Abstract
Drooling is a challenging situation to manage especially in neurologically impaired pediatric population. Numerous surgical procedures have been described in literature but none of them is standardized. We evaluate the effectiveness of bilateral submandibular duct rerouting and sublingual gland excision in drooling paediatric patients. Prospective interventional study was conducted from November 2007 to September 2009 in twenty-eight pediatric patients with drooling who had failed conservative treatment modalities. Patients underwent bilateral submandibular duct transposition and sublingual gland excision. Patients were assessed pre-operatively, at 7, 30 and 90 days after surgery for drooling severity, frequency as per Thomas-Stonell and Greenberg classification and also number of bibs changed per day. Result was categorized using Wilkie and Brody criteria for assessing effectiveness of the surgery. Twenty-eight patients were successfully operated. All patients were followed-up for a duration of at least 3 months. The success rate achieved in term of control of drooling was 95.2 % at 3 months follow up. Statistically significant difference (p < 0.001) was noted in pre-operative and postoperative mean values for severity and frequency of drooling and also bibs/day. Transient, minor complications (n = 5/28, 17.8 %) were encountered following this surgical procedure. Bilateral submandibular duct rerouting and sublingual gland excision in drooling paediatric patients is a simple and effective surgery with minor operative morbidity. Concomitant sublingual gland excision bilaterally helps in reducing the incidence of ranula formation significantly.
Keywords: Drooling, Submandibular duct re-routing, Submandibular duct transposition, Cerebral palsy, Ranula
Introduction
Drooling is unintentional loss of saliva from the mouth. It is considered physiological in children prior to the development of oral neuromuscular control. In a normal child this milestone is achieved by the age of 18–24 months. However, drooling after 4 years of age is uniformly considered abnormal. Cerebral palsy is the most common neuromuscular disorder associated with drooling in pediatric population. 10–37 % of patients with cerebral palsy have been reported to have drooling because of neurologic impairment [1].
Various treatment options are available for managing pathological drooling. Conservative methods include correction of posture, swallowing therapy and anti-cholinergic drugs. Injection of botulinum toxin locally into the salivary glands is a minimally invasive procedure, but needs repetitions and is expensive. Surgical intervention is offered when conservative treatment options fail or when drooling is severe. Patients with subnormal mental status who cannot comply with physiotherapy or drug therapy are also candidates for surgery. Numerous surgical procedures described in literature are different combinations of salivary gland excision, salivary duct rerouting and salivary duct ligation. However, none of them is considered as gold standard for the surgical management of drooling. Bilateral submandibular duct diversion and sublingual gland excision is a simple procedure with persistently good results and durability [2]. Preservation of physiologic function, decrease in the resting salivary flow volume and relatively low morbidity make this procedure ideal for pediatric patients. This study shares our institutional experience of bilateral submandibular duct transposition and sublingual gland excision for drooling in 28 pediatric patients.
Materials and Methods
This prospective interventional study was conducted in a tertiary care centre over a period of 2 years (2007–2009) after obtaining institutional ethical clearance. Patients with failed conservative treatment for drooling were referred from the department of Pediatrics Neurology for surgical management. They were evaluated quantitatively by the care giver as well as the author using Thomas-Stonell and Greenberg classification (Table 1) which consists of a 5-point scale for severity and a 4-point scale for frequency [2]. Drooling was judged in three different situations i.e., at rest, at meal time and during an engaged situation, e.g. at play or while watching television. The mean of all the scores was considered as the final score for severity and frequency of drooling. The number of bibs or clothes changed per day was also noted. The inclusion criteria for surgical enrollment include patients between the age group of 5–18 years having drooling severity ≥ 3 and frequency ≥ 3. Patients with history of salivary aspiration or those not fit for general anesthesia were excluded from the study. Informed written consent was taken from parents of all patients after explaining surgical procedure and associated complications.
Table 1.
Thomas-Stonell and Greenberg classification for drooling severity and frequency
| Severity |
| Score 1: Dry |
| Score 2: Mild-wet lips |
| Score 3: Moderate-wet lips and chin |
| Score 4: Severe–clothing damp |
| Score 5: Profuse-clothing, hands and objects wet |
| Frequency |
| Score 1: Never |
| Score 2: Occasionally (not every day) |
| Score 3: Frequently (every day) |
| Score 4: Constantly |
A total of 28 patients were included in the study out of whom 22 were male and six were female patients. Age range was 5–15 years with a mean age of 9.14 years. All patients were followed up for at least 3 months. The most common pathological etiology responsible for impaired neuromuscular control with consequent drooling was cerebral palsy (57.1 %). Other causes were global developmental delay (14.3 %), hypoxic ischemic encephalopathy (14.3 %), epilepsy (10.7 %) and pseudo bulbar palsy (3.6 %). 27 patients were mentally retarded as per their Intelligence Quotient (IQ) or its equivalent.
All patients were operated under general anaesthesia. After excluding adenoid hypertrophy nasal intubation was preferred to provide adequate access to the oral cavity. Wharton’s duct opening was identified by visualization of outpouring of saliva by pressing the submandibular gland externally. Surgical microscope was used in difficult cases. A rhomboid shaped incision was made around the papilla of the submandibular duct opening including a cuff of mucosa around it (Fig. 1). It was then dissected with the help of micro instruments from the surrounding tissues for a length of about three cm (Fig. 2) avoiding injury to the lingual nerve. A sub-mucosal tunnel was made in the floor of mouth which opened posteriorly at the junction of the base of tongue and anterior tonsillar pillar (Fig. 3). The duct along with the cuff of mucosa was brought through the tunnel and the papilla was fixed at the posterior opening (Fig. 4) with sutures. The ipsilateral sublingual gland was excised. The whole procedure was then repeated on the other side. After achieving hemostasis the mucosal defect in the floor of mouth was closed longitudinally to prevent post-operative restricted tongue mobility. At the end of the procedure nasogastric tube was inserted. Complications like pain, swelling in the floor of mouth, hematoma, sialadenitis and aspiration were evaluated and managed accordingly.
Fig. 1.
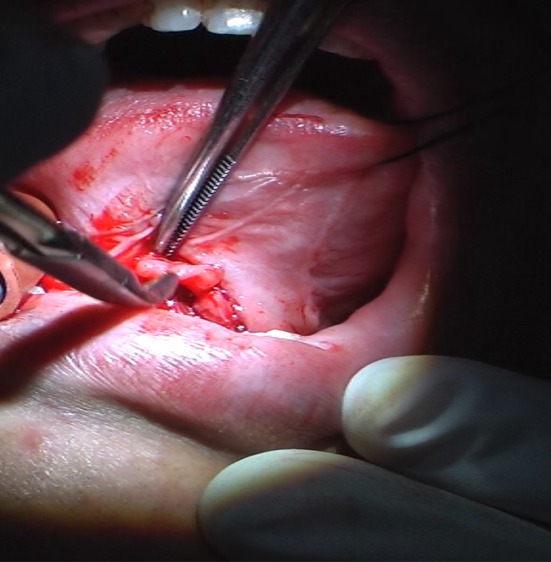
Rhomboid shaped mucosal incision around the papilla
Fig. 2.
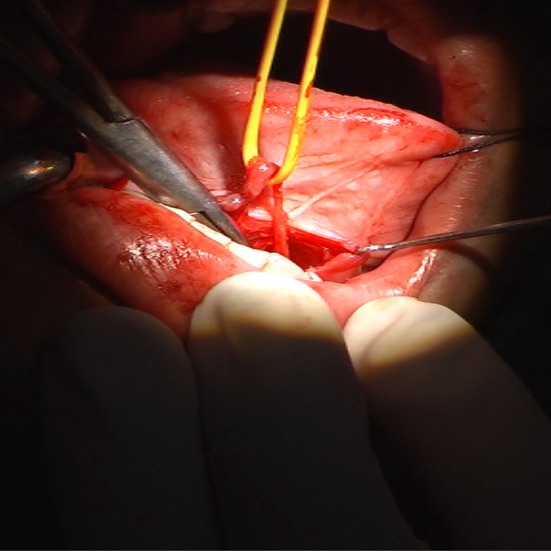
Dissecting the submandibular duct from surrounding tissue
Fig. 3.
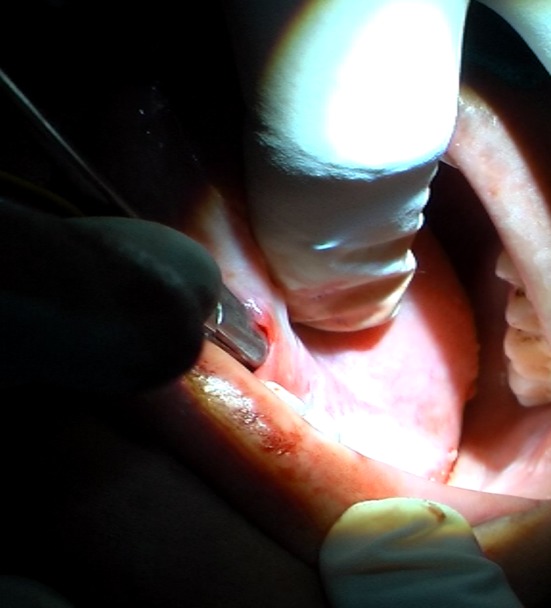
Making a submucosal tunnel
Fig. 4.
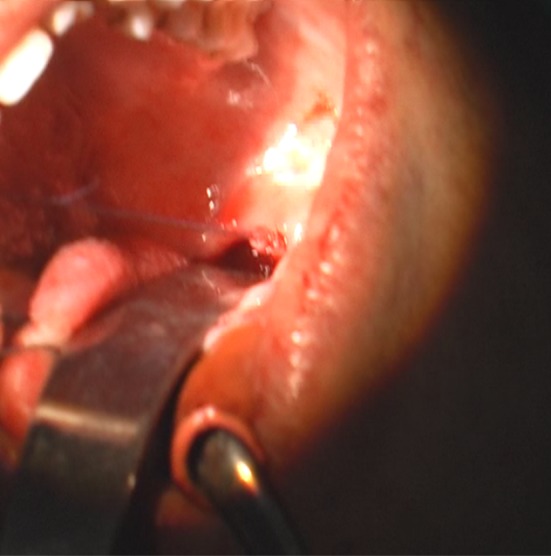
Submandibular duct brought out through the submucosal tunnel
Postoperatively patients were evaluated at 1 week, one month and three months. Degree of drooling was assessed by Thomas-Stonell and Greenberg classification, number of bibs/clothes changed/day and Wilkie and Brody criteria (Table 2). The result was defined as successful when the score improved by at least 1 point on scale and the patient showed fair-excellent result based on Wilkie and Brody criteria. Also complications like ranula formation, sialadenitis, xerostomia, caries tooth and aspiration were looked for during each visit and recorded in patient follow-up chart.
Table 2.
Wilkie and Brody criteria
| Excellent: Apparently normal control of saliva |
| Good: Slight loss of saliva with or without salivary leak or dried both lips |
| Fair: Improved, but with significant residual saliva loss |
| Poor: Failure of significant control or too dry |
Results
The mean number of bibs changed per day, severity score and frequency score as evaluated pre-operatively and on post-operative day 7, 30 and 90 are summarized in Table 3. Applying Friedman test and multiple comparison test, statistically significant difference (p < 0.0001) was found between pre-operative and post-operative mean values over day 30 and 90 in all categories. At 3 month follow up, the result of the surgery was successful in 95.2 % of patients taking an average of the success rate in severity, frequency and Wilkie and Brody criteria. The individual result of surgery in all categories is indicated in Table 4. A total of five patients (17.8 %) reported minor complications which were managed successfully. These include swelling of floor of mouth (n = 3/28), salivary aspiration (n = 1/28) and ranula formation (n = 1/28).
Table 3.
Mean drooling scores pre and post-operatively
| Mean score | Pre-operative | Post-operative day 7 | Post-operative day 30 | Post-operative day 90 |
|---|---|---|---|---|
| Bibs/day | 6.46 | 4.14 | 1.39 | 0.96 |
| Severity | 4.28 | 3.1 | 1.46 | 1.35 |
| Frequency | 3.85 | 3.07 | 1.39 | 1.39 |
Table 4.
Post-operative result classification of all patients
| Severity (%) | Frequency (%) | W&B critera (%) | |
|---|---|---|---|
| Success rate | 96.4 (27/28) | 92.85 (26/28) | 96.4 (27/28) |
| Improvement by 1 scale | 3.5 | 3.57 | Fair—7.1 |
| 2 Scales | 17.8 | 25 | Good—14.28 |
| 3 Scales | 46.4 | 64.28 | Excellent—75 |
| 4 Scales | 28.5 |
Discussion
Drooling is quite distressing to the parents as it requires constant care of the affected child. Often these children have subnormal intelligence which impedes the rehabilitation process. Drooling leads to perioral skin excoriation and infections, soiling of clothes, social embarrassment, isolation and subsequently poor performance in education and overall development of the child. Severe drooling may also lead to dehydration, malnutrition and dyselectrolytemia, when left untreated.
The available treatment options for drooling are correction of posture and positioning, oral awareness and oromotor skill training, orthodontic correction, anti-cholinergic drugs, Botulinum toxin injections and diverse surgical procedures. Surgery is planned when other treatment methods fail to give satisfactory result or when drooling is severe. Surgery should be deferred until the child is at least 5 years of age to allow neurological maturity which might improve drooling. The most commonly described surgical procedure in literature for drooling is rerouting of both Wharton’s ducts to tonsillar fossa. This procedure was first described by Laage-Hellmann [6] and subsequently adopted by others [3–5]. Submandibular glands produce 70 % of the resting salivary flow. So rerouting of the submandibular ducts preserves this physiologic function. Saliva from the relocated duct opening comes into contact with the base of tongue and initiates swallow reflex. Indirect evidence by radioisotope scanning indicates continued function of the submandibular glands at near-normal secretion rates following the procedure [6]. This simple trans-oral surgical procedure has been reported to have high success rate of 82.4–100 % [3–5, 7–13]. In our series success rate of 95.2 % was achieved at 3 months after surgery. The difference in the results at 1 and 3 months was not statistically significant. At 1 and 3 months, two patients had drooling similar to pre-operative level. Both these patients had poor head control and were constantly keeping their head flexed with mouth open.
Some authors have proposed concomitant sublingual excision along with duct relocation to prevent ranula formation. The incidence of ranula formation was up to 10 % when sublingual glands were preserved and up to 4 % when concomitant sublingual gland excision was performed [14]. However, there is no compelling evidence that sublingual gland excision improves the surgical outcome over duct relocation alone [15]. Addition of bilateral sublingual gland excision to submandibular duct transposition has shown success rate of 66–89 % in various series [15–19]. Sublingual gland excision is associated with increased postoperative pain, swelling in the floor of mouth and increased the surgical time. In our series, the incidence of ranula formation was 3.5 % (n = 1/28) without any compromise in the surgical success rate.
Tonsillectomy is a matter of debate in submandibular duct rerouting procedure. O’Dwyer et al. [20] stated that tonsillectomy should be performed initially as a separate procedure if there is a history of recurrent tonsillitis or if tonsils are grossly enlarged. On other hand, Crysdale [4] advocates a one-stage procedure when tonsils are large enough to obstruct the relocated ducts. In our series, rerouted duct was sutured at the base of the anterior tonsillar pillar and tonsillectomy was not performed in any of the patients. This modification was beneficial in terms of less surgical time, reduced postoperative pain and avoidance of the risk of hemorrhage associated with tonsillectomy. No case of obstructed salivary outflow was noted in our series due to the presence of tonsils, as evidenced by the absence of submandibular gland swelling post operatively.
Conclusion
Bilateral submandibular ducts rerouting along with sublingual gland excision is a simple and effective surgical procedure for children with drooling. High success rate and low morbidity makes this procedure ideal for patients with severe drooling or after failed conservative treatment. From our experience we realized that for high success and low complication rate, there should be minimal handling of the Wharton ducts and only one suture should be used to fix the duct at the posterior end of the sub-mucosal tunnel. Addition of bilateral sublingual gland excision leads to low incidence of ranula formation. Along with high success rate this surgery is associated with high parenteral satisfaction (which was assessed using Wilkie and Brody classification in our study). Post-surgical improvement in drooling is persistent over period of time, but follow-up is required to assess sequelae like xerostomia and dental caries.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Prem Sagar, Email: sagardrprem@gmail.com.
K. K. Handa, Email: handak@hotmail.com
Sheffali Gulati, Email: sheffaligulati@gmail.com.
Rajeev Kumar, Email: rajeev9843@yahoo.co.in.
References
- 1.Harris SR, Purdy AH. Drooling and it’s management in cerebral palsy. Dev Med Child Neurol. 1987;29:805–814. doi: 10.1111/j.1469-8749.1987.tb08830.x. [DOI] [PubMed] [Google Scholar]
- 2.Thomas-Stonell N, Greenberg J. Three treatment approaches and clinical factors in the reduction of drooling. Dysphagia. 1988;3:73–78. doi: 10.1007/BF02412423. [DOI] [PubMed] [Google Scholar]
- 3.Guerin RL. Surgical management of drooling. Arch Otolaryngol. 1979;105:535–537. doi: 10.1001/archotol.1979.00790210033007. [DOI] [PubMed] [Google Scholar]
- 4.Crysdale NS, White A. Submandibular duct relocation for drooling: a 10-year experience in 194 patients. Otolaryngol Head Neck Surg. 1989;101:87–92. doi: 10.1177/019459988910100114. [DOI] [PubMed] [Google Scholar]
- 5.Cotton RA, Richardson MA. The effect of submandibular duct rerouting in the treatment of sialorrhoea in children. Otolaryngol Head Neck Surg. 1981;89:535–541. doi: 10.1177/019459988108900405. [DOI] [PubMed] [Google Scholar]
- 6.Laage-Hellmann JE. Retroposition augl submandibularis utforsgang som behandling vid drazling. Nordisk Med. 1969;82:1522. [Google Scholar]
- 7.Panarese A, Ghosh S, Hodgson D, McEwan J, Bull PD. Outcomes of submandibular duct re-implantation for sialorrhoea. Clin Otolaryngol Allied Sci. 2001;26:143–146. doi: 10.1046/j.1365-2273.2001.00439.x. [DOI] [PubMed] [Google Scholar]
- 8.Crysdale WS. The drooling patient: evaluation and current surgical options. Laryngoscope. 1980;90(5, pt 1):775–783. doi: 10.1288/00005537-198005000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Talmon Y, Podoshin L, Fradis M. The surgical treatment of drooling in healthy children. Int J Pediatr Otorhinolaryngol. 1981;3(1):55–61. doi: 10.1016/0165-5876(81)90019-7. [DOI] [PubMed] [Google Scholar]
- 10.Bailey CM, Wadsworth PV. Treatment of the drooling child by submandibular duct transposition. J Laryngol Otol. 1985;99(11):1111–1117. doi: 10.1017/S0022215100098273. [DOI] [PubMed] [Google Scholar]
- 11.Mankarious LA, Bottrill ID, Huchzermeyer PM, Bailey CM. Long-term follow-up of submandibular duct rerouting for the treatment of sialorrhoea in the pediatric population. Otolaryngol Head Neck Surg. 1999;120(3):303–307. doi: 10.1016/S0194-5998(99)70266-4. [DOI] [PubMed] [Google Scholar]
- 12.Fear DW, Hitchcock RP, Fonseca RJ. Treatment of chronic drooling: a preliminary report. Oral Surg Oral Med Oral Pathol. 1988;66(2):163–166. doi: 10.1016/0030-4220(88)90085-0. [DOI] [PubMed] [Google Scholar]
- 13.Ethunandan M, Macpherson DW. Persistent drooling: treatment by bilateral submandibular duct transposition and simultaneous sublingual gland excision. Ann R Coll Surg Engl. 1998;80:279–282. [PMC free article] [PubMed] [Google Scholar]
- 14.O’Dwyer TP, Trimon C, Walsh MA. Surgical management of drooling in the neurologically damaged child. J Laryngol Otol. 1989;103:750–752. doi: 10.1017/S0022215100109971. [DOI] [PubMed] [Google Scholar]
- 15.Glynn F, O’Dwyer TP. Does the addition of sublingual gland excision to submandibular duct relocation give better overall results in drooling control? Clin Otolaryngol. 2007;32:103–107. doi: 10.1111/j.1365-2273.2007.01388.x. [DOI] [PubMed] [Google Scholar]
- 16.De M, Adair R, Golchin K, et al. Outcomes of submandibular duct relocation: a 15-year experience. J Laryngol Otol. 2003;117:821–823. doi: 10.1258/002221503770716287. [DOI] [PubMed] [Google Scholar]
- 17.Crysdale WS, Raveh E, Mc Cann C, Roske L, Kotler A. Management of drooling in individuals with neurodisability: a surgical experience. Dev Med Child Neurol. 2001;43:379–383. doi: 10.1017/S0012162201000718. [DOI] [PubMed] [Google Scholar]
- 18.McAloney N, Kerawala CJ, Stassen LF. Management of drooling by transposition of the submandibular ducts and excision of the sublingual glands. J Ir Dent Assoc. 2005;51(3):126–131. [PubMed] [Google Scholar]
- 19.Hornibrook J. Contemporary surgical management of sialorrhoea. ANZ J Surg. 2007;77(Suppl 1):A57. doi: 10.1111/j.1445-2197.2007.04125_9.x. [DOI] [Google Scholar]
- 20.Dwyer O. TP, Conlon BJ. The surgical management of drooling-a 15-year follow up. Clin Otolaryngol Allied Sci. 1997;22:284–287. doi: 10.1046/j.1365-2273.1997.00022.x. [DOI] [PubMed] [Google Scholar]


