Table 2.
Antimicrobial treatment recommendations for appendicitis and extra-biliary IAIs in adults.
| Guideline | Indication | Treatment |
|---|---|---|
| SIS-IDSA [2] | Community-acquired IAIs of mild-moderate severity including perforated or abscessed appendicitis | Single agent
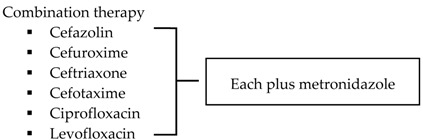
|
| Community-acquired IAIs of high risk or severity a | 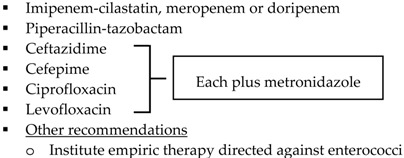 |
|
| Hospital-acquired IAIs | 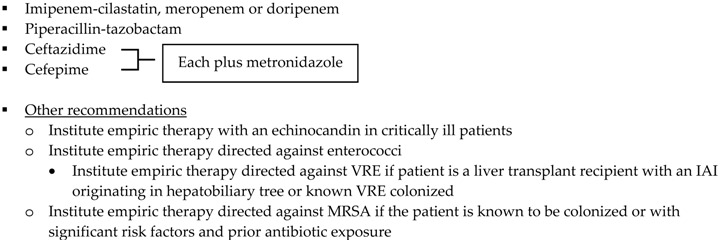 |
|
| WSES [3] | Community-acquired extra-biliary IAIs | Stable, non-critical patients with no risk factors for ESBL pathogens b
|
Stable, non-critical patients
with risk factors for ESBL pathogens b
| ||
Critically ill patients with no risk factors for ESBL pathogens b
| ||
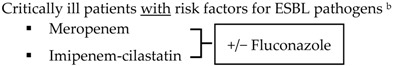 | ||
| Hospital-acquired extra-biliary IAIs | Stable, non-critical patients
with risk factors for MDR pathogens c
|
|
Critically ill patients
with risk factors for MDR pathogens c
|
SIS-IDSA: Surgical Infection Society and the Infectious Diseases Society of America; WSES: World Society of Emergency Surgery; Echinocandins: anidulafungin, caspofungin or micafungin; VRE: vancomycin-resistant enterococci; MRSA: methicillin-resistant Staphylococcus aureus. a High risk or severity includes delay in initial intervention for >24 h, APACHE II score ≥15, advanced age, comorbidity and organ dysfunction, low albumin level, poor nutritional status, degree of peritoneal involvement or diffuse peritonitis, inability to achieve source control, presence of malignancy. b Risk factors for ESBL pathogens include prior exposure to antibiotics (especially third generation cephalosporins), serious comorbid conditions requiring concurrent antibiotic therapy, residence in a long-term care facility, recent hospitalization, advanced age >65 years. c Risk factors for MDR pathogens include nosocomial-acquired infections and prior exposure to antibiotics.
