Abstract
Purpose
To determine working distance, pupil diameter and illumination in real life conditions in a sample of presbyopic participants performing habitual tasks.
Methods
A total of 59 presbyopic subjects (aged between 45 and 63 years) with different occupational backgrounds participated in the study. Participants were first interviewed regarding their habitual tasks with the aid of an ad hoc questionnaire, following which in-office photopic and mesopic pupil diameter was determined. Pupil diameter was also evaluated while participants conducted each of the self-reported habitual tasks by taking a photograph, which was later submitted to image analysis. In addition, working distance was determined with a measuring tape and the illumination that reached the pupil during each of the different tasks was measured, in lux, with a light meter.
Results
The four most common habitual tasks were computer use, reading, sewing and sports. A high intersubject variability was found in pupil diameter, working distance and illumination conditions while conducting the same task. Statistically significant differences were found between the in-office measured photopic and mesopic pupil diameters and those obtained while participants were conducting their habitual tasks in real life conditions (all p < 0.001).
Conclusions
Potential multifocal contact lens users may present with different ages, different jobs or hobbies and different preferences regarding lighting conditions and working distances. This results in different pupil size, even within the same task. This information may be critical when selecting a particular lens design and add power. Eye care practitioners are therefore advised to assess pupil diameter in real life conditions.
Keywords: Multifocal contact lens, Presbyopia, Pupil diameter, Simultaneous vision, Working distance
Resumen
Objetivo
Calcular la distancia de trabajo, el diámetro pupilar y la iluminación en situaciones de la vida real, en una muestra de participantes con presbicia, durante la realización de tareas habituales.
Métodos
En el estudio participaron un total de 59 sujetos con presbicia (de edades comprendidas entre 45 y 63 años), con diferentes perfiles ocupacionales. Primeramente, se preguntó a los participantes acerca de sus tareas habituales con la ayuda de un cuestionario ad hoc, tras el cual se determinó el diámetro pupilar fotópico y mesópico, durante la realización de la tarea. Igualmente, se evaluó el diámetro pupilar mientras los participantes realizaban cada una de las tareas habituales auto-reportadas, tomando una fotografía, a la que posteriormente se realizó un análisis de imagen. Además, se calculó la distancia de trabajo con una cinta métrica, además de medir, en lux, la iluminación que llega a la pupila durante cada una de las diferentes tareas.
Resultados
Las cuatro tareas más comunes y habituales fueron: uso del ordenador, lectura, costura y deportes. Se halló una variabilidad inter-sujetos en términos de diámetro pupilar, distancia de trabajo y condiciones de iluminación, durante la realización de la misma tarea. Se hallaron diferencias estadísticamente significativas entre los diámetros pupilares fotópico y mesópico medidos en el gabinete optométrico y aquéllos evaluados durante la realización de las tareas habituales en situaciones de vida real (todas las p < 0.001).
Conclusiones
Los potenciales usuarios de lentes multifocales presentan diferentes edades, diferentes trabajos o hobbies, y distintas preferencias, en relación a las condiciones de iluminación. Esto resulta en diferentes diámetros pupilares incluso al realizar la misma tarea. Esta información puede ser fundamental a la hora de seleccionar el diseño y la adición de una lente en particular, y añadir una potencia diferente. Por ello, se aconseja la evaluación del diámetro pupilar en las situaciones de la vida real, por parte de los profesionales de la salud visual.
Palabras clave: Lentes multifocales, Presbicia, Diámetro pupilar, Visión simultánea, Distancia de trabajo
Introduction
With a prediction of 21% of the world population aged 60 years or older in 2050,1 presbyopia may become one of the most pressing visual concerns of the 21st Century, particularly in developed countries in which visual demands for near and intermediate vision may be different late in life. Optical and refractive options for presbyopic patients are well documented.2, 3 Contact lenses for presbyopia are traditionally based on translation (mostly rigid gas permeable lenses) or simultaneous vision (mostly hydrogel or silicone-hydrogel materials) principles, with monovision offering an alternative for these patients.4, 5 Simultaneous vision relies on lens designs providing two or more foci through which incoming light from distant and near (and intermediate) objects falls on the retinal plane.6
For simultaneous vision to be effective, light energy distribution to the various foci must be similar, that is, pupil coverage for the distance and near (and intermediate) areas of the lens needs to be approximately the same, although some controversy exists regarding the extent of the deviations that still lead to operative simultaneous vision.7, 8, 9 In fact, even those lens designs labeled as pupil independent, based on successive concentric distance and near vision regions, with spherical aberration providing a certain degree of intermediate vision, require a minimum pupil diameter to work.9, 10, 11
Success with simultaneous vision contact lenses is also influenced by age. Indeed, as presbyopia advances, patients require higher add powers for near vision, that is, larger power gradient across the lens surface.12 Besides, pupil diameter tends to decrease with age, and with it the useful optic zone of the lens. Ocular spherical aberration becomes more positive with age,13 although large inter-subject variations in spherical aberration have been reported.14 The joint contribution of these factors leads to an increase in depth of focus which, in addition to the reported better tolerance to defocus in elder patients,15 has been found to result in changes in the subjective depth of focus of about 0.027 D per year from the age of 21–50 years.16
Given the variety of simultaneous vision lens designs, contact lens practitioners base their lens selection on their knowledge of power distribution for each lens type (information not always provided by the manufacturer) and on the specific visual demands of their patients for distance, intermediate and near tasks. Successful multifocal contact lens fitting has been associated with the expertise of practitioners and with correct lens selection,17 although even then contact lens dropout remains particularly high in this correction modality, with many patients reporting unsatisfactory vision as their main reason for lens discontinuation.18 Whereas high contrast visual acuity is usually good with multifocal contact lenses, their biggest challenge is contrast sensitivity loss, photic phenomena and underperformance in challenging situations such nighttime driving.19, 20, 21, 22
Pupil size, as part of the near vision triad (accommodation, convergence and miosis), is influenced by working distance, as well as by the level of illumination under which each task is conducted. In addition, even within the same task, illumination and working distance, pupil diameter has been shown to present with significant differences between individuals.23 The joint contribution of these factors may help explain differences in subjective visual satisfaction. Besides, in regards to illumination, it may be safely assumed that some tasks are undertaken under less than ideal and/or different conditions from those under which in-office pupil diameter was assessed, thus resulting in suboptimal performance of the selected lens design. A similar reasoning may apply to working distance for each task.
It was therefore the aim of the present study to further explore the suggestions of Plainis and co-workers24 and determine pupil diameter, working distance and illumination conditions in a group of presbyopic participants while they were conducting their habitual tasks, such as reading, working with the computer, etc., in their individual real life conditions. Pupil diameter was then compared with in-office measurements under photopic and mesopic conditions. Although in-office measurements aim at establishing the normal range of pupil diameters for a particular patient, this information alone may not be sufficient when selecting the best contact lens design for a combination of habitual tasks conducted at home or at the workplace under different levels of illumination. By highlighting the wide diversity of working distances and illumination conditions (and thus, pupil diameters), even within the same task, the goal of the present study was to increase the awareness of practitioners of the need to assess these parameters in conditions as similar as possible to those encountered by each individual patient in his or her daily activities.
Materials and methods
Study sample
A total of 59 presbyopic subjects participated in the study, which took place in Terrassa (Spain) between October of 2013 and January of 2014. Aiming at sample representativeness, participants were recruited from different vocations, resulting in a diversity of visual demands and habitual tasks (both at home and at the workplace). The most common jobs were: clerical worker (10); shop assistant (7); education related (6); health related (5); middle or senior management (5). Inclusion criteria were age between 45 and 65 years (inclusive), refractive error between +5.00 and −5.00 D, ocular astigmatism <−2.00 D and corrected monocular and binocular visual acuity at distance and near equal or better than 0.0 logMAR. Participants manifesting any eye disease, dry eye, binocular vision abnormalities or amblyopia, anisometropia >1.00 D, or a clinically significant anisocoria of 0.4 mm or larger were excluded from the study. Both spectacle and contact lens wearers were included in the study.
All participants provided written informed consent after the nature of the study was explained to them. The study was conducted in accordance with the Declaration of Helsinki tenets of 1975 (as revised in Tokyo in 2004) and received the approval of an institutional review board (School of Optics and Optometry of Terrassa).
Procedure
Subjects were first interviewed with the aid of an ad hoc questionnaire in which they indicated the number of hours per week that they allocated to two habitual tasks, either at home or at the workplace, and they also reported the visual satisfaction while undertaking these tasks. Visual satisfaction was graded with a vertical visual analog scale ranging from 0 to 10 cm (defined as “very unhappy with my vision quality” and “very happy with my vision quality”, respectively). In addition, even though it was not the purpose of the present study, past and present contact lens use was also documented.
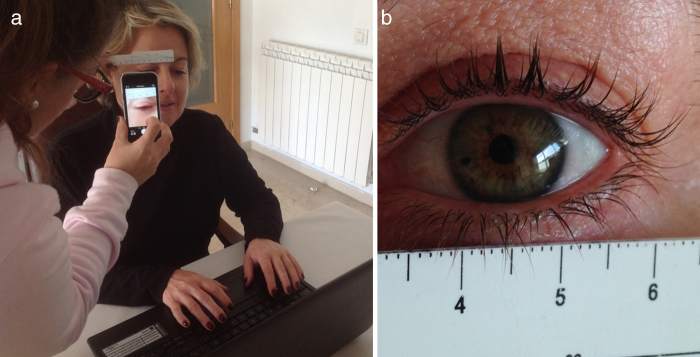
After completing the questionnaire, pupil diameter was determined while participants conducted their described habitual tasks at home and/or at the workplace, in exactly the same conditions in which they commonly conducted those tasks (all measurements were conducted at the site of the actual task). Pupillary diameter (in 1 mm steps) was assessed by capturing a picture with the mobile phone (Fig. 1a), and placing a ruler under or over the eye (between the eye and the spectacle frame, if necessary) for later reference during image analysis (Fig. 1b), which was conducted with the available tools in the open source software ImageJ 1.47v. Although, as far as we know, the actual mobile phone technique employed in the present study has not been previously described, pupil diameter assessment through image analysis has been reported as more repeatable and accurate, over a range of illuminations, than estimates by other clinical techniques.25 Photographs used for image analysis and pupil diameter measurement did not display any information regarding the task participants were performing at the time. Only horizontal pupil diameter was assessed. In participants with dark irises, image contrast was later manipulated for better observation and identification of the pupil. In addition, working distance from the plane of the task to the outer ocular canthus (in 1 cm steps) was determined with a measuring tape and the illumination during each of the different tasks was measured, in lux (lx), with a light meter GOSSEN MAVOLUX 5032 (GOSSEN Foto- und Lichtmesstechnik GmbH, Nürnberg, Germany), which was placed next to the head of the participants and facing the plane of the task.
Figure 1.
(a) Image capture during real conditions to determine pupil diameter. (b) Image capture of eye with reference rule.
Special care was taken when conducting measurements (particularly when placing the mobile phone and reference rule to assess pupil diameter) to avoid interfering with the attention of the participants or with his or her line of sight, that is, with the task being undertaken. All images were obtained by placing the mobile phone at approximately 40 cm in front of the eyes. All participants used their habitual distance and/or near prescription when conducting their tasks.
Pupil diameter was later examined while performing a routine visual examination under photopic (1000 lx) and mesopic (5 lx) conditions in the optometric practice, with the infrared Colvard pupillometer (Oasis Medical). During pupillometry, participants were instructed to fixate at a distant target. In office illumination was measured with the same light meter.
All experimental measures were conducted by the same, trained optometrist. For each parameter under evaluation, three consecutive measurements were conducted, and the mean of these values was used for data collection and statistical purposes
Data analysis
Statistical analysis was performed with the IBM SPSS software 19.0 for Windows (IBM Corporation, Armonk, NY). All data were analyzed for normality using the Kolmogorov–Smirnov test, revealing several instances of non-normal distributions which recommended a non-parametric approach. Therefore, descriptive data is presented in terms of median and range. The Wilcoxon test for matched pairs (the same participants were compared in different conditions) was employed to investigate the differences between in-office and real life pupil diameter data (for comparison purposes, habitual tasks were broadly classified into photopic or mesopic according to the measured illumination under which they were performed). In addition, the Spearman coefficient of correlation test (rho) was used to explore possible associations between the parameters under study. A p value of <0.05 was considered to denote statistical significance throughout the study.
Results
A total of 59 subjects (30 females) participated in the study, with a median age of 53 years (range from 45 to 63 years). No statistically significant difference in age was found between males and females. Forty-eight (81.4%) of the participants used glasses or contact lenses daily (11 participants were young presbyopes who, while not wearing distance correction, took advantage of their small myopic refractive error for near work). Of those requiring visual correction, 15 subjects were using or had used contact lenses. Interestingly, only 7 participants (11.9%) had tried multifocal contact lenses, with only one participant still using them at the time of the study. The rest of the participants reported poor vision as the main reason for discontinuation.
Information regarding in-office pupil diameters in photopic and mesopic conditions versus percentage of patients is presented in Table 1. Mean photopic pupil diameter was of 2.3 mm (±0.5 mm); mean mesopic pupil diameter was 5.4 mm (±0.6 mm). No statistically significant difference was encountered between males and females in either photopic or mesopic pupil diameter. As expected, a weak, albeit statistically significant correlation was found between photopic and mesopic pupil diameters (rho = 0.3; p = 0.021), that is, participants with larger pupils in photopic conditions also had larger pupils in mesopic conditions. However, no statistically significant association was disclosed between age and pupil diameter in the present sample of participants, although large pupil diameters in both photopic and mesopic conditions were usually found in the youngest presbyopic participants.
Table 1.
Percentage of patients in terms of pupil diameter in photopic (1000 lx) and mesopic (5 lx) conditions (in-office measurements). Mean and standard deviation (SD) values are also shown.
| Photopic |
Mesopic |
|||
|---|---|---|---|---|
| Range of Diameter (mm) | Percentage (%) | Range of Diameter (mm) | Percentage (%) | |
| 1.5–2.4 | 69.5 | 3.5–4.4 | 3.4 | |
| 2.5–3.4 | 27.1 | 4.5–5.4 | 57.6 | |
| ≥3.5 | 3.4 | 5.5–6.4 | 32.2 | |
| ≥6.5 | 6.8 | |||
| Mean | 2.3 | 5.4 | ||
| SD | 0.5 | 0.6 | ||
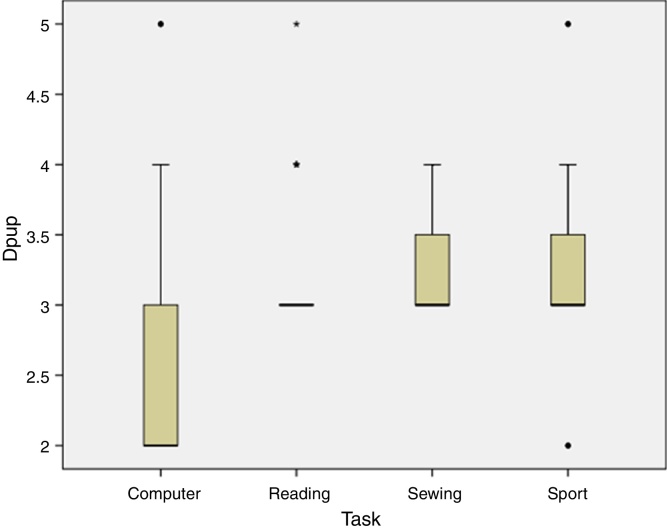
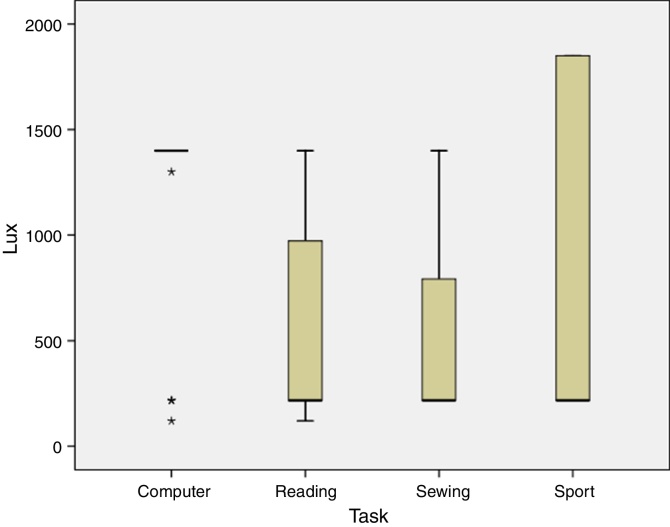
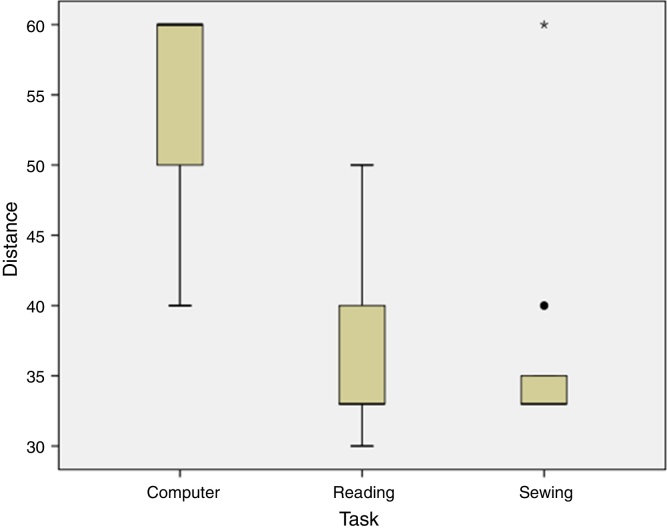
Participants were asked to name two habitual tasks they performed either at home or at the workplace, as well as an estimation of the approximate number of hours per week they devoted to each task. Table 2 displays a summary of the reported habitual tasks, with percentage of participants, and median and range of hours per week, visual satisfaction, measured pupil diameter, illumination (in lux) and working distance (measurements were conducted at the site of the actual task). Upon examining differences between individual data, a large variability of parameters was encountered. In effect, even if two participants reported undertaking the same task, in most cases their visual satisfaction, hours per week and, most notably, pupil diameter, illumination conditions and working distance were different. This variability in pupil diameter, illumination and working distance is shown in Figure 2, Figure 3, Figure 4, respectively, for 4 of the most commonly reported habitual tasks (reading, sports, computer use and sewing, all with more than 10% of respondents). Interestingly, when asked, the majority of participants reported that they read books and/or newspapers in print format, although a small minority possessed an e-book reader or tablet or read on the computer screen.
Table 2.
Habitual tasks, with details on number and percentage (%) of participants conducting each task (all participants named two habitual tasks), hours per week devoted to that task, visual satisfaction, pupil diameter, illumination and working distance while conducting the task in real-life conditions. Data is presented as median (minimum–maximum).
| Task | Number and (%) | Hours/week | Visual satisfaction (0–10) | Pupil diameter (mm) | Illumination (lx) | Working distance (cm) |
|---|---|---|---|---|---|---|
| Computera | 22 (18.6) | 30 (3–56) | 7 (5–10) | 2 (2–5) | 1400 (120–1400) | 60 (40–60) |
| Cooking | 2 (1.7) | 17.5 (15–20) | 8.5 (8–9) | 3.5 (3–4) | 217 | 60 |
| Drawing | 1 (0.8) | 20 | 8 | 3 | 1400 | 50 |
| Driving | 5 (4.2) | 30 (20–40) | 9 (7–9) | 2 (2–3) | 1850 | Far |
| Gym | 1 (0.8) | 12 | 10 | 3 | 217 | Far |
| Homecare | 4 (3.4) | 22 (14–40) | 7 (6–10) | 3 (2–4) | 1090 (217–1300) | 55 (40-Far) |
| Piano | 2 (1.7) | 5 (4–6) | 8 (7–9) | 4 | 792.5 (285–1300) | 55 (50–60) |
| Pilot | 1 (0.8) | 15 | 8 | 4 | 2300 | Far |
| Playing Cards | 2 (1.7) | 8 | 5.5 (5–6) | 4.5 (4–5) | 217 | 48.5 (42–55) |
| Readinga | 35 (29.7) | 10 (4–48) | 6 (1–9) | 3 (3–5) | 217 (120–1400) | 33 (30–50) |
| Restoring Furniture | 2 (1.7) | 20 (10–30) | 6 | 3 | 3400 | 40 (30–50) |
| Sewinga | 15 (12.7) | 10 (3–30) | 7 (2–9) | 3 (3–4) | 217 (217–1400) | 33 (33–60) |
| Participating in Sportsa | 19 (16.1) | 8 (3–50) | 9 (8–10) | 3 (2–5) | 217 (217–1850) | Far (60-Far) |
| Theater | 1 (0.8) | 10 | 9 | 4 | 120 | Far |
| TV | 5 (4.2) | 10 (10–20) | 8 (8–9) | 5 (3–5) | 2.7 | 200 (200–300) |
| Writing | 1 (0.8) | 12 | 4 | 4 | 1400 | 45 |
Denotes the four most common tasks. Parameters were measured at the site of the actual task.
Figure 2.
Pupil diameter (in mm) while performing 4 common habitual tasks (outliers are shown).
Figure 3.
Illumination conditions (in lx) while performing 4 common habitual tasks (outliers are shown).
Figure 4.
Working distance (in cm) while performing 3 common habitual tasks (sports is omitted as all sports involved far vision, with the exception of 2 participants) (outliers are shown).
In-office photopic and mesopic pupil diameter values were compared with those measured while participants conducted their habitual tasks. The Wilcoxon test for related samples disclosed statistically significant differences in all instances (all p < 0.001), that is, in a significant number of participants, pupil diameter, as measured during routine visual examination, was different from actual pupil diameter while performing their habitual tasks.
Finally, an analysis of the possible associations among these parameters with the Spearman coefficient of correlation test revealed a statistically significant positive correlation between visual satisfaction and working distance (rho = 0.581; p < 0.001), that is, participants reported a higher visual satisfaction with those tasks involving far vision. It must be noted that a weak, albeit statistically significant negative correlation (rho = −0.377; p = 0.003) was found between age and visual satisfaction, with older participants reporting lower levels of visual satisfaction with their habitual tasks.
Discussion
The present study aimed at exploring pupil diameter, working distance and illumination in a sample of presbyopic participants while they conducted their habitual tasks at home or at the workplace (i.e., at the site of the actual task) in real life conditions. Pupil diameter measurement is critical during simultaneous vision multifocal contact lens design selection. A small pupil, in a center near lens, may result in serious difficulties for distance vision, mainly in those lens designs in which the distant vision region is located more peripherally. Similarly, a large pupil (such as may occur while driving at night), might give rise to abundant photic phenomena if the patient is wearing a lens design with a power profile favoring near vision over a large area of its geometry.
The in-office measured average values of pupil diameter for photopic (2.3 ± 0.5 mm) and mesopic (5.4 ± 0.6 mm) conditions are in agreement with published data in presbyopic subjects, with small deviations accounting for differences in the age range of study participants,26, 27 although other authors reported larger pupil diameters in healthy subjects of similar age range.8, 28 However, illumination conditions were found to differ when participants conducted their habitual tasks in their preferred real life conditions, resulting in statistically significant differences in pupil diameter between in-office and daily life conditions. It may be assumed that these discrepancies would lead to relevant differences in the light distribution to distance and near foci in a theoretical simultaneous vision multifocal contact lens, particularly in pupil dependent designs, thus influencing visual performance during near, intermediate and near tasks. It must be noted that, even if information is available on the typical lighting levels (and corresponding pupil diameters) for common visual tasks such as driving at night, reading or office work,23, 29 the present findings gave support to the assumption that individual conditions differ from the published average values.
Besides, pupil diameter may be considered a very dynamic parameter, not only influenced by illumination but also by other factors, most importantly age and working distance. Winn and co-workers28 described a negative correlation between age and pupil diameter when measurements were conducted under the same illumination conditions (in fact, luminance from a 10° field of view stimulus was evaluated instead of illumination), as well as an overall decrease in pupil diameter at the highest levels of illumination. Our data analysis failed to reveal any statistically significant correlation between age and pupil diameter, a discrepancy which may be attributed to the relatively small and skewed age range in our sample or to our decision to present real life pupil measurements in 1 mm steps, rather than to take advantage of the superior resolution which was provided by our image analysis approach.
Observation distance is another important factor to be considered when selecting the best lens design for each patient, not only for its influence on pupil diameter, but also for the correct determination of the required add power of the lens. The present findings revealed working distances when using the computer or when reading ranging from 40 to 60 cm and from 30 to 50 cm, respectively. A change from 30 to 50 cm is equivalent to a change in 1 D of add power, that is, it may require a modification in lens selection, for example, from low to mid add power (in a lens design with three possible add powers).
In light of the disparity in pupil diameters, working distance and illumination conditions referring to the same task, it is not unexpected for presbyopic patients to report different levels of visual satisfaction, either with their multifocal correction, as previously documented,18, 30 or otherwise, as disclosed by the present findings, in which visual satisfaction was found to decrease with age, particularly for those tasks requiring intermediate or near vision. An interesting addition to the present study would have been to evaluate visual satisfaction with the same tasks while participants wore simultaneous vision contact lenses.
In conclusion, practitioners challenged with multifocal contact lens abandonment may be advised to obtain detailed information regarding the particular working distance and illumination conditions preferred by each patient while conducting his or her habitual tasks and to measure pupil diameter in those specific conditions. Given the encountered wide diversity in pupil diameters, even within the same task, arising from a similarly wide range of working distance-illumination combinations, in-office measurements alone may not provide with sufficient information to allow practitioners informed decisions when selecting the optimum lens design for a particular patient. However, even with this information, a certain degree of trial and error might be necessary, as available data on the power distribution of simultaneous vision contact lenses stems from in vitro studies employing sophisticated instrumentation and analysis,10, 11, 31 not readily available to the eye care practitioner.
Conflict of interest
None of the authors have any proprietary interests or conflicts of interest related to this submission.
References
- 1.United Nations Department of Economic and Social Affairs . 2013. Population Division. World Population Ageing 2013 (Document ST/ESA/SER.A/348), New York. [Google Scholar]
- 2.Charman W.N. Developments in the correction of presbyopia I. Ophthalmic Physiol Opt. 2014;34:8–29. doi: 10.1111/opo.12091. [DOI] [PubMed] [Google Scholar]
- 3.Charman W.N. Developments in the correction of presbyopia II. Ophthalmic Physiol Opt. 2014;34:397–426. doi: 10.1111/opo.12129. [DOI] [PubMed] [Google Scholar]
- 4.Bennett E.S. Contact lens correction of presbyopia. Clin Exp Optom. 2008;91:265–278. doi: 10.1111/j.1444-0938.2007.00242.x. [DOI] [PubMed] [Google Scholar]
- 5.Bennett E.S., Weissman B.A. 2nd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2004. Clinical Contact Lens Practice. [Google Scholar]
- 6.Young G., Grey C.P., Papas E.B. Simultaneous vision bifocal contact lenses: a comparative assessment of the in vitro optical performance. Optom Vis Sci. 1990;67:339–345. doi: 10.1097/00006324-199005000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Charman W.N., Saunders B. Theoretical and practical factors influencing the optical performance of contact lenses for the presbyope. J Br Contact Lens Assoc. 1990;13:67–75. [Google Scholar]
- 8.Chateau N., Baude D. Simulated in situ optical performance of bifocal contact lenses. Optom Vis Sci. 1997;74:532–539. doi: 10.1097/00006324-199707000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Bradley A., Nam J., Xu R., Harman L., Thibos L. Impact of contact lens zone geometry and ocular optics on bifocal retinal image quality. Ophthalmic Physiol Opt. 2014;34:331–345. doi: 10.1111/opo.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hough A. Soft bifocal lenses: the limits of performance. Cont Lens Anterior Eye. 2002;25:161–175. doi: 10.1016/s1367-0484(02)00060-7. [DOI] [PubMed] [Google Scholar]
- 11.Plainis S., Atchison D.A., Charman W.N. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013;90:1066–1077. doi: 10.1097/OPX.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 12.Cox I., Apollino A., Erickson P. The effect of add power on simultaneous vision, monocentric, bifocal, soft lens visual performance. Int Contact Lens Clin. 1993;20:18–21. [Google Scholar]
- 13.Atchison D.A., Markwell E.L. Aberrations of emmetropic subjects at different ages. Vision Res. 2008;48:2224–2231. doi: 10.1016/j.visres.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 14.Hartwig A., Atchison D.A. Analysis of higher-order aberrations in a large clinical population. Invest Ophthalmol Vis Sci. 2012;53:7862–7870. doi: 10.1167/iovs.12-10610. [DOI] [PubMed] [Google Scholar]
- 15.Wang B., Ciuffreda K.J. Depth-of-focus of the human eye: theory and clinical implications. Surv Ophthalmol. 2006;51:75–85. doi: 10.1016/j.survophthal.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Mordi J.A., Ciuffreda K.J. Static aspects of accommodation: age and presbyopia. Vision Res. 1998;38:1643–1653. doi: 10.1016/s0042-6989(97)00336-2. [DOI] [PubMed] [Google Scholar]
- 17.Montés-Micó R., Madrid-Costa D., Domínguez-Vicent A., Belda-Salmerón L., Ferrer-Blasco T. In vitro power profiles of multifocal simultaneous vision contact lenses. Cont Lens Anterior Eye. 2014;37:167. doi: 10.1016/j.clae.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 18.Gispets J., Arjona M., Pujol J., Vilaseca M., Cardona G. Task oriented visual satisfaction and wearing success with two different simultaneous vision multifocal soft contact lenses. J Optom. 2011;4:76–84. [Google Scholar]
- 19.Papas E.B., Decenzo-Verbeten T., Fonn D. Utility of short-term evaluation of presbyopic contact lens performance. Eye Contact Lens. 2009;35:144–148. doi: 10.1097/ICL.0b013e3181a20361. [DOI] [PubMed] [Google Scholar]
- 20.Kollbaum P.S., Dietmeier B.M., Jansen M.E., Rickert M.E. Quantification of ghosting produced with presbyopic contact lens correction. Eye Contact Lens. 2012;38:252–259. doi: 10.1097/ICL.0b013e31825aa879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chu B.S., Wood J.M., Collins M.J. Effect of presbyopic vision corrections on perceptions of driving difficulty. Eye Contact Lens. 2009;35:133–143. doi: 10.1097/ICL.0b013e3181a1435e. [DOI] [PubMed] [Google Scholar]
- 22.Chu B.S., Wood J.M., Collins M.J. The effect of presbyopic vision corrections on nighttime driving performance. Invest Ophthalmol Vis Sci. 2010;51:4861–4866. doi: 10.1167/iovs.10-5154. [DOI] [PubMed] [Google Scholar]
- 23.Koch D.D., Samuelson S.W., Haft E.A., Merin L.M. Pupillary size and responsiveness. Implications for selection of a bifocal intraocular lens. Ophthalmology. 1991;98:1030–1035. [PubMed] [Google Scholar]
- 24.Plainis S., Ntzilepis G., Atchison D.A., Charman N. Through-focus performance with multifocal contact lenses: effect of binocularity, pupil diameter and inherent ocular aberrations. Ophthalmic Physiol Opt. 2013;33:42–50. doi: 10.1111/opo.12004. [DOI] [PubMed] [Google Scholar]
- 25.Twa M.D., Bailey M.D., Hayes J., Bullimore M. Estimation of pupil size by digital photography. J Cataract Refract Surg. 2004;30:381–389. doi: 10.1016/S0886-3350(03)00619-9. [DOI] [PubMed] [Google Scholar]
- 26.Llorente-Guillemot A., García-Lázaro S., Ferrer-Blasco T., Pérez-Cambrodí R., Cerviño A. Visual performance with simultaneous vision multifocal contact lenses. Clin Exp Optom. 2012;95:54–59. doi: 10.1111/j.1444-0938.2011.00666.x. [DOI] [PubMed] [Google Scholar]
- 27.García-Lázaro S., Albarrán-Diego C., Ferrer-Blasco T., Radhakrishnan H., Montés-Micó R. Visual performance comparison between contact lens-based pinhole and simultaneous vision contact lenses. Clin Exp Optom. 2013;96:46–52. doi: 10.1111/j.1444-0938.2012.00791.x. [DOI] [PubMed] [Google Scholar]
- 28.Winn B., Whitaker D., Elliott D.B., Phillips N.J. Factors affecting light-adapted pupil size in normal human subjects. Invest Ophthalmol Vis Sci. 1994;35:1132–1137. [PubMed] [Google Scholar]
- 29.Menezes EV, Roffman JH. Multifocal lens designs with intermediate optical powers. European Patent Application no. EP 0 756 189 A2. European Patent Office, 1997.
- 30.Fernandes P.R.B., Neves H.I.F., Lopes-Ferreira D.P., Jorge J.M.M., González-Meijome J.M. Adaptation to multifocal and monovision contact lens correction. Optom Vis Sci. 2013;90:228–235. doi: 10.1097/OPX.0b013e318282951b. [DOI] [PubMed] [Google Scholar]
- 31.Wagner S., Conrad F., Bakaraju R.C., Fedtke C., Ehrmann K., Holden B.A. Power profiles of single vision and multifocal soft contact lenses. Cont Lens Anterior Eye. 2015;38:2–14. doi: 10.1016/j.clae.2014.07.008. [DOI] [PubMed] [Google Scholar]