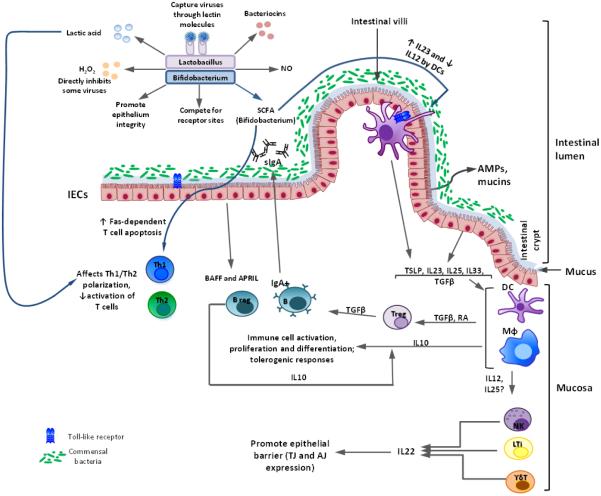
Figure 1. Interactions between probiotics of Lactobacillus and Bifidobacterium genera and the immune system modelled in vitro and in vivo (in mice and Gn pigs).
In the intestinal lumen, Lactobacillus/Bifidobacterium strains (Lacto/Bifido) inhibit some viruses directly by producing lactic acid, H2O2, bacteriocins, and other inhibitory agents; (2) Lacto/Bifido also preserve the integrity of the epithelium and compete with pathogens for Intestinal epithelial cell (IEC) receptors; (3) Lacto capture viruses by lectin-mediated binding to viral glycoproteins to prevent infection; (4) Lacto-derived nitric oxide (NO) has microbicidal and tumoricidal activities; (5) short chain fatty acids (SCFA) produced by Bifido block dendritic cell (DC) development; induce Fas-mediated T cell apoptosis; decrease IL-12 expression, but increase IL-23 production by DCs.
Intestinal epithelial cells (IECs) secrete mucins and antimicrobial peptides (AMPs) in response to the commensal microbiota/probiotics, regulating microbial replication and interaction with intestinal mucosa. IECs produce BAFF and APRIL factors, stimulating activated B (plasma) cells to produce secretory IgA (sIgA) that further limits microbial interaction with the epithelium. Under homeostatic conditions, commensal microbiota/probiotics stimulate the secretion of cytokines [including thymus stimulating lymphoprotein (TSLP), IL-33, IL-23, IL-25, and TGFβ] by IECs that promote development of antigen presenting cells [macrophages (Mφ) and DCs]. Antigen presenting cells (APCs) induce regulatory T (Treg) cell generation through TGFβ- and retinoic acid (RA)-dependent mechanisms. APC and Treg derived TGFβ and IL-10, maintain the anti-inflammatory nature of the intestine by inhibiting/reducing effector responses. Intestinal innate lymphoid cells (ILCs), including natural killer (NK) cells, lymphoid tissue inducer (LTi) cells, and γδ T cells, produce IL-22 that regulates expression of tight and adherent junction (TJ and AJ) proteins by IECs, regulating intestinal barrier function.