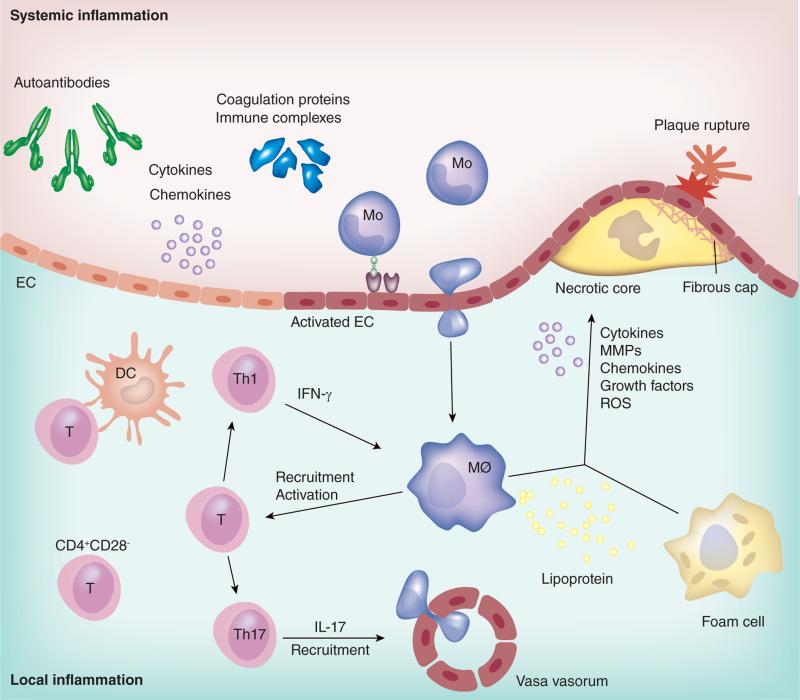
Figure 1. Pathophysiology of atherosclerosis in rheumatologic disease.
The major pathophysiology of atherosclerosis in rheumatologic disease is outlined. Systemic inflammation is accompanied by elevated cytokines, chemokines and coagulation proteins, which causes endothelial activation and dysfunction. Autoantibodies and immune complexes are hallmarks of autoimmune disease, and some of them have the potential to promote atherosclerosis. Activated ECs promote recruitment of Mos into the subendothelial space, where Mos differentiate into MØs. MØs ingest lipoproteins and become foam cells, and secrete cytokines, MMPs, chemokines, growth factors and ROS. These lead to the formation of a necrotic core and fibrous cap which is correlated with plaque rupture. Th1 cytokine IFN-γ activates MØs, and activated MØs further promote recruitment and activation of T cells. DCs interact with T cells, and Th17 cells promote recruitment of inflammatory cells. CD4+CD28− cells are reported to contribute to the development of atherosclerosis in RA as well as coronary artery disease.
DC: Dendritic cell; EC: Endothelial cell; MØ: Macrophage; MMP: Matrix metalloproteinase; Mo: Monocyte;
ROS: reactive oxygen species