Introduction
Pythiosis is an infectious disease caused by microorganisms of the Pythium genus, a form of funguslike oomycetes living in water-rich habitats. Human pythiosis is an emerging disease with a high rate of morbidity and mortality. Early recognition and management is crucial for successful treatment and outcomes. Because identifying the pathogen can be challenging, pythiosis might be easily misdiagnosed. Here we report a case of vascular pythiosis, the manifestation of which mimics medium-sized vasculitis.
Case report
A 54-year-old man presented with severe pain on his right thumb. Two months earlier, he had several subcutaneous nodules on his right forearm and bluish discoloration of his right thumb (Fig 1, A). He had no significant medical history and was not taking any medicines or herbs. He worked as a rice farmer and often was in contact with soil and mud. He had a 2 pack-year smoking history and excessive alcohol consumption. Skin biopsy was performed on the subcutaneous nodule for histology and microbiological culture. Three weeks later, his right thumb became gangrenous and the skin of his right second, fourth, and fifth digits became purplish-blue in color (Fig 1, B). The first histopathology finding showed large oval-shaped aggregates of mixed inflammatory cells, histiocytes, and multiple giant cells with negative special stains for bacteria, mycobacteria, and fungi. Results of tissue cultures were also all normal. Granulomatous vasculitis was suspected.
Fig 1.
Clinical manifestations. A, Multiple subcutaneous nodules along the right forearm with blue-colored skin of the right thumb. B, Gangrenous right thumb with blue-colored skin of the right second, fourth, and fifth digits.
Absent pulses of digital thumb arteries and radial artery of the right hand were found by digital palpation and confirmed with a Doppler probe. New fluctuant swelling of the right thenar eminence was also recognized. In addition, he appeared moderately pale and mildly jaundiced on examination. Angiogram of the right arm found total occlusion of radial and ulnar arteries with collateral flow to the hand. Balloon angioplasty of the ulnar artery was introduced. The abscess in the right thenar was drained and debrided; however, laboratory tests failed to identify microorganisms from the pus.
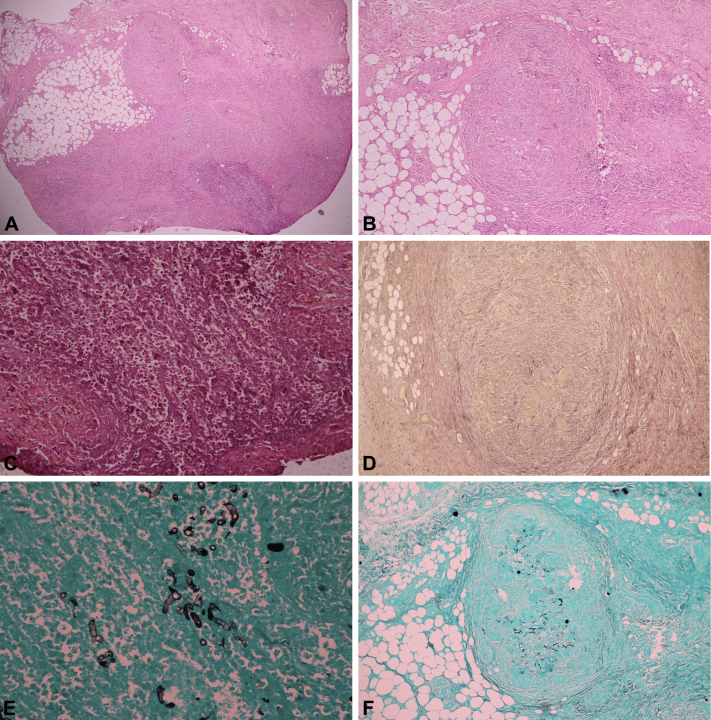
Histologic sections of the subcutaneous nodule were reviewed and favored an infectious process, as there was a large suppurative granuloma apart from the oval-shaped granuloma resembling an obliterated vessel (Fig 2, A–C). Special Verhoeff-van Gieson stains were requested to identify elastic fibers of vascular structures but could not be seen. The oval-shaped granuloma was identified as a nonvascular structure (Fig 2, D), and many broad ribbonlike hyphae were seen by Gomori methenamine silver (GMS) stain both in the suppurative and oval-shaped granulomas (Fig 2, E and F). At that time, members of the genus Pythium—an angioinvasive funguslike microorganism—were also considered possible pathogens in this susceptible patient, so a serologic test for Pythium antibody was performed with a weakly positive result. After the third debridement of the thenar area, Pythium insidiosum was eventually identified from debrided tissue and pus (Fig 3).
Fig 2.
Histopathology of subcutaneous nodule. A, Low magnification. B, Aggregration of mixed inflammatory cells, histiocytes, and multiple giant cells. C, Large suppurative granuloma. D, Verhoff-Van Gieson stain shows negative results. E, GMS stain shows broad, ribbonlike hyphae in a high magnification. F, GMS stain show broad, ribbonlike hyphae in the granuloma.
Fig 3.
Pythium culturing. A, Colonies growing on the media with grass leafs (the attractant). B, Zoospores spreading out from the sporangia after transferring the grass leaf to the water media.
The diagnosis of vascular pythiosis was presumed. Computed tomography angiography of the upper extremity was used to assess disease extension. Right radial and ulnar arteries were damaged, and the affected vessels appeared to extend proximally to the upper half of right brachial artery. Because the patient had sepsis, right above-elbow amputation was performed, and histopathology of the amputated limb confirmed the diagnosis of vascular pythiosis. There were large thrombi containing broad ribbonlike hyphae occluded within the lumen of radial and ulnar arteries. These vascular walls were severely destroyed (Fig 4, A and B). Moreover, in the normal-appearing brachial artery, there were small thrombi containing hyphae within the lumen (Fig 4, C-F). However, there were neither thrombi nor hyphae at the proximal end of the resected brachial artery, referring as an organism-free surgical margin.
Fig 4.
Histopathology of the amputated arm. A, Hematoxylin-eosin stain shows large thrombi containing hyphae and inflammatory cells occluded within the lumen of ulnar artery and hyphae invading the vascular wall. Vascular architecture is also destroyed. B, GMS stain confirms the presence of hyphae in the ulnar artery. C, Hematoxylin-eosin stain shows normal-looking brachial artery with small thrombi containing hyphae. D, GMS stain confirms the presence of hyphae in the brachial artery. E and F, GMS stain shows broad, ribbonlike hyphae in a high magnification.
Surgical treatment was combined with antifungal agents and triple-dose immunotherapy. Itraconazole 600 mg daily, terbinafine 500 mg daily, and saturated solution of potassium iodine 2,295 mg daily were administered. The patient's condition improved dramatically after amputation. However, the subsequent outcomes could not be evaluated, as he was lost to follow-up after discharge from the hospital. Moreover, he was newly diagnosed with hemoglobin constant spring trait, hepatitis C virus infection, and liver cirrhosis.
Discussion
Pythiosis in humans was first described in 1985 from Thailand.1 Thereafter, several cases have been reported mainly from Thailand and tropical countries.2 Four clinical presentations of human pythiosis have been described: cutaneous pythiosis, ocular pythiosis, vascular pythiosis, and pythiosis at unusual sites.1 Most Thai patients have had vascular pythiosis, followed by ocular pythiosis. Associated risk factors include agricultural exposures and underlying hematologic diseases, especially thalassemia. Most cases outside Thailand, however, have been diagnosed as cutaneous or ocular pythiosis, occurring in healthy hosts who have water-associated leisure activities.
Cutaneous pythiosis usually presents with a chronic ulcer or painful subcutaneous nodule. The most common sites are extremities, followed by the periorbital area. Most cases of ocular pythiosis manifest as a corneal ulcer or keratitis with a history of eye injury. Vascular pythiosis affects medium-to-large sized arteries and often manifests with chronic arterial insufficiency of the lower extremities, including intermittent claudication, gangrenous ulcers, and absent pulses. Soft tissue swelling or infection may be seen in some patients with vascular pythiosis. Vascular and disseminated pythiosis are life-threatening conditions with overall mortality rates of 40% and 100%, respectively. The leading causes of death are ruptured aneurysm and sepsis.3
Removal of infected tissue is key for successful treatment in pythiosis, as topical and systemic antifungal therapies are generally ineffective. Unlike fungi, oomycetes lack ergosterol in their cell membrane, and this might explain why patients with pythiosis have a poor response to conventional antifungal agents, which target ergosterol.2 However, in cutaneous form, a combination regimen of oral terbinafine and itraconazole has been reported to be effective in limited cases, and saturated solution of potassium iodine has shown some benefits.2, 4 Moreover, immunotherapy has been successfully used as an adjunctive therapy in vascular pythiosis.
P insidiosum has been responsible for virtually all cases of human pythiosis. Microbial cultures are considered positive when both a compatible colony and sporangia containing zoospores are seen. The zoospores are induced only in water media with plant materials or animal tissue. Apart from culturing, P insidiosum can be detected by serologic tests for antibody and by DNA sequencing.
Even though human pythiosis is a rare disease, we encourage clinicians to keep in mind the existence of such microorganism.
Footnotes
Funding sources: None.
Conflicts of interest: None decalred.
References
- 1.Krajaejun T., Sathapatayavongs B., Pracharktam R. Clinical and epidemiological analyses of human pythiosis in Thailand. Clin Infect Dis. 2006;43:569–576. doi: 10.1086/506353. [DOI] [PubMed] [Google Scholar]
- 2.Gaastra W., Lipman L.J., De Cock A.W. Pythium insidiosum: an overview. Vet Microbiol. 2010;146:1–16. doi: 10.1016/j.vetmic.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 3.Prasertwitayakij N., Louthrenoo W., Kasitanon N., Thamprasert K., Vanittanakom N. Human pythiosis, a rare cause of arteritis: case report and literature review. Semin Arthritis Rheum. 2003;33:204–214. doi: 10.1016/j.semarthrit.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Shenep J.L., English B.K., Kaufman L. Successful medical therapy for deeply invasive facial infection due to Pythium insidiosum in a child. Clin Infect Dis. 1998;27:1388–1393. doi: 10.1086/515042. [DOI] [PubMed] [Google Scholar]