Abstract
Objective
Secondhand smoke exposure (SHSe) poses risks to hospitalized children upon discharge and no uniformly effective interventions have been identified. Understanding change-related processes and social-contextual factors related to motivation for implementing home and car smoking bans may inform interventions to reduce infant SHSe among mothers with a hospitalized infant.
Methods
In this cross-sectional, secondary analysis, mothers of neonatal ICU infants who reported smoking or living with a smoker (N=205) were assigned to stages of change (pre-contemplation, contemplation, preparation, or action) based on behaviors and intentions for establishing smoking bans in their homes and cars. Processes of change (POC) for SHSe reduction practices, self-efficacy, depressive symptoms, generalized anxiety, and social support for not smoking in the home were examined across all four stages.
Results
The majority of mothers were in the action stage for having a home smoking ban in place (55%); only 35% of participants were in action for a car smoking ban. POC use differed across the stages of change for having a home ban (p=0.004) and car ban (p=0.02), with earlier stages using fewer overall and relatively fewer cognitive/affective processes. Earlier stage women also reported lower self-efficacy to change, less familial and partner support for in-home smoking bans, and more depressive symptoms.
Conclusions
Novel intervention targets were identified, including cognitive/affective change processes, mental health, and familial/social contingencies for implementing SHSe protective practices. Creative ways in which to affect change at the individual and household level are needed in order to fully address the complexity of child SHSe.
Keywords: Secondhand smoke, infant, home smoking ban, car smoking ban, stages of change
Secondhand smoke exposure (SHSe) is a significant public health problem. Recent survey data suggest the significant downward trend in secondhand smoke exposure seen between 1988 and 2002 has leveled off and that significant disparities persist (Chen, Burton et al. 2010). Infants and young children are commonly exposed to secondhand smoke in their homes, increasing risk for sudden infant death syndrome, acute respiratory infections, ear problems, and asthma (USDHHS 2007).
Acute illness or hospitalization of a child provides an ideal opportunity to intervene with parents on eliminating SHSe in their homes and cars, particularly for children suffering from respiratory-related conditions (Winickoff, Hibberd et al. 2001). Infants hospitalized after birth in a neonatal intensive care unit (NICU) are often born premature, at low birthweight, and typically have diminished respiratory function; and the smoking rate is high in this low-income, minority population (Stotts, Evans et al. 2011, Stotts, Green et al. 2013). Families with a medically at-risk child would benefit from a home smoking ban (Wakefield, Banham et al. 2000, Gehrman and Hovell 2003, Pizacani, Martin et al. 2003), yet implementation is often a challenge. Interventions targeting households with smokers from NICU and similar populations have been tested with varying levels of success (Stotts, Green et al. 2013, Rosen, Myers et al. 2014, Blaakman, Borrelli et al. 2015, Chi, Wu et al. 2015, Northrup, Matt et al. 2015), and, to the best of our knowledge, no SHSe intervention has been designated as evidence-based (Priest, Roseby et al. 2008). Little is known about the process of change for reducing SHSe in general or about individual- OR social-contextual factors that may help or hinder new mothers in the adoption of home and car smoking bans.
Understanding and examining the process of change for smoking cessation has been a central focus of the Transtheoretical Model (Prochaska and DiClemente 1983, Prochaska, Velicer et al. 1991), and more recently the model has been used as a framework for SHSe interventions (Kegler, Escoffery et al. 2012, Huang, Wu et al. 2013). The stages and process of change are two interrelated dimensions used to understand intentional behavior change. The stages of change (precontemplation, contemplation, preparation, action, maintenance) represent the temporal, motivational aspects of change and the processes of change are overt and covert activities individuals engage in when they attempt to modify problem behaviors (Norcross, Krebs et al. 2011). The processes of change were identified as common across over 400+ psychotherapies (Prochaska and DiClemente 1983, Prochaska and DiClemente 1985). Experiential processes (i.e., cognitive and affective experiences/activities) help increase awareness of the advantages of changing and/or the negative consequences and regret/guilt associated with not changing, which tend to increase motivation for change. Behavioral processes (i.e., action-oriented, behavioral activities) involve strategies like counterconditioning or response substitution, identifying helping relationships, and reinforcement management to support and sustain active change.
Processes of change have been found to be differentially effective in certain stages of change. Experiential processes tend to peak in the contemplation or preparation stages while behavioral processes are used most in the action and maintenance stages, and this interaction has been related to outcome (Rosen 2000). Engaging in more experiential than behavioral processes during the contemplation and preparation stages and relatively more behavioral than experiential processes during the action stage was predictive of more successful behavior change (Perz, DiClemente et al. 1996).
Motivation for change does not exist in a vacuum, of course, and is undoubtedly influenced by other individual and social-contextual factors (Hovell and Hughes 2009). For example, we found that women who quit smoking during pregnancy used fewer experiential and behavioral processes of change compared to women who quit outside of pregnancy (Stotts, DiClemente et al. 1996). Pregnant quitters essentially failed to engage in the decision-making and other experiential processes, and yet were able to suspend their smoking during pregnancy. This may, in part, explain the typically poor long-term outcomes for pregnant quitters after giving birth (i.e., postpartum relapse; (Colman and Joyce 2003, Fang, Goldstein et al. 2004)). Decision-making and other processes used in changing smoking ban policies may be similarly altered by having a hospitalized infant, underscoring the importance of context in the change process.
Additional contextual factors potentially important for new mothers include mental health and social contingencies, which may affect motivation to implement a home or car smoking ban or other protective practices. Postpartum depressive symptoms are not uncommon among new mothers and may be even more pronounced among mothers with a high-risk infant (Northrup, Evans et al. 2013). Depressive symptoms are associated with poor outcomes for smoking cessation and other behavioral changes (MacPherson, Tull et al. 2010). Social contingencies (e.g., praise from a friend) are reflected in the Transtheoretical Model’s behavioral processes of change (e.g., reinforcement management, helping relationships) and have received increased attention in recent years (Hovell and Hughes 2009, Zhang, Cowling et al. 2010). Social reinforcement or punishment for indoor smoking may especially influence motivation to change home and car smoking policies in new mothers, particularly mothers of low SES who tend to reside in households with multiple family members or friends. Families have been found to be influential in normalizing smoking behaviors and practices (Weden and Miles 2012, Vuolo and Staff 2013). Smoking encouragement and discouragement by family members has also been identified as an important contributor to smoking status (Hofstetter, Hovell et al. 2010). Despite bringing home from the hospital an infant at high respiratory risk, NICU mothers may be unduly influenced by other household members when considering a home and car smoking ban.
This secondary data analysis was the first study to examine the use of the processes of change across the stages of change for implementing home and car smoking bans among mothers with a hospitalized infant. Relations between stage of change and postpartum depression symptoms and social encouragement/discouragement for smoking in the home were also explored. The overarching goal was to better understand and characterize the process of change involved in establishing a smoke-free home for new mothers with physically vulnerable infants to identify new and/or more precise intervention targets. It was hypothesized that NICU mothers may be engaging in lower levels of experiential relative to behavioral processes of change for establishing home and car smoking bans, which has been indicative of less success in making or sustaining behavior change (Perz, DiClemente et al. 1996). It was also expected that NICU mothers who smoked themselves, lived with more than one smoker, were encouraged by others to smoke indoors, or did not have a residence of her own would be less likely to have a home smoking ban in place compared to women who did not smoke or who lived with only one smoker.
Methods
Participants
Participants (N = 205) were recruited as part of an ongoing, NICU-based, SHSe intervention study (Baby’s Breath II; (Stotts, Northrup et al. 2013)), registered on clinicaltrials.gov (NCT01726062). Between September 2012, and April, 2015, mothers of infants admitted to the NICU of a large children’s hospital in Houston, TX, were recruited. Eligible participants: (1) had an infant in the NICU; (2) reported ≥1 smoker living in the household; and (3) lived within a 50-mile radius of the hospital (follow-up assessments were conducted in the home).
Study Design and Procedures
The parent study employs a randomized-controlled, parallel-group design; only baseline data were used in this study. Research assistants (RAs) approached caregivers in the NICU to screen for eligibility. All participants provided written informed consent in compliance with our institutional IRB. At the baseline visit, while the infant was hospitalized in the NICU, RAs administered a structured interview and participants completed a self-paced computerized questionnaire. Following baseline, participants were randomized to conventional NICU care or a Motivational Interviewing intervention targeting the prevention of infant SHSe after discharge.
Measures
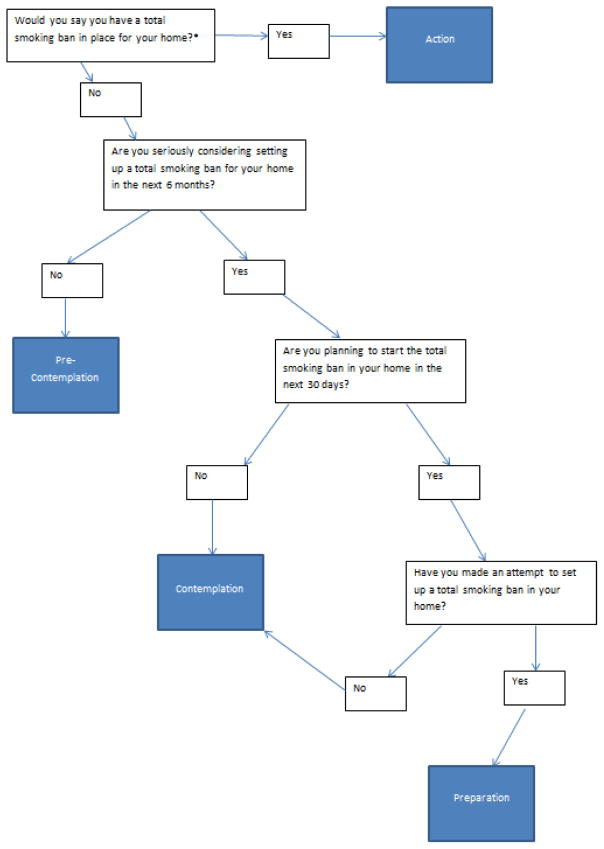
The baseline interview included demographic, smoking-related, and psychosocial measures. In-home and in-car smoking ban statuses were assessed separately with a multiple-choice question and two confirmation questions (Mullen, Carbonari et al. 1991, Stotts, Green et al. 2013). Stage of change (SOC) classifications were assigned according to participant responses to four staging questions adapted from the stages of change algorithm for smoking ((DiClemente, Prochaska et al. 1991); see Figure 1). Participants were assigned to pre-contemplation, contemplation, preparation, or action/maintenance groups, separately for home and for car smoking bans. All women who reported currently having a smoking ban in place were classified in the action stage, as a meaningful timeframe for separating action from maintenance for this behavior has not been established.
Figure 1.
Stage of Change Classification Flowchart.
The Processes of Change (POC) scale (Prochaska, Velicer et al. 1988, Cancer Prevention Resource Center 2011) is a 10-item self-report measure, adapted to secondhand smoke, that assesses experiential (cognitive/affective) and behavioral change processes (Cronbach’s alpha = .88). Participants reported the frequency with which they engaged in various cognitive or behavioral activities related to protecting their infant from SHSe in the last month on a 5-point Likert scale. The experiential subscale focused on thoughts and feelings related to SHSe (e.g., “It worries me when I think of how my family may be affected by secondhand smoke”). The behavioral subscale focused on actions taken related to reducing SHSe (e.g., “I look for people who will support and care about me in my attempt to keep my baby from secondhand smoke.”). Higher mean scores on POC questions indicate higher engagement in the change processes.
Self-efficacy for enforcing a home and car smoking ban was assessed using an adaptation of the Smoking Abstinence Self-efficacy scale (Diclemente, Prochaska et al. 1985). This 14-item scale asks participants to rate their level of confidence for avoiding SHSe in different situations, such as “when it is raining outside” or “when others are smoking,” on a 5-point Likert scale. Higher scores indicate higher confidence for adhering to a smoking ban (Cronbach’s alpha = .97).
The Center for Epidemiological Studies-Depression Scale (CES-D; Radloff 1977) is a 20-item, self-report scale used to assess depression symptoms in community populations, and has been identified as a valid instrument in similar populations (Vigod, Villegas et al. 2010). In our sample the Cronbach’s alpha was .87. A score of 16 or higher was found in initial studies (e.g., Radloff 1977) to indicate depressive illness and continues to be a valid and widely used criterion (Rush 2000, Vigod, Villegas et al. 2010, McManus and Poehlmann 2011, Northrup, Evans et al. 2013).
A social support for not smoking in the home and car scale was adapted from the social support for non-smoking scale (Hofstetter, Hovell et al. 2010). Participants were asked to report whether 12 different groups of people in their lives (partner, mother, father, siblings, other children, grandparents, aunt(s), uncle(s), friends, co-workers, healthcare providers, or any others) “encouraged” (value = +1), “discouraged” (value = −1), or “neither encouraged nor discouraged” (value=0) smoking in the home and car. A composite encouragement value was created by adding the reported value for each group together and dividing by 12. For non-existent relationships, a value of 0/zero was imputed per scoring instructions (Hofstetter, Hovell et al. 2010). A higher score indicated more encouragement for smoking in the home and car. Additionally, relationship-level aggregates were created and explored for the participants’ partner (1 item), parents (2 items), other family (6 items), and friends/coworkers (2 items) by adding the reported values together and dividing by the total number of people in the group.
Statistical analyses
Chi-square tests were used to compare participant characteristics (race, SES) among stages of change groups. ANOVAs were used to compare means of experiential POC, behavioral POC, self-efficacy for adhering to a smoking ban, social support (encouragement for indoor smoking), and CES-D scores across stages of change. Further, post-hoc, pairwise comparisons were made with Tukey’s procedure. Multinomial logistic regression was used to examine the effect of social support for smoking in the home and car by stages of change group. All statistical analyses were conducted in SAS 9.4 (Cary, NC).
Results
Household and smoking characteristics
Results showed that 22% of mothers and 80% of their partners were smokers. Forty-three percent of participants also reported additional household smokers. The mean number of cigarettes smoked per day by all household residents was 12.9. The mean age of participants in the study was 26 years, and the majority of participants were African American. Over half of participants had three or more children living in the home and over a third lived with extended family or friends/others. The average size of the household was nearly 6 people, with a range of 2–18. Medicaid was the insurance used by a large majority of the women and their children (See Table 1).
Table 1.
Descriptive Characteristics of Study Sample (N=205)
| Variable | N (%) | M (SD) |
|---|---|---|
| Participant Smoking | 46 (22) | |
| Partner Smoking | 138 (80) | |
| Other Smokers Living in Household | 89 (43) | |
| Race/Ethnicity | ||
| Hispanic | 43 (21) | |
| White | 23 (11) | |
| Black | 133 (65) | |
| Other | 6 (3) | |
| Number of Children in Home | ||
| One | 48 (23) | |
| Two | 50 (24) | |
| Three or More | 107 (53) | |
| Annual Household Income | ||
| <$25,000 | 127 (66) | |
| >=$25,000 | 66 (34) | |
| Highest Education Level | ||
| <= High School | 125 (61) | |
| > High School | 80 (39) | |
| Current Living Situation | ||
| With Partner or Alone | 131 (64) | |
| With Parents/Extended Family/Friends/Other | 74 (36) | |
| Medicaid Recipient | 183 (89) | |
| Breastfeeding Status | ||
| No, Never | 50 (24) | |
| Yes, Currently | 135 (66) | |
| Did for a While, then Stopped | 20 (9) | |
| Not Employed | 164 (80) | |
| Relationship Status | ||
| Married or Living with Partner | 119 (58) | |
| Single/Divorced/Separated | 86 (42) | |
| GAD-7 Score | 6.5 (5.8) | |
| CES-D Score | 17.2 (11.9) | |
| Encouragement Score | 0.09 (0.44) | |
| Age | 26 (5.8 | |
| # People in the Household | 5.6 (2.0) | |
| # Smokers in the Household | 2.5 (0.83) | |
| Total Cigarettes per Day (all Household Smokers) | 12.9 (14.4) | |
| Infant Birthweight in Grams | 2180 (938) | |
Home and car smoking bans by stage of change
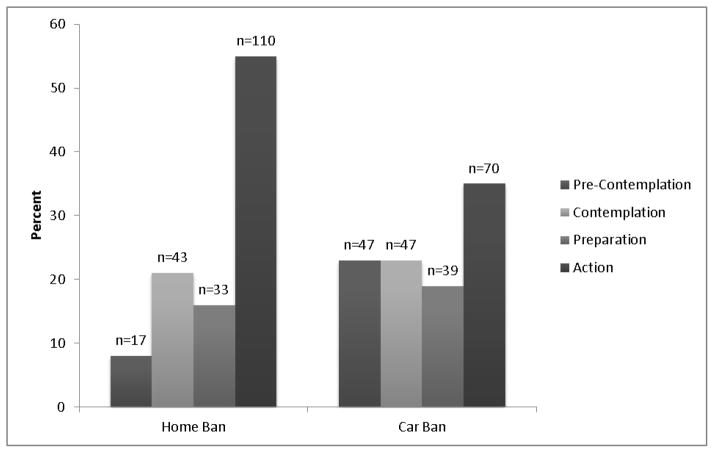
About half of NICU mothers (55%) were classified in the action stage of change for implementing a home smoking ban, and 8% were in the precontemplation stage or not currently thinking about implementing a home smoking ban. However, only 35% of women were in the action stage, while 23% were in precontemplation for having a car smoking ban (see Figure 2).
Figure 2.
Percentage of participants in each stage of change for home smoking and car smoking bans.
Household and smoking characteristics by stage of change
Participants in the four stages of change differed on a few characteristics. First, with regard to home smoking bans, a higher number of women who self-identified as Hispanic were in the action stage of change relative to Non-Hispanic Blacks or Whites, (χ2 [N = 197] = 20.7, p = .01). Also, the number of cigarettes smoked per day by all household members differed significantly by stage of change (F [3,199] = 11.2, p = .0001); women in the action stage reported fewer cigarettes smoked per day by all household members (M=8.2, SD=8.9) relative to women in the contemplation (M=21.7, SD=19.3) and preparation (M=16.0, SD=15.5; p<0.05) stages. The proportion of mothers who smoked was not different across stage of change (χ2(N=205)=5.3, p=0.15).
Regarding car smoking bans, stage differences were found only for the participant’s current living situation. Women who had their own place of residence, either alone or with their partner, were more likely to be in the action stage of change for a car smoking ban compared to those living with friends or relatives, (X2 [N =198] = 11.8, p = .008).
Processes of change by stage for home and car smoking bans
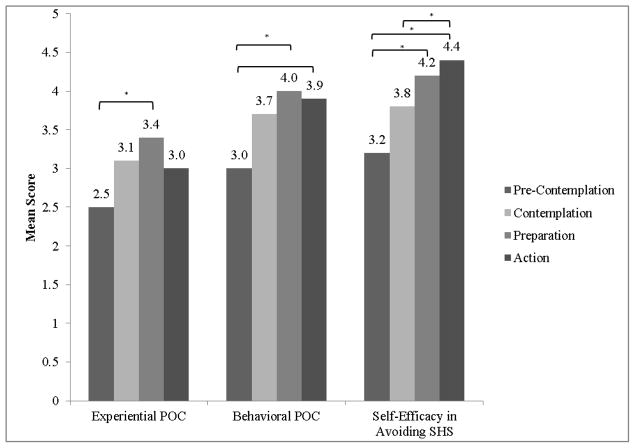
Experiential (F(3,197) = 3.56, p=0.02) and behavioral (F(3,197) = 4.22, p=0.006) processes of change scores differed across the stages of change for instituting a home smoking ban. With regard to experiential processes, women in the preparation stage were engaging in the highest level of experiential processes (M=3.4, SD=0.94) and were significantly higher compared to pre-contemplation women, (M=2.4, SD=1.1; p<0.05). Women in preparation (M=4.0, SD=0.92) and action (M=3.9, SD=1.0) for a home ban were using higher levels of behavioral processes compared to precontemplators, (M=3.0, SD=1.2; p<0.05). Notably, within each stage, use of behavioral processes is higher than experiential process use, even in the earlier stages of change (See Figure 3).
Figure 3.
Mean processes of change and self-efficacy scores by home ban stage of change
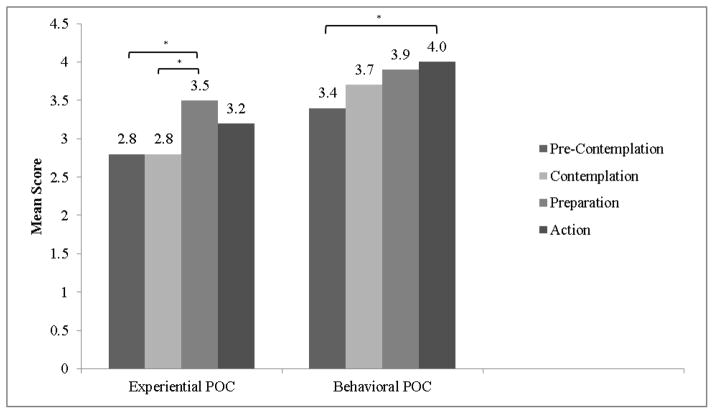
Regarding a car smoking ban, mean behavioral (F(3,197)=3.19, p=0.02) and experiential (F(3,197)=5.12, p=0.002) POC scores also varied by stage of change. Women in preparation were engaging in experiential processes at higher levels (M=3.5, SD=0.92) compared to both contemplation (M=2.8, SD=0.84) and pre-contemplation women (M=2.8, SD=0.93; p<0.05). Women in the action stage for implementing a car smoking ban were reporting higher levels of behavioral processes (M=4.0, SD=1.1) relative to the pre-contemplation group (M=3.4, SD=0.96; p<0.05; see Figure 4). Similar to findings for home bans, behavioral processes were being reported at higher levels relative to experiential processes in all 4 stages.
Figure 4.
Mean processes of change scores by car ban stage of change.
Self-efficacy for enforcing a home and car smoking ban
Confidence for enforcing a home smoking ban differed significantly by stage of change (F(3,196)=11.01, p<0.0001). Self-efficacy was significantly lower among women in the pre-contemplation stage for implementing a home smoking ban (M=4.0, SD=0.97) compared to preparation (M=4.2, SD=0.71) and action stage women (M=4.2, SD=0.98; p<0.05). Contemplation stage women were also lower in confidence (M=3.9, SD=0.99) compared to the action group (p<0.05; see Figure 3). Self-efficacy for enforcing a car smoking ban did not differ by stage of change (F(3,196)=0.69, p=0.56).
Depressive Symptoms (CES-D) by stage of change
CES-D scores differed across the stages of change for implementing a home smoking ban (F(3,197)=4.72, p=0.003). Specifically, less motivated women in the contemplation group reported significantly more depressive symptoms (M=23.0, SD=13.0) compared to women in the action group (M=15.3, SD =11.7; p<0.05)). No differences were found on CES-D scores across the stages of change for implementing a car smoking ban, (F(3,197) = 0.14, p=0.9).
Social support for not smoking in the home and car
The mean composite social support score was 0.09 (SD = 0.44), indicating a slight tendency for the social networks of our participants to encourage (vs. discourage) smoking in the home and car. The mean social support scores varied significantly across stages of change for both home ban (F(3,198)=5.53, p=0.001) and car ban (F(3,198)=6.41, p=0.0004). For home bans, women in action reported higher levels of discouragement from their family and friends (M =−0.01, SD =0.43) for smoking in their home and car than women in the precontemplation group (M=0.27, SD=0.48; p<0.05). Regarding a car ban, action stage women reported more people in their social networks discouraged smoking in the car (M=−0.08, SD=0.46) than women in precontemplation (M=0.23, SD=0.40; p<0.05), contemplation (M=0.19, SD=0.38; p<0.05), and preparation (M=0.15, SD=0.40; p<0.05).
Stage differences were also found when larger relationship-level categories were examined (partner, parents, other family members, friends/coworkers). For home smoking bans, the odds of having a partner discourage smoking in the home and car were 2.5 times higher for the action group compared to the precontemplation group (p=0.03; 95% CI [1.1–5.7]); and 1.5 times higher for the action group compared to the contemplation group (p0.049 95% CI [1.1–2.4]). The odds of the participants’ parents discouraging smoking in the home and car was 3.1 times higher in the action group compared to the precontemplation group (p=.006; 95% CI [1.4–7.1]); 2.2 times higher in the action group compared to the contemplation group (p=0.005; 95% CI [1.3–4.0]); and 1.9 times higher in the action group as compared to the preparation group (p=0.03; % CI [1.1–3.6]). The odds of other family members discouraging smoking in the home and car and was 5 times higher in the action group compared to the precontemplation group (p=.04; 95% CI [1.1–23.1]).
Similarly, with regard to a car smoking ban, women in action reported more discouragement of smoking from partners relative to each of the pre-contemplation (p=0.0003; OR = 2.4, 95% CI [1.5–3.8]), contemplation (p=0.001; OR = 2.1, 95% CI [1.4–3.3]), and preparation groups p<0.0001; OR = 2.7, 95% CI [1.6–4.4]). Participants’ parents were also more discouraging of smoking in the home and car in the action group compared to parents of women in precontemplation and contemplation, (p=0.004; OR = 2.6, 95% CI [1.4–4.9]), (p=0.002; OR = 2.6, 95% CI [1.4–4.7]), respectively. Finally, other family members of women in action were more discouraging of smoking in the home and car compared to the precontemplation group, (p=0.003; OR = 6.2, 95% CI [1.9–20.7]). There was no relationship between stage of change and discouragement of smoking in the home and car by mother’s friends, co-workers, or health professionals.
Discussion
Nearly two-thirds of the hospitalized children in this sample were discharged to a household where at least one person smokes inside the home or car, exposing them to SHS and its harmful effects. Home and car smoking bans reduce risks from SHSe and are especially important for medically at-risk children with compromised respiratory systems. This study was the first to explore motivation for change in a population of disadvantaged families with a hospitalized, NICU infant. The primary goal was to better understand and to generate hypotheses regarding the use of common change processes, as well as relevant individual- and social-contextual factors, with the ultimate goal to inform intervention. Overall, about half of mothers of hospitalized NICU infants reported being in the action stage for having a home smoking ban; however, only 34% were in action for restricting smoking in the car. Meaningful differences on processes of change, depression, self-efficacy and social support were found among women with varying motivation, providing important avenues for intervention.
Mothers’ engagement in the processes of change differed among the stages for instituting both home and car bans. As is typical, precontemplators were using both experiential and behavioral processes at the lowest levels relative to women in the other stages, particularly preparation and action. Relative use of the experiential and behavioral processes in the various stages of change was also notable. Women in the later stages (preparation and action) were using more behavioral than experiential processes, which is appropriate and indicative of success (Prochaska, Velicer et al. 1988). However, as hypothesized, less motivated mothers in the earlier stages of change were also using behavioral processes at higher rates relative to experiential processes and were less confident in their ability to implement a home smoking ban; a pattern previously associated with the inability to achieve or sustain change (Perz, DiClemente et al. 1996, Stotts, DiClemente et al. 1996).
Context is important in interpreting these findings. Mothers in this study had recently given birth to premature, low birth weight or otherwise medically at-risk infants admitted to a NICU. Thus, most mothers are interested, if not concerned, about the impact of SHSe on their infant upon discharge. Even women in the early stages of change who state they are unready to institute a smoking ban reported some behavioral activities toward change. Unfortunately, earlier stage women reported less use of the cognitive and affective processes important for successfully progressing to the later stages and eventual change (Perz, DiClemente et al. 1996, Rosen 2000). For NICU mothers, similar to women who suspend smoking upon learning of their pregnancy (Stotts, DiClemente et al. 1996, Stotts, DiClemente et al. 2000), their infants’ medical issues likely negate thoughtful consideration about the benefits and challenges of change which typically lead to the decision to implement a home or car smoking ban. Early processes that raise consciousness of the problem or explore thoughts and feelings about SHSe and change seem unnecessary, or perhaps frightening, in light of the overwhelming concern about the infants’ health. Without engaging in these early processes, however, it is challenging to initiate and/or sustain change. Sustaining SHSe restrictions has been noted as a challenge in similar intervention studies (Blaakman, Borrelli et al. 2015). In order to promote successful change mothers and other household members may need to thoroughly explore and understand the effects of SHSe on their vulnerable infant as well as what it will mean for them to change household smoking policies. Also, a focus on other more global benefits for everyone in the home, as well as the baby, may assist in making and sustaining a decision to change (Mullen 2004). Motivational Interviewing and TTM-based interventions addressing similar issues have been found at least partially effective in preventing passive smoke exposure among pregnant women and mothers of small children in previous studies (Huang, Wu et al. 2013, Eakin, Rand et al. 2014)
Additional contextual factors were also associated with motivation for implementing an indoor and car smoking ban, confirming several of our hypotheses. Specifically, mothers with a hospitalized infant who: (1) did not have their own place of residence; (2) reported larger amounts of smoking among household members; and 3) reported more encouragement for smoking in the home and car tended to be in earlier stages of change for smoking bans. From these findings it is clear that the social environment in which a mother resides is related to her motivation and likely her ability to affect change. This may be especially salient for low-income women who often reside with multiple family members and friends to share housing and transportation costs (Dominguez and Watkins 2003). SHSe intervention studies have targeted mothers or mothers and partners alone (Stotts, Green et al. 2013, Winickoff, Nabi-Burza et al. 2013, Rosen, Myers et al. 2014), but this may be inadequate. Ideally, all family members and caretakers of the child would be involved in the intervention in order to reduce SHSe not only in the home but also in other environments in which the child visits (Eakin, Rand et al. 2014). As discussed in other studies targeting SHSe, interventions must address complex familial and social relationships and contingencies in order to improve upon effectiveness (Hovell and Hughes 2009, Eakin, Rand et al. 2014).
Individual characteristics, namely the smoking status of the mother and her depression symptoms, were also hypothesized to differ by stage of change. Surprisingly, mothers’ smoking status was not associated with stage of change for establishing a home smoking ban. This is contrary to previous literature indicating that mothers who smoke are less likely to have home smoking bans (e.g., Gonzales, Malcoe et al. 2006), and therefore should be interpreted with caution. However, the context, i.e., having an infant in the NICU, may have functioned to diminish this relationship such that mothers who smoke were just as likely to be motivated to protect their infants as mothers who did not. Depressive symptomatology, however, may significantly impact motivation to implement smoking bans as mothers who reported more depression were in the earlier, less motivated stages of change. Maternal depression has previously been reported as influential on maternal behaviors associated with child health (Leiferman 2002) and warrants further study in the context of SHS protective behaviors among postpartum mothers.
This exploratory study was an initial hypothesis-generating attempt to characterize motivation for changing household SHSe practices and the associated processes and contextual influences among mothers with a health-compromised child, in order to glean more precise intervention targets. There are limitations to the methods that need to be considered. The data are cross-sectional in nature and therefore conclusions regarding change over time cannot be made. The findings of this study may not be generalizable to all NICUs, as the study population was predominately African American and low SES, likely reflective of other large, urban NICUs. The precontemplation group for home bans was relatively small and therefore estimates of effects may be unstable. The low number of precontemplation participants is likely a result of having recently given birth to medically at-risk infants, which may lead to a sudden, externally driven increase in motivation to change behavior. A 10-item processes of change measure was used precluding separate analyses of the 10 individual processes of change (Prochaska, Velicer et al. 1988). Single measures are used for each construct (e.g., depression). With these caveats in mind, results provide novel intervention targets and hypotheses to be pursued in subsequent studies. Specifically, further study of motivation and change processes over time, particularly processes related to a new mother’s social and familial context, is clearly needed.
SHSe among children has both short and long-term detrimental consequences. Emerging data suggest that effective interventions need to have multiple components that address individual-level practices as well as social/familial influences. Creative ways in which to affect change at the household or family level are needed in order to fully address the complex problem of SHSe in homes.
Highlights.
NICU mothers were in different stages of change for establishing a home smoking ban.
Fewer NICU mothers were in action for a smoking ban in their car vs. home.
Early stage women were not sufficiently using cognitive-affective change processes.
Family encouragement of indoor smoking was associated with early stages of change.
Reducing child secondhand smoke exposure requires intervention at multiple levels.
Acknowledgments
1. Role of Funding Source
This study was supported by grant R01 HL107404 through the U.S. National Institute on Health, National Heart, Lung, and Blood Institute.
Authors would like to acknowledge the physicians and staff of the Children’s Memorial Hermann Hospital neonatal intensive care unit who assisted in the conduct of the parent study.
Footnotes
2. Contributors
Angela Stotts wrote the first draft of the manuscript. Michelle Klawans and Thomas Northrup conducted the statistical analyses and wrote the results section. Yolanda Villarreal and Melbourne Hovell edited multiple drafts of the paper. All authors contributed to and have approved the final manuscript.
3. Conflict of Interest
All authors declare they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Angela L. Stotts,
Michelle R. Klawans,
Thomas F. Northrup,
Yolanda Villarreal,
Melbourne F. Hovell,
References
- Blaakman SW, Borrelli B, et al. Secondhand Smoke Exposure Reduction After NICU Discharge: Results of a Randomized Trial. Academic pediatrics. 2015 doi: 10.1016/j.acap.2015.05.001. [DOI] [PubMed] [Google Scholar]
- Cancer Prevention Resource Center. Smoking: Processes of Change (Short Form) 2011 from http://www.uri.edu/research/cprc/Measures/Smoking01.htm.
- Chen CI, Burton T, et al. Recent trends in exposure to secondhand smoke in the United States population. BMC Public Health. 2010;10(1):359. doi: 10.1186/1471-2458-10-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi YC, Wu CL, et al. Randomized trial of a secondhand smoke exposure reduction intervention among hospital-based pregnant women. Addictive Behaviors. 2015;41:117–123. doi: 10.1016/j.addbeh.2014.10.001. [DOI] [PubMed] [Google Scholar]
- Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. American Journal of Preventive Medicine. 2003;24(1):29–35. doi: 10.1016/s0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, et al. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991;59(2):295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Diclemente CC, Prochaska JO, et al. Self-efficacy and the stages of self-change of smoking. Cognitive Therapy and Research. 1985;9(2):181–200. [Google Scholar]
- Dominguez S, Watkins C. Creating networks for survival and mobility: Social capital among African-American and Latin-American low-income mothers. Social problems. 2003;50(1):111–135. [Google Scholar]
- Eakin MN, Rand CS, Borrelli B, Bilderback A, Hovell M, Riekert KA. Effectiveness of motivational interviewing to reduce head start children’s secondhand smoke exposure. A randomized clinical trial. American journal of respiratory and critical care medicine. 2014;189(12):1530–1537. doi: 10.1164/rccm.201404-0618OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang WL, Goldstein AO, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. The Journal of the American Board of Family Practice. 2004;17(4):264–275. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- Gehrman CA, Hovell MF. Protecting children from environmental tobacco smoke (ETS) exposure: A critical review. Nicotine Tob Res. 2003;5(3):289–301. doi: 10.1080/1462220031000094231. [DOI] [PubMed] [Google Scholar]
- Gonzales M, Malcoe HL, Kegler MC, Espinoza J. Prevalence and predictors of home and automobile smoking bans and child environmental tobacco smoke exposure: a cross-sectional study of US-and Mexico-born Hispanic women with young children. BMC Public Health. 2006;6(1):1. doi: 10.1186/1471-2458-6-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter CR, Hovell MF, et al. It’s others, not the police: smoking, reprimand, and fines among adults of Korean descent in California. Health Psychology. 2010;29(3):255. doi: 10.1037/a0018166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovell MF, Hughes SC. The behavioral ecology of secondhand smoke exposure: A pathway to complete tobacco control. Nicotine Tob Res. 2009;11(11):1254–1264. doi: 10.1093/ntr/ntp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C-M, Wu H-L, et al. Transtheoretical model-based passive smoking prevention programme among pregnant women and mothers of young children. The European Journal of Public Health. 2013:cks177. doi: 10.1093/eurpub/cks177. [DOI] [PubMed] [Google Scholar]
- Kegler MC, Escoffery C, et al. Pilot study results from a brief intervention to create smoke-free homes. Journal of environmental and public health. 2012:2012. doi: 10.1155/2012/951426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiferman J. The effect of maternal depressive symptomatology on maternal behaviors associated with child health. Health Education & Behavior. 2002;29(5):596–607. doi: 10.1177/109019802237027. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, et al. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology. 2010;78(1):55. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus BM, Poehlmann J. Maternal depression and perceived social support as predictors of cognitive function trajectories during the first 3 years of life for preterm infants in Wisconsin. Child: Care, Health, and Development. doi: 10.1111/j.1365-2214.2011.01253.x. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen PD. How can more smoking suspension during pregnancy become lifelong abstinence? Lessons learned about predictors, interventions, and gaps in our accumulated knowledge. Nicotine & Tobacco Research. 2004;6(Suppl2):S217–S238. doi: 10.1080/14622200410001669150. [DOI] [PubMed] [Google Scholar]
- Mullen PD, Carbonari JP, et al. Improving disclosure of smoking by pregnant women. American journal of obstetrics and gynecology. 1991;165(2):409–413. doi: 10.1016/0002-9378(91)90105-z. [DOI] [PubMed] [Google Scholar]
- Norcross JC, Krebs PM, et al. Stages of change. Journal of Clinical Psychology. 2011;67(2):143–154. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- Northrup T, Evans PW, et al. Depression among mothers of high-risk infants in a neonatal intensive care unit. MCN: The American Journal of Maternal/Child Nursing. 2013;38(2):89–94. doi: 10.1097/NMC.0b013e318270f8b8. [DOI] [PubMed] [Google Scholar]
- Northrup TF, Matt GE, et al. Thirdhand smoke in the homes of medically fragile children: Assessing the impact of indoor smoking levels and smoking bans. Nicotine & Tobacco Research. 2015 doi: 10.1093/ntr/ntv174. epub: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perz CA, DiClemente CC, et al. Doing the right thing at the right time? The interaction of stages and processes of change in successful smoking cessation. Health Psychology. 1996;15:462–468. doi: 10.1037//0278-6133.15.6.462. [DOI] [PubMed] [Google Scholar]
- Pizacani BA, Martin DP, et al. Household smoking bans: which households have them and do they work? Preventive Medicine. 2003;36(1):99–107. doi: 10.1006/pmed.2002.1123. [DOI] [PubMed] [Google Scholar]
- Priest N, Roseby R, et al. Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. Cochrane Database Syst Rev. 2008;(4):CD001746. doi: 10.1002/14651858.CD001746.pub2. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Common processes of self-change in smoking, weight control, and psychological distress. In: Shiffman S, Wills TA, editors. Coping and substance use. Florida: Academic Press; 1985. pp. 319–343. [Google Scholar]
- Prochaska JO, Velicer WF, et al. Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol. 1988;56(4):520–528. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, et al. Patterns of change: dynamic typology applied to smoking cessation. Multivar Behav Res. 1991;26(1):83–107. doi: 10.1207/s15327906mbr2601_5. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosen CS. Is the sequencing of change processes by stage consistent across health problems? A meta-analysis. Health Psychology. 2000;19(6):593. [PubMed] [Google Scholar]
- Rosen LJ, Myers V, et al. Meta-analysis of parental protection of children from tobacco smoke exposure. Pediatrics: peds. 2014:2013–0958. doi: 10.1542/peds.2013-0958. [DOI] [PubMed] [Google Scholar]
- Rush A, et al. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Stotts A, Evans P, et al. Secondhand smoke risk in infants discharged from a NICU: Potential for significant health disparities? Nicotine and Tobacco Research. 2011;13(11):1015–1022. doi: 10.1093/ntr/ntr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stotts A, Green C, et al. Feasibility and efficacy of an intervention to reduce secondhand smoke exposure among infants discharged from a neonatal intensive care unit. Journal of Perinatology. 2013 doi: 10.1038/jp.2013.43. [DOI] [PubMed] [Google Scholar]
- Stotts AL, DiClemente CC, et al. Pregnancy smoking cessation: a case of mistaken identity. Addict Behav. 1996;21(4):459–471. doi: 10.1016/0306-4603(95)00082-8. [DOI] [PubMed] [Google Scholar]
- Stotts AL, DiClemente CC, et al. Postpartum return to smoking: Staging a suspended” behavior. Health Psychol. 2000;19(4):324–332. doi: 10.1037//0278-6133.19.4.324. [DOI] [PubMed] [Google Scholar]
- Stotts AL, Green C, et al. Feasibility and efficacy of an intervention to reduce secondhand smoke exposure among infants discharged from a neonatal intensive care unit. Journal of Perinatology. 2013;33(10):811–816. doi: 10.1038/jp.2013.43. [DOI] [PubMed] [Google Scholar]
- Stotts AL, Northrup TF, et al. Baby’s Breath II protocol development and design: A secondhand smoke exposure prevention program targeting infants discharged from a neonatal intensive care unit. Contemporary Clinical Trials. 2013;35(1):97–105. doi: 10.1016/j.cct.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHHS. Children and Secondhand Smoke Exposure: The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2007. [Google Scholar]
- Vigod SN, Villegas L, et al. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- Vuolo M, Staff J. Parent and child cigarette use: A longitudinal, multigenerational study. Pediatrics. 2013;132(3):e568–e577. doi: 10.1542/peds.2013-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield M, Banham D, et al. Restrictions on smoking at home and urinary cotinine levels among children with asthma. American Journal of Preventive Medicine. 2000;19(3):188–192. doi: 10.1016/s0749-3797(00)00197-5. [DOI] [PubMed] [Google Scholar]
- Weden MM, Miles JN. Intergenerational relationships between the smoking patterns of a population-representative sample of US mothers and the smoking trajectories of their children. American Journal of Public Health. 2012;102(4):723–731. doi: 10.2105/AJPH.2011.300214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winickoff JP, Hibberd PL, et al. Child hospitalization: an opportunity for parental smoking intervention. Am J Prev Med. 2001;21(3):218–220. doi: 10.1016/s0749-3797(01)00355-5. [DOI] [PubMed] [Google Scholar]
- Winickoff JP, Nabi-Burza E, et al. Implementation of a parental tobacco control intervention in pediatric practice. Pediatrics. 2013;132(1):109–117. doi: 10.1542/peds.2012-3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Cowling DW, et al. The impact of social norm change strategies on smokers’ quitting behaviours. Tobacco Control. 2010;19(Suppl 1):i51–i55. doi: 10.1136/tc.2008.029447. [DOI] [PMC free article] [PubMed] [Google Scholar]