Abstract
Classical inflammatory monocytes and their derivative macrophages promote tumor metastasis whereas CD8+ T and NK cells restrict tumor growth. In a recent paper published in Science, Hanna and colleagues demonstrate that another monocyte population, nonclassical patrolling monocytes, is enriched in the microvasculature of tumor-challenged lung and reduces tumor metastasis by recruiting NK cells.
Tumor metastasis accounts for 95% of cancer-related deaths in the developed world. In the past decade focus has shifted from study of cancer cells alone to the tumor microenvironment that consists of many cell types that overall support cancer progression. Circulating monocytes extravasate into the tissue and differentiate into macrophages, which are key players in the regulation of metastasis as they provide support for the extravasation, survival and growth of metastatic cancer cells1.
There are at least two circulating monocyte populations in the blood: classical “inflammatory” monocytes (IMo, CCR2HighLy6C+ in mouse; CCR2High CD14++CD16− in human) and nonclassical “patrolling” monocytes (PMo, CX3CR1HighLy6C− in mouse; CX3CR1HighCD14+CD16+ in human). IMo are recruited to inflammatory sites through the CCR2-CCL2 axis; they extravasate, differentiate into tissue macrophages and dendritic cells, and respond to bacterial and parasitic infections. In breast cancer models, IMo are also recruited via the CCL2-CCR2 axis to metastatic sites where they promote cancer cell extravasation and survival2.
PMo in steady state conditions are localized in the microvasculature of different organs via the CXC3R1-CX3CL1 axis, where they patrol the capillaries and scavenge cell debris and particles3. Different from IMo, PMo rarely extravasate into the tissue and differentiate into macrophages3. PMo depend on the transcription factor N4a1 for their development from bone marrow precursors4 and in pathological conditions they can respond to a variety of stimuli, contributing to resolution of inflammation5. In a recent study by Hanna et al.6, a new anti-tumoral function of PMo has been demonstrated in different models of murine metastasis. This function of mouse surveillance resulted in increased killing of metastatic cells by natural killer (NK) cells.
Using transgenic mice in which PMo, but not IMo, express GFP under the Nr4a1 promoter, the authors showed that PMo patrol the lung microvasculature in steady state conditions3. After injection of lung metastatic cancer cells, they observed reduced patrolling movement and an accumulation of PMo at the tumor site. PMo can extravasate within 4 h of tumor cell arrival. After 7 days, 40%-50% of PMo in the lung had extravasated7. Using Nr4a1−/− mice, in which PMo are selectively ablated, the authors showed that loss of Nr4a1 enhances metastatic seeding of injected tumor cells. Similar data were obtained in MMTV-PyMT mice that spontaneously develop metastatic mammary tumors. Female PyMT mice transplanted with Nr4a1−/− bone marrow developed more lung metastases than controls, suggesting that PMo are important for the suppression of lung metastasis.
Adoptive transfer of wild-type (WT) LyC6− monocytes into Nr4a1−/− mice prior to tumor cell injection inhibited metastasis to the lung, while injection of LyC6− monocytes into Nr4a1−/− mice after tumor injection did not, indicating that PMo need to be present in the vasculature before tumor cell arrival. In contrast, injection of IMo promoted metastatic growth, confirming the pro-tumoral role of IMo previously reported by others2.
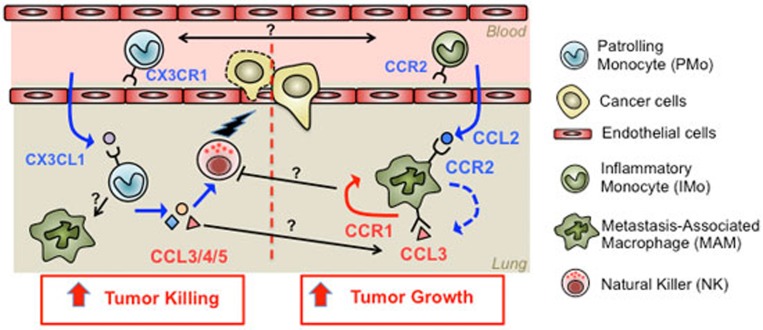
Hanna et al. focused on the scavenging properties of PMo. Using confocal microscopy they found that PMo engulfed tumor debris more efficiently than IMo via a mechanism mediated by CX3CR1, as its absence decreased debris uptake by PMo. CX3CR1 is required for the arrest of PMo at the tumor site because PMo from CX3CR1−/− mice did not accumulate at the tumor site in the lung. Using CX3CL1 mCherry mice the authors showed that CD31+ endothelial cells express CX3CL1 at low levels in the lung microvasculature and that this expression was increased after tumor challenge, suggesting that the CX3CR1-CX3CL1 axis could be associated with PMo recruitment to the tumor site (Figure 1).
Figure 1.
Pro- and anti-tumoral functions of IMo and PMo in the lung metastatic site. Left panel, PMo are recruited by endothelial cells expressing CX3CL1 in response to tumor cell accumulation; they extravasate into the lung tissue where they express CCL3/4/5 and potentially recruit cytotoxic NK cells. Right panel, IMo are recruited by the tumor via a CCL2-mediated mechanism; they extravasate into the lung tissue where they differentiate into MAMs and interact with cancer cells, promoting their extravasation and the formation of micrometastasis. These recruited IMo differentiate into MAMs and secrete CCL3 that enhances their retention in the tissue. Question marks represent open questions to be investigated, i.e., the potential interaction/competition between IMo and PMo to get access to the tumor site, the potential ability of PMo to differentiate into MAMs, the potential interaction between MAMs and NK cells in the tissue and the pro-tumoral and anti-tumoral effects exerted by monocyte/macrophage-derived CCL3.
The recruited PMo could not directly kill tumor cells but they expressed higher levels of chemokines, CCL3, CCL4 and CCL5, compared to IMo. These chemokines can recruit NK cells, and indeed lung metastases from PyMT mice that received bone marrow from N4a1−/− mice showed reduced NK cell recruitment to the tumor site. This suggests that PMo exert their anti-tumoral function by recruiting NK cells to the lung, which kill the invading cells. This work therefore demonstrates that Ly6C− patrolling monocytes can respond to the presence of early metastasis in the lung and exert an anti-tumoral activity.
Different reports have demonstrated the complex dynamics of Ly6C+ and Ly6C− monocyte recruitment in the absence of injury8. Hanna et al. showed that both IMo and PMo were recruited to the tumor site 4 h after tumor cell injection but the number of PMo was significantly lower than that of IMo even though more stable over time. PMo extravasate to the lung in response to septic and aseptic injury3 and they can differentiate into classical and nonclassical macrophages9. In this report the authors did not show whether PMo could differentiate into macrophages. It would be interesting to investigate whether PMo can be “corrupted” by cancer cells once they extravasate and be converted to pro-tumoral cells. It would also be interesting to assess whether IMo and PMo compete for access to the tumor site and whether IMo can suppress the anti-tumor function of PMo by, for example, inhibiting NK cell activity once they become metastasis-associated macrophages (MAMs). This may be a mechanism whereby some tumor cells escape from being killed and progress to full-blown metastasis. This mechanism is also consistent with the data from the PMo adoptive transfer experiments since PMo appear to act early during seeding but not after establishment of metastatic foci despite their continued accumulation.
PMo express higher levels of CCL3/4/5 compared to IMo and are potentially able to recruit NK cells to the tumor site. This is consistent with other studies showing that intravenously injected B16 melanoma cells develop more lung metastatic foci in Ccl3−/− mice than WT mice10. However, recent studies demonstrated that IMo are retained in the metastatic site through a CCL3-dependent mechanism11 and promote tumor cell survival. It would be interesting to assess using conditional genetics whether PMo-derived CCL3 recruits NK cells and at the same time affects MAM retention. It would also be interesting to study less immunogenic metastasis models using different mechanisms of seeding, as the imaging in the present study revealed that the tumor cells were in clumps, suggesting potential tumor proliferation within vessels as reported by others12. Quantitation of cancer cells at different steps could identify the step when tumor cell loss occurs.
In conclusion, the study by Hanna et al.6 sheds new light on the role of PMo during metastasis formation and opens new questions regarding crosstalk between IMo and PMo and their potential dual roles in tumor progression. Enhancement of PMo-mediated immune blockade therapeutically might reduce the already inefficient metastatic process below a threshold such that metastasis does not occur.
References
- Kitamura T, Qian BZ, Pollard JW. Nat Rev Immunol 2015; 15:73–86. [DOI] [PMC free article] [PubMed]
- Qian BZ, Li J, Zhang H, et al. Nature 2011; 475:222–225. [DOI] [PMC free article] [PubMed]
- Auffray C, Fogg D, Garfa M, et al. Science 2007; 317:666–670. [DOI] [PubMed]
- Hanna RN, Carlin LM, Hubbeling HG, et al. Nat Immunol 2011; 12:778–785. [DOI] [PMC free article] [PubMed]
- Hanna RN, Shaked I, Hubbeling HG, et al. Circ Res 2012; 110:416–427. [DOI] [PMC free article] [PubMed]
- Hanna RN, Cekic C, Sag D, et al. Science 2015; 350:985–990. [DOI] [PMC free article] [PubMed]
- Carlin LM, Stamatiades EG, Auffray C, et al. Cell 2013; 153:362–375. [DOI] [PMC free article] [PubMed]
- Yona S, Kim KW, Wolf Y, et al. Immunity 2013; 38:79–91. [DOI] [PMC free article] [PubMed]
- Misharin AV, Cuda CM, Saber R, et al. Cell Rep 2014; 9:591–604. [DOI] [PMC free article] [PubMed]
- Nakasone Y, Fujimoto M, Matsushita T, et al. Am J Pathol 2012; 180:365–374. [DOI] [PubMed]
- Kitamura T, Qian BZ, Soong D, et al. J Exp Med 2015; 212:1043–1059. [DOI] [PMC free article] [PubMed]
- Al-Mehdi AB, Tozawa K, Fisher AB, et al. Nat Med 2000; 6:100–102. [DOI] [PubMed]