the six studies, the combined OR of 1.59 (95% CI, 1.14-2.22) indicated that MIs inserted in patients who were 20 years of age and over had a significantly higher success rate (1.53 times higher) than did MIs inserted in patients who were under the age of 20 years. A subgroup of one prospective study and another subgroup of retrospective studies acquired homogeneity (I2 = 0.00 and phet[within] > 0.1). The combined OR of the prospective study (OR, 3.23; 95% CI, 1.30-8.05) was higher than that of the retrospective studies (OR, 1.42; 95% CI, 1.03-1.96), but treatment effects did not differ between the subgroups (phet[between] = 0.101 > 0.1) (Table 3, Figure 3B).
For the meta-analysis investigating the difference in MI success rates based on MI length, four studies that collectively included 628 MIs were used. Most of the individual studies considered in our meta-analysis reported success rates based on MI length, though some of the excluded studies used only long MIs (≥ 8 mm),1,4,5,6,10,14,25 while others did not provide success rates according to MI length that were restricted to the posterior region. Based on the homogeneity (phet[within] > 0.1) demonstrated by the four studies, the combined OR of 0.46 (95% CI, 0.26-0.80) indicated that long MIs (≥ 8 mm) had success rates that were 2.17 (= 1/0.46) times higher than the rates obtained with short MIs (< 8 mm). While the combined OR of the prospective study (OR, 0.56; 95% CI, 0.19-1.64) indicated no significant differences between long and short MIs, the combined OR of the retrospective studies (OR, 0.42; 95% CI, 0.22-0.82) indicated that long MIs had significantly higher success rates than did short MIs. Homogeneity was also obtained in all subgroups based on the study design, study quality, and sample size (I2 < 25%) (Table 3, Figure 3C).
In the meta-analysis evaluating the difference in MI success rates according to MI diameter, four studies were considered. Some of the excluded studies used only one type of MI diameter. Other studies included different diameters, but did not report the success rates according to the diameter. Based on the homogeneity (phet[within] > 0.1) demonstrated by the four studies, the combined OR of 0.62 (95% CI, 0.40-0.97) indicated that MIs with large diameters (> 1.4 mm) had success rates that were 1.61 (= 1/0.62) times higher than the success rates of MIs with small diameters (≤ 1.4 mm). While the combined OR of the retrospective studies (OR, 0.74; 95% CI, 0.45-1.22) indicated that there was no significant difference in the success rates of large-diameter and small-diameter MIs, the combined OR of the prospective study by Wiechmann et al.10 (OR, 0.34; 95% CI, 0.14-0.86) showed that MIs with large diameters had significantly higher success rates than did MIs with small diameters (Table 3, Figure 3D).
Publication bias was assessed for the five factors used in our study. No publication bias was found based on the Begg's and Eggar's tests (p > 0.05), except in the subgroup of retrospective studies used to investigate age differences. If publication bias was found, a bias-corrected OR estimate that was obtained by the trim-and-fill method was used as the final outcome measure. Note that the OR values changed, and the significance of the values also changed (Table 4).
Table 4. Publication bias based on study design, study quality, and sample size of Miniscrew Implant with respect to five confounding factors.
NA, Not available.
*Adjusted odds ratio after trim and fill (adjusted 95% confidence interval) =1.53 (1.06–2.22).
DISCUSSION
The aim of this study was to systematically review previous studies that addressed prognostic factors affecting the success of MIs inserted into the buccal posterior region. The success rates of MIs inserted in the maxilla were higher than the rates of MIs inserted in the mandible. Significantly higher MI success rates were found in patients who were ≥ 20 years of age. Significantly higher success rates were also identified when long MIs (≥ 8 mm) and large diameter MIs (> 1.4 mm) were used. No significant differences were found between the success rates of MIs inserted in males and females.
Compared to similar studies, our results showed some consistencies with previous findings, but also showed some inconsistencies. For instance, Dalessandri et al.11 performed meta-analyses using the same five factors of age, sex, jaw of insertion, MI length, and MI diameter and found that sex, MI length, and MI diameter showed no significant differences in terms of the success rates of MIs. However, they also reported that MIs inserted in the maxilla had higher success rates than did MIs inserted in the mandible and that MIs inserted in older (> 20 years) patients had higher success rates than did MIs inserted in younger (< 20 years) patients. While the results of Dalessandri et al.'s study11 in terms of the success rates associated with the jaw of insertion (maxilla/mandible), sex, and age were consistent with the results of the present study, their results for the length and diameter of MIs were inconsistent with the results mentioned above. Moreover, in a study by Papageorgiou et al.,29 age, sex, MI length, and MI diameter showed no significant differences in terms of the success rates of MIs. However, they did report that MIs inserted in the maxilla had higher success rates than did MIs inserted in the mandible. Therefore, only their results for the jaw of insertion and sex were consistent with our results mentioned above, while those for age, MI length, and MI diameter were inconsistent. However, in a study by Crismani et al.,30 although only a systematic review was performed rather than a meta-analysis, they reported that short screws (< 8 mm) with small diameters (< 1.2 mm) should be avoided, which is consistent with the present results. Some consistent and inconsistent results of previous studies compared to our study were shown. Below, we discussed the results for each factor.
Jaw of insertion
The present meta-analysis was performed on the success rates of MIs inserted in the buccal area only, since the following inconsistent sucess rates contributed to the heterogeneity. MIs inserted into the anterior region and palatal side that had serious effects on the outcome were excluded from the present meta-analysis because greater root proximity in the anterior region31 and significantly higher success rates on the palatal side32 have been reported. Since the success rates of miniscrews placed in the mandibular lingual side were lower than the rates for the buccal side in Lai and Chen's study,33 the success rate in the mandible was considered to be much lower than the rate in the maxilla. On the other hand, since the retromolar area showed the highest success rate (100%) in Lin et al.'s study34 and since this area was included as part of the mandible, the success rate in the mandible was reportedly higher than the rate in the maxilla.
Furthermore, prospective studies, compared to retrospective studies, showed higher success rates for MIs inserted in the maxilla. Since prospective studies usually have fewer potential sources of bias and fewer confounding factors than retrospective studies, prospective studies are deemed more reliable than retrospective studies. The higher success rates in the maxilla than in the mandible were reportedly due to the thicker mandibular cortical bone compared to the maxillary bone, overheating of the mandibular bone during drilling, and irritation during chewing.3,4 While the insertion region in the maxilla is keratinized gingiva, it is highly possible that the mandibular insertion region is free gingiva. Therefore, gingival inflammation is more likely to occur in the mandible compared to in the maxilla. Since inflammation leads to loosening, oral hygiene management can help prevent the miniscrews from loosening. Another recommended way to reduce the MI insertion failure in the mandibular buccal posterior region is with pilot drilling, which is different from pre-drilling. During pilot drilling, the MI is inserted into the notch with the fissure bur using a hand driver.35 On the other hand, pre-drilling is a technique using a bur with a smaller diameter than the miniscrew inserted, to make an opening that has a depth less than the thread length of the miniscrew. We found that MIs inserted in the maxilla had higher success rates than did MIs inserted in the mandible regardless of the study design.
Sex
Since females tend to get more orthodontic treatments than males for esthetic reasons, the proportion of females was significantly larger in most of the studies examined in our meta-analysis. Although no heterogeneity among the 13 studies was detected, subgroup analyses were performed using the criteria of study design, study quality, and sample size of MIs; each subgroup acquired homogeneity. Although males have a higher bone mineral density than females, the success rate of MIs was not significantly different between the two sexes. These findings were consistent with the results of previous studies.36
Age
In the present meta-analysis, significantly higher success rates were identified in patients who were ≥ 20 years of age compared to in patients who were < 20 years of age. However, in studies that had a sample size of < 200 MIs, no significant differences were found between the success rates of MIs inserted in patients ≥ 20 years old and those who were < 20 years old. However, these studies had moderate heterogeneity (I2 = 32.54%), indicating that a few of the studies had different success rates. Therefore these results should be interpreted with caution. Chen et al.16 reported that adolescents had a higher chance of loosening than adults, as thin cortical bone and low bone density were linked to the increased failure of MIs. This result in which increased loosening in younger patients was consistent with the findings of the present meta-analysis. Removable appliances or extraoral appliances such as facemasks may be suitable alternatives to MIs for adolescents. Females usually reach full physical development by 15-17 years of age, whereas males typically complete puberty by 18-19 years of age.37 If the data in the previously published articles had been categorized using these peaks of physical growth, the results might have shown remarkable differences between the success rates of MIs inserted in patients with a different age dichotomization.
Miniscrew implant length and diameter
The most common MI lengths in the buccal area are 6 mm and 8 mm. Based on the study by Crismani et al.,30 which recommended that lengths under 8 mm be avoided, the present meta-analysis divided MIs into lengths of < 8 mm or ≥ 8 mm. As for diameter, ≤ 1.4 mm vs. > 1.4 mm was selected because the common diameters in the buccal region are 1.4 mm and 1.6 mm, and because Crismani et al.30 recommended that miniscrew diameters under 1.2 mm should be avoided, while Kuroda et al.38 recommended that miniscrew diameters of 1.3 mm and over be used. Even when the criteria of diameter is changed to ≤ 1.2 mm vs. > 1.2 mm or ≤ 1.3 mm vs. > 1.3 mm, larger diameter MIs still show a higher success rate than smaller MIs. It should be noted that although significant differences in the success rates were found between the groups up to 1.4 mm, for the group of ≤ 1.5 mm vs. > 1.5 mm, no significant differences in the succes rates were observed. This result supports the results reported that smaller diameter MIs should be avoided by Crismani et al.30 and Kuroda et al.38 Since miniscrew retention depends on its mechanical interdigitation to the bone, the physical length and diameter of the screw plays an essential role in its placement. Compared to longer and larger screws, shorter and smaller screws have less mechanical interdigitation and can easily break during implantation. Thus, it is important to select an appropriate size when placing miniscrews in the interradicular space to provide orthodontic anchorage, and it is also essential to prevent the screw from being too close to the roots.38 In terms of clinical applications, the results of the present meta-analysis indicating the success rate of each type of screw (length/diameter) and the region where MIs are most successful (maxilla/mandible) can help reduce the failure rate of MIs.
Some of the limitations in the present meta-analysis are as follows: (1) The exclusion of LOE articles may contribute to a risk of publication bias; however, the publication bias could be reduced by using the trim-and-fill method. (2) Despite an exhaustive search of the literature, the number of identified studies satisfying the inclusion criteria was low. Among them, only 5 prospective studies were found, and the number of prospective study in a subgroup was only one (Table 3). With one prospective study, a meta-analysis could not be performed.
More prospective study, including randomized controlled trials, will be needed to make firm conclusions, and authors should choose appropriate studies since inconsistent success rates imposed by particular areas may contribute to the heterogeneity.
CONCLUSION
The success rates of MIs inserted in the maxilla were higher than the rates of MIs inserted in the mandible. Compared to retrospective studies, prospective studies showed higher success rates for MIs inserted in the maxilla. Significantly higher MI success rates were found in patients who were ≥ 20 years of age. Significantly higher success rates were also identified when long MIs (≥ 8 mm) and large diameter MIs (> 1.4 mm) were used. No significant differences were found between the success rates of MIs inserted in males and females. When a treatment plan is made, these risk factors, i.e. jaw of insertion, age, MI length, and MI diameter, should be taken into account, while sex is not critical to the success of MIs.
ACKNOWLEDGEMENTS
This research was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF), funded by the Ministry of Education (2011-0012875).
Appendix 1
Search strategy for the electronic databases used in this meta-analysis
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 2.Moon CH, Lee DG, Lee HS, Im JS, Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 3.Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109–114. doi: 10.1111/j.1600-0501.2005.01211.x. [DOI] [PubMed] [Google Scholar]
- 4.Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 5.Choi JH, Park CH, Yi SW, Lim HJ, Hwang HS. Bone density measurement in interdental areas with simulated placement of orthodontic miniscrew implants. Am J Orthod Dentofacial Orthop. 2009;136:766.e1–766.e12. doi: 10.1016/j.ajodo.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 6.Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194–199. doi: 10.1016/j.ajodo.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Wu TY, Kuang SH, Wu CH. Factors associated with the stability of mini-implants for orthodontic anchorage: a study of 414 samples in Taiwan. J Oral Maxillofac Surg. 2009;67:1595–1599. doi: 10.1016/j.joms.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Viwattanatipa N, Thanakitcharu S, Uttraravichien A, Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2009;136:29–36. doi: 10.1016/j.ajodo.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Wiechmann D, Meyer U, Büchter A. Success rate of mini- and micro-implants used for orthodontic anchorage: a prospective clinical study. Clin Oral Implants Res. 2007;18:263–267. doi: 10.1111/j.1600-0501.2006.01325.x. [DOI] [PubMed] [Google Scholar]
- 11.Dalessandri D, Salgarello S, Dalessandri M, Lazzaroni E, Piancino M, Paganelli C, et al. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n > 50) Eur J Orthod. 2014;36:303–313. doi: 10.1093/ejo/cjt049. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28:138–144. doi: 10.1017/S0266462312000086. [DOI] [PubMed] [Google Scholar]
- 14.Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol. 2002;31:115–123. doi: 10.1093/ije/31.1.115. [DOI] [PubMed] [Google Scholar]
- 15.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100–106. [PubMed] [Google Scholar]
- 16.Chen YJ, Chang HH, Huang CY, Hung HC, Lai EH, Yao CC. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. [DOI] [PubMed] [Google Scholar]
- 17.Antoszewska J, Papadopoulos MA, Park HS, Ludwig B. Five-year experience with orthodontic miniscrew implants: a retrospective investigation of factors influencing success rates. Am J Orthod Dentofacial Orthop. 2009;136:158.e1–158.e10. discussion 158-9. doi: 10.1016/j.ajodo.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 18.Manni A, Cozzani M, Tamborrino F, De Rinaldis S, Menini A. Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eur J Orthod. 2011;33:388–395. doi: 10.1093/ejo/cjq090. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe H, Deguchi T, Hasegawa M, Ito M, Kim S, Takano-Yamamoto T. Orthodontic miniscrew failure rate and root proximity, insertion angle, bone contact length, and bone density. Orthod Craniofac Res. 2013;16:44–55. doi: 10.1111/ocr.12003. [DOI] [PubMed] [Google Scholar]
- 20.Topouzelis N, Tsaousoglou P. Clinical factors correlated with the success rate of miniscrews in orthodontic treatment. Int J Oral Sci. 2012;4:38–44. doi: 10.1038/ijos.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen CH, Chang CS, Hsieh CH, Tseng YC, Shen YS, Huang IY, et al. The use of microimplants in orthodontic anchorage. J Oral Maxillofac Surg. 2006;64:1209–1213. doi: 10.1016/j.joms.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 22.Tseng YC, Hsieh CH, Chen CH, Shen YS, Huang IY, Chen CM. The application of mini-implants for orthodontic anchorage. Int J Oral Maxillofac Surg. 2006;35:704–707. doi: 10.1016/j.ijom.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses [Internet] Ottawa (ON): Ottawa Health Research Institute; [accessed 2006 May 11]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 24.Cooper H, Hedges LV. The handbook of research synthesis. 1st ed. New York: Russell Sage Foundation Publications; 1994. p. 251. [Google Scholar]
- 25.Lim HJ. Meta-analysis in dental research. J Korean Dent Assoc. 2014;52:478–490. [Google Scholar]
- 26.Greenland S. Invited commentary: a critical look at some popular meta-analytic methods. Am J Epidemiol. 1994;140:290–296. doi: 10.1093/oxfordjournals.aje.a117248. [DOI] [PubMed] [Google Scholar]
- 27.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 28.Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20:641–654. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 29.Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop. 2012;142:577–595.e7. doi: 10.1016/j.ajodo.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 30.Crismani AG, Bertl MH, Celar AG, Bantleon HP, Burstone CJ. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop. 2010;137:108–113. doi: 10.1016/j.ajodo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 31.Lim JE, Lee SJ, Kim YJ, Lim WH, Chun YS. Comparison of cortical bone thickness and root proximity at maxillary and mandibular interradicular sites for orthodontic mini-implant placement. Orthod Craniofac Res. 2009;12:299–304. doi: 10.1111/j.1601-6343.2009.01465.x. [DOI] [PubMed] [Google Scholar]
- 32.Lim HJ, Choi YJ, Evans CA, Hwang HS. Predictors of initial stability of orthodontic miniscrew implants. Eur J Orthod. 2011;33:528–532. doi: 10.1093/ejo/cjq122. [DOI] [PubMed] [Google Scholar]
- 33.Lai TT, Chen MH. Factors affecting the clinical success of orthodontic anchorage: Experience with 266 temporary anchorage devices. J Dent Res. 2014;9:49–55. [Google Scholar]
- 34.Yi Lin S, Mimi Y, Ming Tak C, Kelvin Weng Chiong F, Hung Chew W. A study of success rate of miniscrew implants as temporary anchorage devices in singapore. Int J Dent. 2015;2015:294670. doi: 10.1155/2015/294670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paik CH, Park IK, Woo Y, Kim TW. Orthodontic miniscrew implant: Clinical applications. New York: Mosby; 2009. p. 258. [Google Scholar]
- 36.Lim HJ, Eun CS, Cho JH, Lee KH, Hwang HS. Factors associated with initial stability of miniscrews for orthodontic treatment. Am J Orthod Dentofacial Orthop. 2009;136:236–242. doi: 10.1016/j.ajodo.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 37.Susanne C, Guidotti A, Hauspie R. Age changes of skull dimensions. Anthropol Anz. 1985;43:31–36. [PubMed] [Google Scholar]
- 38.Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung HM, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131(4 Suppl):S68–S73. doi: 10.1016/j.ajodo.2006.06.017. [DOI] [PubMed] [Google Scholar]