Abstract
Background
Compare the effectiveness and cost of stepped care trauma-focused cognitive behavioral therapy (SC-TF-CBT), a new service delivery method designed to address treatment barriers, to standard TF-CBT among young children who were experiencing posttraumatic stress symptoms (PTSS).
Methods
A total of 53 children (ages 3-7 years) who were experiencing PTSS were randomly assigned (2:1) to receive SC-TF-CBT or TF-CBT. Assessments by a blinded evaluator occurred at screening/baseline, after Step One for SC-TF-CBT, post-treatment, and 3-month follow-up. Trial registration: ClinicalTrials.gov: https://www.clinicaltrials.gov/ct2/show/NCT01603563
Results
There were comparable improvements over time in PTSS and secondary outcomes in both conditions. Non-inferiority of SC-TF-CBT compared to TF-CBT was supported for the primary outcome of PTSS, and the secondary outcomes of severity and internalizing symptoms, but not for externalizing symptoms. There were no statistical differences in comparisons of changes over time from pre- to post-treatment and pre- to 3 month follow-up for PTSD diagnostic status, treatment response or remission. Parent satisfaction was high for both conditions. Costs were 51.3% lower for children in SC-TF-CBT compared to TF-CBT.
Conclusions
Although future research is needed, preliminary evidence suggests that SC-TF-CBT is comparable to TF-CBT, and delivery costs are significantly less than standard care. SC-TF-CBT may be a viable service delivery system to address treatment barriers.
Keywords: Stepped care, TF-CBT, young children, PTSD, trauma
Introduction
Young children are exposed to a wide variety of potentially traumatic events (e.g., physical and sexual abuse, witnessing domestic violence and accidents), with some studies documenting trauma exposure as high as 70% (Roberts, Ferguson, & Crusto, 2013; Roberts, Huang, Crusto, & Kaufman, 2014). Approximately 16-33% of children exposed to traumatic events will develop posttraumatic stress disorder (PTSD) (Alisic et al., 2014), although these estimates may vary based on location and type of trauma. Without effective treatment, childhood PTSD and associated deleterious outcomes persist (Scheeringa, Zeanah, Myers, & Putnam, 2005). There are effective psychotherapies for young children after trauma, but these treatments require weekly therapist-led sessions ranging from three months to one year (Cohen, Deblinger, Mannarino, & Steer, 2004; Lieberman, Ghosh Ippen, & Van Horn, 2006; Scheeringa, Weems, Cohen, Amaya-Jackson, & Guthrie, 2011). For some families, the time commitment, costs, stigma, and transportation needed for in-office therapy meetings are treatment barriers that limit access to care (Bringewatt & Gershoff, 2010). Further, some parents may not seek treatment for their child due to wanting to solve the problem independently (Thurston & Phares, 2008). Newer service delivery models are needed to address treatment barriers and provide alternative treatments that are accessible, efficient, affordable, and effective.
Stepped care models are designed to provide first-line interventions that are easily accessible, lower cost, convenient for patients, and require less therapist time than standard treatment methods, such as weekly in-office therapist-directed treatment. Importantly, the first step must provide active mechanisms such that a substantial number of patients will improve. These models include a priori criteria for defining early treatment response after each step which is used to guide subsequent treatment. Stepped care models reserve resources, such as therapist time and costs, for those needing more intensive treatment (Bower & Gilbody, 2005).
Trauma-focused cognitive behavioral therapy (TF-CBT) is a well-established evidence-based treatment for children ages 3-18 (Silverman et al., 2008) that is widely disseminated (Cohen & Mannarino, 2008;). TF-CBT is a therapist-led treatment requiring weekly sessions with the parent and child for three to six months. Recently, TF-CBT was developed into a stepped care model called Stepped Care TF-CBT (see online supplementary Figure S1) in which the first step, Step One, is a parent-led treatment where the majority of the treatment is provided at home by the parent. The at-home treatment is supported with three in-office sessions with the therapist, phone support, and web-based psychosocial information and video demonstrations (Salloum, Scheeringa, Cohen, & Storch, 2013). An a priori early responder status criterion after Step One is used to indicate if the child needs more treatment or can end treatment (Salloum, Scheeringa, Cohen & Storch, 2015). Children who need more treatment step up to Step Two, which consists of nine weekly TF-CBT therapist-led sessions. Children ending treatment after Step One enter the maintenance phase for six weeks where they continue parent-child meetings and practice skills they learned (Salloum, Scheeringa, et al., 2013). A parent-led treatment may be well-suited for young children as this age group is still very dependent on the parent and it allows the parent an opportunity to help solve the child's problems.
An open trial with nine parents and children who participated in SC-TF-CBT found that five of nine responded to Step One, parents were satisfied with the treatment, and costs of delivering the treatment were low (Salloum, Robst, et al., 2014). The current study addressed the next step in the development of SC-TF-CBT in that it compares the effectiveness and costs of SC-TF-CBT relative to standard TF-CBT among young children ages 3-7. We hypothesized that SC-TF-CBT would be comparable over time to TF-CBT in terms of child posttraumatic stress symptoms (PTSS: primary outcome), PTSS severity, internalizing and externalizing symptoms (secondary outcomes), parental expectation and credibility of treatment, and parent satisfaction, and that SC-TF-CBT would cost significantly less than TF-CBT.
Methods
Participants
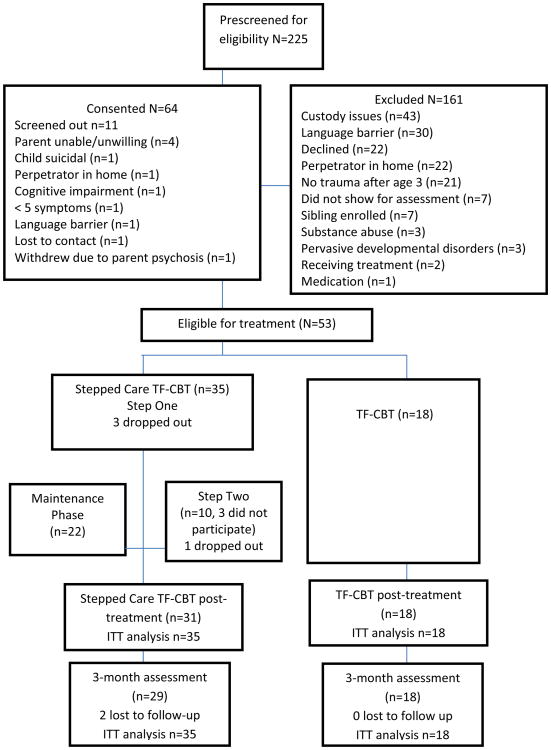
Participants were recruited consecutively between May 2012 and August 2014 from a community mental health non-profit agency in an urban area where the study treatment occurred. Participants were recruited via phone when the parent called the agency seeking services. Referrals came from community sources (e.g., child welfare organizations, victim services, schools, hospitals, mental health clinics). These referral sources were the typical referrals to the agency, and most sources were provided with information about the study. Fifty-three young children (ages 3-7; M=5.04, SD=1.49) and their parent/guardian (ages 22-57; M=32.81, SD=8.42) were enrolled. Inclusion criteria included: (a) Child experienced ≥1 traumatic event after the age of 36 months; (b) child had ≥5 DSM-IV PTSD symptoms, with at least one symptom in re-experiencing or avoidance; (c) child was between the ages of 3-7 years. Exclusion criteria were: (a) any condition that limited the child's or caregiver's ability to comprehend the treatment or follow instructions (e.g., psychosis, mental retardation, or autism); (b) caregiver substance use disorder within past three months; (c) child or caregiver suicidality; (d) child or caregiver not fluent in English; (e) if child was on medication, the regimen was not stable for at least four weeks before enrollment; and (f) the caregiver was the perpetrator or the perpetrator was living in the same residence as the child. See Figure 1 for patient flow of enrollment and retention, and Table 1 for demographic information.
Figure 1. Consolidated standards of reporting trials flow diagram of study (N=53).
Table 1. Demographics and Characteristics by Condition (N=53).
| Characteristic | SC-TF-CBT (n=35) n (%) |
TF-CBT (n=18) n (%) |
p-valuea |
|---|---|---|---|
| Child gender | .59 | ||
| Male | 19 (54.3) | 8 (44.4) | |
| Female | 16 (45.7) | 10 (55.6) | |
| Child ethnicity | .38 | ||
| Hispanic or Latino | 14 (40) | 10 (55.6) | |
| Child race | .15 | ||
| American Indian/Alaskan Native | 1 (2.9) | 0 (0) | |
| African American | 6 (17.1) | 8 (44.4) | |
| White | 25 (71.4) | 9 (50) | |
| Mixed Race | 3 (8.6) | 1 (5.6) | |
| Child index traumab | .33 | ||
| Sexual abuse | 11 (31.4) | 7 (38.9) | |
| Domestic violence | 12 (34.3) | 6 (33.3) | |
| Death/grief | 4 (11.5) | 2 (11.1) | |
| Physical abuse | 1 (2.9) | 1 (5.6) | |
| Accidents | 3 (8.6) | 0 (0.0) | |
| Community violence | 1 (2.9) | 0 (0.0) | |
| Crime | 1 (2.9) | 0 (0.0) | |
| Witnessed parent arrest | 1 (2.9) | 0 (0.0) | |
| Removal from parent/home | 0 (0.0) | 2 (11.1) | |
| Illness/medical | 1 (2.9) | 0 (0.0) | |
| Parent/Guardian relationship | .16 | ||
| Biological mother | 30 (85.7) | 16 (88.9) | |
| Biological father | 3 (8.6) | 0 (0) | |
| Grandmother | 2 (5.7) | 0 (0) | |
| Great aunt | 0 (0) | 1 (5.6) | |
| Aunt | 0 (0) | 1 (5.6) | |
| Parent/Guardian ethnicity | .24 | ||
| Hispanic/Latino | 11 (31.4) | 9 (50) | |
| Parent/Guardian race | .03* | ||
| American Indian/Alaskan Native | 0 (0) | 2 (11.1) | |
| African American | 6 (17.1) | 6 (33.3) | |
| White | 29 (82.9) | 10 (55.6) | |
| Household incomec | .95 | ||
| $0 – 9,999 | 5 (14.3) | 7 (38.9) | |
| $10,000 – 24,999 | 9 (25.7) | 5 (27.8) | |
| $25,000 – 34,999 | 11 (31.4) | 1 (5.6) | |
| $35,000 – 49,999 | 4 (11.4) | 0 (0) | |
| $50,000 + | 6 (17.1) | 5 (27.8) | |
| Parent/Guardian employed | 22 (62.9) | 10 (55.6) | .77 |
| Parent/Guardian in treatment | 7 (20) | 5 (27.8) | .73 |
| Parent/Guardian with PTSD | 15 (42.9) | 13 (72.2) | .04* |
| Parent/Guardian with MDD | 6 (17.2) | 4 (22.2) | .72 |
| Parent/Guardian age, y, M(SD) | 32.80 (7.58) | 33.39 (9.99) | .81 |
| Child's age, y, M(SD) | 4.94 (1.47) | 5.50 (1.25) | .18 |
Note.
Non-parametric tests were used for nominal level data; thus no test statistic is provided.
T-tests were used for mean differences in age measured in years (y) for parents (t(51)=-.24) and children (t(51)=-1.37).
p<.05
Type of trauma was collapsed into non/interpersonal trauma (e.g., sexual abuse, domestic violence, physical abuse and kidnapping).
Income was collapsed into < or $35,000 > for the significance analysis.
Procedures
This study was approved by the University of South Florida Institutional Review Board. Written informed consent was obtained from caregivers; children age 7 provided written assent and younger children were provided a brief verbal explanation about the study and assent was waived. The independent evaluator (IE), a master level clinician trained by the first, fourth, and last authors, and blinded to treatment conditions, administered the screening/baseline assessments. Child-caregiver dyads who met criteria were randomly assigned to one of the study conditions using a 2 (SC-TF-CBT) to 1 (TF-CBT) ratio. A 2:1 ratio was used since SC-TF-CBT is in the developmental phase and there are numerous outcome studies on TF-CBT (Cohen et al., 2004; Deblinger, Mannarino, Cohen, Runyon, & Steer, 2011). A computerized randomized block procedure generated by the second author using Splus was used by the Project Coordinator to assign cases to a condition. After randomization, parents completed the Expectancy Rating Form (ERF; Borkovec & Nau, 1972) before being scheduled for therapy the following week. Caregivers assigned to SC-TF-CBT were asked if they had access to the internet (91.67% had access). Parents who did not have access were provided printed psychoeducational information from the National Child Traumatic Stress Network (NCTSN) website.
There were four assessment periods, all conducted by the IE: screening/baseline, after Step One, post-treatment, and 3-month follow-up. Caregivers were provided compensation for their participation in assessments ($25 for baseline, a lower amount to minimize inducement to participate, $50 for each remaining assessments), but not for therapy. This trial was registered in ClinicalTrials.gov (see https://www.clinicaltrials.gov/ct2/show/NCT01603563).
Treatment
SC-TF-CBT
Step One consisted of three in-office therapist-led sessions (60 minutes), 11 parent-child meetings at-home over six weeks using an empirically-informed workbook that was based on the Preschool PTSD Treatment manual (Salloum, Scheeringa, Cohen & Amaya-Jackson, 2009), weekly brief phone support, psychoeducation information from NCTSN website, and a website with video demonstrations of relaxation exercises and imaginal and in vivo exposures. For a complete description of Step One see Salloum, Scheeringa, et al., 2013. If the child responded to Step One, the child proceeded to the maintenance phase for six weeks to practice the skills learned. Early responder status criteria was defined as ≤3 PTSS, or a Trauma Symptom Checklist for Young Children (Briere, 2005) PTS score of ≤39, and an IE Clinical Global Impression-Improvement (CGI-Improvement; Guy, 1976) rating of 3 (improved), 2 (much improved), or 1 (free of symptoms)(Salloum et al., 2015). If the child did not respond, s/he stepped up to Step Two which consisted of nine TF-CBT sessions.
Standard TF-CBT
Standard TF-CBT, 12 (90-minute) in-office therapist-led sessions, was provided to the child with active parent involvement. Treatment consisted of the core components of TF-CBT (e.g., psychoeducation; parenting skills; relaxation; affective expression and modulation; cognitive coping and processing; trauma narrative; conjoint child-parent sessions; and enhancing future safety and development)(Cohen, Mannarino, & Deblinger, 2006).
Treatment Fidelity and Number of Sessions
Four master-level mental health therapists employed by a community agency provided therapy. The average experience post-masters was 4 years, 9 months (range 5 months to 14 years, 10 months). Therapists provided both treatments and completed treatment fidelity checklists for each session. Therapy session audio files were reviewed (e.g., 41.03% for SC-TF-CBT and 31.71% for TF-CBT) for inter-rater agreement by the project coordinator (PC); inter-rater agreement was .93 (p<.001) for SC-TF-CBT and .95 (p<.001) for TF-CBT. The PC was a master level licensed professional who was not blinded to treatment. The average number of therapist-led in-office therapy sessions was 2.6 (.98) for Step One, 6.3 (4.62) for Step Two, and 11.06 (2.6) for TF-CBT. Three parents who qualified for Step Two chose not to participate, but continued with the assessments. One of these parents indicated that she did not think more treatment was needed as the child was being reunited with her biological parent. One parent became homeless, went to a shelter and did not have transportation. The reason for non-participation of the third parent was unknown. The average number of parent-child meetings in Step One was 7.91 (4.02).
Measures
Primary Outcome Measure
Trauma Symptom Checklist for Young Children (TSCYC; Briere, 2005) measures the frequency of children's trauma symptoms. The 27-item posttraumatic stress (PTS) subscale was used for the present study (total score range=27-108, ≥40 in the clinical range; current sample α=.92; administered at all four assessments periods).
Secondary Outcome Measures
Clinical Global Impression-Severity (CGI-Severity; National Institute of Mental Health, 1985) is a 1-item 7-point Likert scale ranging from 0 (no illness) to 6 (extremely severe symptoms/completely nonfunctional) to measure symptom severity. This rating was completed by the IE after each assessment period. The last author and IE, both blind to study condition, reviewed the CGI-Severity scores together for agreement. Inter-rater reliability between an independent rater and the IE was good (Kappa=.75, p < .001).
Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000, 2001) is a widely used, psychometrically sound parent-report of children's emotional and behavioral problems. The current study utilized the 1½ to 5-year old and 6 to18-year old versions. T-scores for internalizing and externalizing behavior problems were used. This measure was administered at baseline, post and follow-up assessments.
Diagnostic Assessment and Improvement
Diagnostic Infant and Preschool Assessment (DIPA; Scheeringa & Haslett, 2010) is a semi-structured clinical interview with the parent/guardian to assess for mental health disorders in young children. The PTSD module was used to determine inclusion and PTSD diagnostic status (e.g., DSM-IV PTSD and an alternative algorithm for PTSD (PTSD-AA) for young children) (Scheeringa, Zeanah, Myers, & Putnam, 2003). For the PTSD module, 29.25% of interviews were reviewed by a psychology doctoral student and inter-rater reliability was excellent (Kappa=.93, p < .001). This measure was administered at all assessment periods.
CGI-Improvement (Guy, 1976) is a 1-item 8-point Likert scale to measure overall symptom improvement with scores ranging from 1 (free of symptoms) to 8 (very much worse). An IE rating of 1, 2, or 3 was used as treatment response, and a rating of 1 was used as remission. The IE score was reviewed by the last author (who was blinded to treatment) and a consensus rating was obtained. This rating was completed after Step One, and at post and follow-up assessments.
Treatment credibility and satisfaction
The ERF (Borkovec & Nau, 1972) is a parent self-report, 4-item, 10-point Likert scale (1=low to 10=high) assessing the parent's expectations regarding the success and credibility of the treatment at baseline. Scores were averaged such that the total score ranged from 0 to 10. A fifth item that measured on a scale of 0 to 100% how much the parent expected the child's symptoms to improve by the end of the treatment was included (current sample α=.84).
Client Satisfaction Questionnaire (CSQ; Nguyen, Attkisson, & Stegner, 1983) has 8-items on a 4-point Likert scale to measure parent's satisfaction with the treatment. Responses range from 1 (low) to 4 (high) with higher scores indicating greater treatment satisfaction (range 8 to 32; current sample α=.91; administered at post-treatment).
Parenting measure
Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version (SCID-RV; First, Spitzer, Miriam, & Williams, 2002) is a structured, clinician-administered interview for adult DSM-IV criteria disorder diagnosis. The SCID-RV was administered only at baseline to screen for exclusion criteria, parent PTSD and depression.
Cost measures
The Therapist/Patient Time Tracking System (TTTS; Salloum, Robst, et al., 2013) records, by the therapist, the amount of time that therapist and client spend throughout treatment, including face-to-face therapy sessions, phone calls, documenting treatment notes, and client homework.
Cost Characteristics Information (CCI; Salloum, Robst, et al., 2013) estimates indirect treatment costs, such as insurance co-payments/deductibles or cost of treatment, gas, and compensation from missing work or therapy appointments.
Data analyses
In general, we conducted two analyses, ‘difference tests’ and non-inferiority tests. Difference tests were conducted using linear mixed-effects models (for continuous outcomes) or generalized linear mixed-effects models (for non-continuous outcome) to accommodate correlations among repeated measures. Included in the model were treatment status, time, and treatment by time interaction. The presence of a non-significant interaction would suggest that the children in the two conditions changed at comparable rates. For non-inferiority tests, we followed the recommendation of Greene, Morland, Durkalski, and Frueh (2008) and concluded non-inferiority if the SC-TF-CBT values were within at least 80% of TF-CBT. Since there were only a few incomplete cases and drop outs, intent-to-treat (ITT) analysis based on multiple imputation method was conducted for the child primary and secondary outcomes and for the diagnostic and improvement status ratings. Ten imputations were generated at item level, and the aforementioned analyses were repeated on these imputed data sets and results then were aggregated (Schafer, 1997). Since we had less than 10% missing cases, 10 imputations would carry a 99% efficiency and thus were adequate (Rubin, 1987). All four participants who dropped out were included in the ITT analysis (two had complete data for all time points that was used; two cases had missing post-treatment and follow-up data which were imputed). Follow-up data were imputed for the two lost-to-follow-up cases. Since the ITT and completer results were comparable, we reported the ITT results. From the original design, we had anticipated that the power would fall between .29 (small non-inferiority margin) to .44 (medium non-inferiority margin). For the actual sample size, power ranged from .34 (small non-inferiority margin) to .52 (medium non-inferiority margin). While multiple comparisons were unavoidable, we opted not to impose any corrections due to the piloting/exploratory nature of the study. The analyses were conducted using Splus for generalized linear models and SPSS for multiple imputation.
Costs were analyzed instead of cost effectiveness based on the findings below that children receiving SC-TF-CBT improved at the same rate as children receiving TF-CBT. Cost effectiveness ratios are based on a difference in treatment efficacy, and in the absence of such differences can be reduced to a comparison of costs. Statistical significance of cost differences was assessed using SAS Proc Genmod with a log-link to account for the non-normal distribution of costs. Based on the expert panel recommendations of Gold, Seigel, Russell, and Weinstein (1996), costs are examined from a societal perspective, meaning the costs to the health care system and the patient/parents are included. Treatment is typically paid for by private or public insurers in the US healthcare system; thus, we present the cost analysis under the scenario in which payments are by insurers (i.e., payer direct cost). Payer direct cost consisted of the cost of a session and phone calls paid by a third party (e.g., Medicaid rate). Social costs also include the value of patient and (uncompensated) provider time. Patient indirect cost included indirect cost of participating in treatment including, cost of travel and lost wages from time spent in treatment, driving to and from treatment, waiting for treatment sessions, or doing homework. Provider indirect costs included time not reimbursed, including time preparing and documenting sessions. Total cost includes all direct and indirect costs. Masters level therapist time was valued at the Florida Medicaid payment rate of $18.33 per quarter hour. Patient/parent travel costs to and from sessions was 23 cents per mile (U.S. Department of Labor, 2011). Parent time was valued at the median hourly wage ($18.06 for college graduates and $11.79 for high school graduates) (Internal Revenue Services, 2011). The sample size provides marginal power (.77 with α=.05) to detect large effect sizes (Cohen's d=.8) using a two-tailed test.
Results
Baseline equivalence between conditions indicated that there were significant differences for parent/guardian race and PTSD diagnosis status (see Table 1). However, since these two variables were not significantly associated with outcome variables, they were not included in the model. There were no significant differences in demographics, primary and secondary outcome measures, and ERF ratings between completers (n=49) and drop outs (n=4: 11.4% in SC-TF-CBT due to transportation, scheduling difficulty and medical issues). The average number of traumatic events was 2.75 (±1.22), which was not different by condition, t(51) = -.33, p = .741. In SC-TF-CBT, 22 responded to Step One (see Figure 1). One parent in Step One was court-ordered to therapist-directed treatment due to possible on-going domestic violence. Of Step One participants, the response rate was 71% (22/31; ITT 22/35, 63%), and responder status criteria was maintained at post and follow-up assessment.
Primary and secondary outcomes
Table 2 provides descriptive data. Online supplementary Table S1 summarizes the results from both difference and non-inferiority tests. With respect to the primary outcome, TSCYC-PTS total, and secondary outcomes, CGI-Severity, CBCL Internalizing and Externalizing T scores, results from difference tests showed that participants in SC-TF-CBT changed at comparable rates, if not better, in comparison to those in standard TF-CBT (p-values ranged between .023 to .597). SC-TF-CBT was not inferior to standard TF-CBT on all variables except for externalizing T scores (p = .09).
Table 2. ITT Means and SD for Primary and Secondary Outcomes by Condition (SC-TF-CBT n=35; TF-CBT n=18).
| Variable | SC-TF-CBT | TF-CBT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Baseline M(SD) | Post M(SD) | FU M(SD) | Post ES d | FU ES d | Baseline M(SD) | Post M(SD) | FU M(SD) | Post ES d | FU ES d | |
| TSCYC-PTS | 56.29 (13.91) | 37.19 (10.19) | 35.94 (11.59) | 1.57 | 1.59 | 52.61 (15.84) | 38.11 (9.89) | 34.94 (8.53) | 1.10 | 1.39 |
| CGI-S | 4.26 (0.85) | 1.10 (1.21) | 1.07 (1.28) | 3.02 | 2.94 | 3.83 (1.04) | 1.44 (1.20) | 1.17 (0.99) | 2.13 | 2.62 |
| Internalizing T score | 66.86 (8.06) | 51.08 (12.31) | 50.08 (13.38) | 1.52 | 1.52 | 63.06 (11.00) | 50.61 (11.85) | 48.61 (13.61) | 1.09 | 1.17 |
| Externalizing T score | 64.94 (11.00) | 51.21 (12.31) | 50.71 (14.70) | 1.18 | 1.10 | 66.28 (10.77) | 54.28 (12.84) | 54.11 (15.62) | 1.01 | 0.91 |
Note. ES= effect size, d = Cohen's d
Diagnostic status and improvement (ITT)
For the PTSD-DSM-IV diagnostic status, there was no statistical difference at post-treatment between SC-TF-CBT (48.6% at baseline to 0%) and TF-CBT (33.3% at baseline to 0%), p = .443 (χ2(1) = 0.59). Similarly, there was no significant difference in PTSD-DSM-IV criteria at follow-up (SC-TF-CBT = 8.6% vs. TF-CBT = 0%), p =.861 (χ2(1) = 0.03). For the PTSD-AA, there were no significant differences at post-treatment between SC-TF-CBT (91.4% baseline to 14.3%) and TF-CBT (88.9% at baseline to 5.6%), p = .866 (χ2(1) = 0.03), and the differences at follow-up were not significant (SC-TF-CBT = 14.3% vs. TF-CBT = 5.6%, p = .866, χ2(1) = 0.03).
There were no statistical differences in treatment response between SC-TF-CBT and TF-CBT at post-treatment (94.3% vs. 100%, p = .785, χ2(1) = 0.07) and follow-up (91.4% vs. 94.4%, p = .694, χ2(1) = 0.15), respectively. Similarly, there were no statistical differences in remission between SC-TF-CBT and TF-CBT at post-treatment (42.9% vs. 27.8%, p = .439, χ2(1) = 0.60) and follow-up (45.7% vs. 33.3%, p = .567, χ2(1) = 0.33).
Treatment credibility and satisfaction
There was no significant difference in parent ERF ratings between SC-TF-CBT (M=9.19, SD=88) and TF-CBT (M=9.14, SD=1.21), p = 0.563. Similarly, on the rating of parent expectation of improvement, there was no significant difference between conditions (M=81.11, SD = 19.06 vs M=86.57, SD=12.11, SC-TF-CBT and TF-CBT, respectively, p = 0.443).
Satisfaction scores were high for both conditions (SC-TF-CBT = 30.03±2.74; TF-CBT= 29.50±4.02). There were no significant differences on CSQ scores between the two conditions (see Table S1).
Cost results
Costs were 51.3% lower (χ2(52)=36.3, p < .0001) for children in SC-TF-CBT (n=35, M=$953.17, SD=645.43) compared to standard TF-CBT (n=18, M=$1,957.19, SD=64.38). Direct and indirect costs to parents/patients and providers were significantly lower for children in SC-TF-CBT. Patient/parent indirect costs were lower for SC-TF-CBT due to the overall lower time requirements, particularly for office visits (see Table 3).
Table 3. Differential Costs Between SC-TF-CBT and Standard TF-CBT (N=53).
| Cost | SC-TF-CBT | TF-CBT | Effect size | Wald | p value |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | (Cohen's d) | Chi square | ||
| Payer direct cost | $466.62 (354.30) | $1,057.03 (257.54) | 1.38 | 36.3 | <.0001 |
| Patient indirect cost | $238.30 (154.38) | $436.82 (220.00) | 0.99 | 15.0 | <.0001 |
| Provider indirect cost | $248.24 (201.45) | $463.34 (116.20) | 1.00 | 15.5 | <.0001 |
| Total cost | $953.17 (645.43) | $1,957.19 (564.38) | 1.29 | 30.5 | <.0001 |
Note. The Wald Chi square and p values are from generalized linear models with a log-link to account for non-normal distributions.
Discussion
There has been considerable research on the effectiveness of TF-CBT (Cohen et al., 2004; Deblinger et al., 2011; Mannarino, Cohen, Deblinger, Runyon, & Steer, 2012); however, innovative service delivery approaches to provide TF-CBT are limited. Results of this trial comparing SC-TF-CBT to TF-CBT are encouraging. Outcomes in both treatments changed at comparable rates and SC-TF-CBT was not inferior to TF-CBT on PTSS, PTSS severity and internalizing symptoms, but not for externalizing symptoms. There were no significant differences in changes in diagnostic status, treatment response and remission between conditions. Importantly, there were no significant differences by condition in parents' perceived treatment credibility, anticipated improvements and treatment satisfaction. SC-TF-CBT was significantly less costly than TF-CBT.
The majority of children in Step One responded to the parent-led therapist-assisted treatment and did not require further treatment. This high early response rate to a parent-led treatment potentially addresses the treatment barrier of parents wanting to help their children. Step One may be more convenient for parents as it limits the number of times parents have to attend in-office visits. Research is needed to identify characteristics that may determine who is likely to respond to Step One and who may need to be assigned directly to standard TF-CBT. Matching children at baseline to the best level of care may minimize dropouts, as having parents complete Step One without the child responding may contribute to parents dropping out and not proceeding to Step Two.
SC-TF-CBT and TF-CBT both had mean externalizing T scores below the clinical range at post-treatment, large effect sizes, and improvements were comparable across the two conditions. However, the non-inferiority test, which is more stringent than difference tests, did not suggest that SC-TF-CBT was at least 80% as effective as TF-CBT in reducing externalizing behaviors. Additional strategies for addressing externalizing symptoms in Step One for children with high externalizing scores may lead to non-inferiority between SC-TF-CBT and TF-CBT. Research with the inclusion of supplementary behavioral strategies in Step One and larger samples to test non-inferiority of externalizing symptoms is needed.
In the current study, cost was the main treatment barrier assessed, and the potential for over a 50% savings is promising. The cost to patients in SC-TF-CBT was 1.8 times less than TF-CBT and the payer costs were 2.27 times lower in SC-TF-CBT than TF-CBT. Beyond these encouraging numbers, the meaning of this type of improvement to standard care may have several implications for practice and policy. First, more parents may have access to treatment for their children. Second, therapy would be more efficient with early responders requiring fewer weeks in therapy and more resources would be available for children needing more intensive care. Third, the therapist role in Step One is one of an assistant rather than a direct provider. Fourth, payers and policy makers may require large child serving systems and agencies and/or private therapists to provide stepped care approaches such as SC-TF-CBT.
There are notable study limitations. First, the small sample size is a limitation and does not allow for more advanced analyses. Future trials on SC-TF-CBT need larger, more diverse samples, including non-English speaking participants, that allow for moderators of treatment to be tested and identification of candidate baseline characteristics that could be used to match children to the appropriate level of care prior to treatment. Testing differing outcomes, satisfaction, and attrition by race, ethnicity and/or cultural practices, as well as conducting qualitative studies with therapists and patients to learn about possible cultural modifications for specific groups, are needed for the future development of SC-TF-CBT. Second, research with a longer follow-up is needed to ensure that treatment gains are maintained for children who receive parent-led therapist-assisted treatment compared to therapist-led treatment. Third, cost data was limited in that other mental health and health services were not collected. Future research will need to address these costs limitations.
Conclusion
The current study provides preliminary support for the effectiveness and cost of SC-TF-CBT relative to standard TF-CBT among young children. The parent-led therapist-assisted treatment may be a viable option for many parents and children. However, research is needed to develop an algorithm that matches children at baseline to either weekly therapist-directed treatment or to the parent-led therapist-assisted treatment so that treatment for potential non-responders of Step One is not delayed. We highlight the need for additional research on SC-TF-CBT as this service delivery model may be a viable alternative for many parents seeking an accessible, efficient, affordable, and effective trauma-focused treatment.
Supplementary Material
Figure S1. Stepped Care Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) Model
Table S1 Difference Test and Non-inferiority Test Results for Primary and Secondary Outcomes
Key Points.
TF-CBT is a well-established treatment, but alternative delivery systems to address treatment barriers are limited; thus Stepped Care TF-CBT, with a parent-led therapist-assisted treatment as a first step and standard TF-CBT for the second step, was developed.
There were comparable improvements over time in PTSS, symptom severity, internalizing and externalizing symptoms, PTSD diagnostic status, remission and response for Stepped Care and standard TF-CBT.
SC-TF-CBT was not inferior to TF-CBT on PTSS, severity, internalizing symptoms, parent credibility and satisfaction, but non-inferiority for externalizing symptoms was not supported.
Costs were 51.3% lower in SC-TF-CBT compared to standard TF-CBT. SC-TF-CBT offers a promising new service delivery system, but more research is needed.
Acknowledgments
The study was supported by A National Institute of Mental Health award assigned to A.S. (R34MH092373). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The Crisis Center of Tampa Bay, Victoria Swaidan, B.A. and Brittany Kugler, MSW, M.A. at the University of South Florida, and David Tolin at The Institute of Living, Yale University School of Medicine are gratefully acknowledged. Authors W.W. and J.R. served as statistical experts for this research. Apart from funding from the National Institute of Mental Health (NIMH), A.S. also received funding from the Agency for Healthcare Research and Quality, Eckerd Child Welfare, and the Crisis Center of Tampa Bay as well as royalties from Taylor and Francis, and Centering Corporation. A grant by the NIMH was assigned to W.W. Author J.R. received funding from NIMH and Florida Agency for Health Care Administration. T.K.M. received research support from the International OCD Foundation, National Institutes of Health, Florida Mental Health Institute, Otsuka Pharmaceuticals, Pfizer, Inc., F. Hoffmann-La Roche Ltd, Shire Pharmaceuticals, Neurocrine Biosciences, Inc., and Psyadon Pharmaceuticals. T.K.M received textbook honorarium from Lawrence Erlbaum. The author was on the Medical Advisory Board for Tourette Syndrome Association. The author is on the Scientific Advisory Board for IOCDF. M.S.S. is supported by funding from the Administration on Children, Youth, & Families. J.A.C. received funding from NIMH, National Institute for Child Health and Human Development, and Substance Abuse and Mental Health Services Administration. The author received book royalties from Guilford Press. E.A.S. was supported by funding from the National Institutes of Health, Center for Disease Control, Agency for Healthcare Research and Quality, International OCD Foundation, All Children's Hospital Research Foundation, and Janssen Pharmaceuticals. The author was also supported by a research grant from All Children's Hospital Guild Endowed Chair. The author received textbook honorarium from Springer publishers, American Psychological Association, Wiley, and Lawrence Erlbaum. The author has been a consultant/member for Rogers Memorial Hospital, Prophase, Inc., Speaker's Bureau Scientific, and the Advisory Board for the International OCD Foundation.
Footnotes
Conflict of interest statement: See Acknowledgements for disclosures.
Supporting information: Additional Supporting Information may be found in the online version of this article:
References
- Achenbach TM, Rescorla LA. Manual for ASEBA preschool-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, Smid GE. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. The British Journal of Psychiatry. 2014;204:335–340. doi: 10.1192/bjp.bp.113.131227. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. [Google Scholar]
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. The British Journal of Psychiatry. 2005;186:11–17. doi: 10.1192/bjp.186.1.11. [DOI] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Checklist for Young Children: Professional manual. Lutz, FL: Psychological Assessment Resources, Inc; 2005. [Google Scholar]
- Bringewatt EH, Gershoff ET. Falling through the cracks: Gaps and barriers in the mental health system for America's disadvantaged children. Children and Youth Services Review. 2010;32(10):1291–1299. doi: 10.1016/j.childyouth.2010.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Mannarino AP. Disseminating and Implementing Trauma-focused CBT in community settings. Trauma, Violence and Abuse. 2008;9(4):214–226. doi: 10.1177/1524838008324336. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York, N.Y.: The Guilford Press; 2006. [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma-focused cognitive behavioral therapy for children: impact of the trauma narrative and treatment length. Depression and Anxiety. 2011;28(1):67–75. doi: 10.1002/da.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Miriam G, Williams JBW. Structured Clinical Interview for DSM-IV-TR axis I disorders, research version, patient edition with Psychotic Screen. New York: New York State Psychiatric Institute Biometrics Research; 2002. [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- Greene CJ, Morland LA, Durkalski VL, Frueh BC. Noninferiority and equivalence designs: issues and implications for mental health research. Journal of Traumatic Stress. 2008;21(5):433–439. doi: 10.1002/jts.20367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology. Washington, DC: US Department of Health, Education, and Welfare; 1976. [Google Scholar]
- Lieberman AF, Ghosh Ippen C, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(8):913–918. doi: 10.1097/01.chi.0000222784.03735.92. [DOI] [PubMed] [Google Scholar]
- Mannarino AP, Cohen JA, Deblinger E, Runyon MK, Steer RA. Trauma-focused cognitive-behavioral therapy for children: sustained impact of treatment 6 and 12 months later. Child Maltreatment. 2012;17(3):231–241. doi: 10.1177/1077559512451787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. Clinical Global Impressions Scale. Psychopharmacology Bulletin. 1985;21:839–843. [Google Scholar]
- Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Evaluation and Program Planning. 1983;6(3-4):299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- Roberts YH, Ferguson M, Crusto CA. Exposure to traumatic events and health-related quality of life in preschool-aged children. Quality of Life Research. 2013;22(8):2159–2168. doi: 10.1007/s11136-012-0330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts YH, Huang CY, Crusto CA, Kaufman JS. Health, emergency department use, and early identification of young children exposed to trauma. Journal of Emergency Medicine. 2014;46(5):719–724. doi: 10.1016/j.jemermed.2013.11.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 1987. [Google Scholar]
- Salloum A, Robst J, Scheeringa MS, Cohen JA, Wang W, Murphy TK, et al. Storch EA. Step one within Stepped Care Trauma-Focused Cognitive Behavioral Therapy for young children: A pilot study. Child Psychiatry and Human Development. 2014;45:65–77. doi: 10.1007/s10578-013-0378-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloum A, Scheeringa MS, Cohen JA, Amaya-Jackson L. Stepping together: Parent-child workbook for children (ages 3 to 7) after trauma, Version 1.2. 2009 Unpublished book. asalloum@usf.edu. [Google Scholar]
- Salloum A, Scheeringa MS, Cohen JA, Storch EA. Development of stepped care trauma focused cognitive-behavioral therapy for young children. Cognitive and Behavioral Practice. 2013;21:97–108. doi: 10.1016/j.cbpra.2013.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloum A, Scheeringa MS, Cohen JA, Storch EA. Responder status criterion for stepped care trauma-focused cognitive behavioral therapy for young children. Child and Youth Care Forum. 2015;44(1):59–78. doi: 10.1007/s10566-014-9270-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- Scheeringa MS, Haslett N. The reliability and criterion validity of the Diagnostic Infant and Preschool Assessment: a new diagnostic instrument for young children. Child Psychiatry and Human Development. 2010;41(3):299–312. doi: 10.1007/s10578-009-0169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Weems CF, Cohen JA, Amaya-Jackson L, Guthrie D. Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three-through six year-old children: A randomized clinical trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2011;52(8):853–860. doi: 10.1111/j.1469-7610.2010.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(5):561–570. doi: 10.1097/01.CHI.0000046822.95464.14. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW. Predictive validity in a prospective follow-up of PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(9):899–906. doi: 10.1097/01.chi.0000169013.81536.71. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, Amaya-Jackson L. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Thurston IB, Phares V. Mental health service utilization among African American and Caucasian mothers and fathers. Journal of Consulting and Clinical Psychology. 2008;76(6):1058–1067. doi: 10.1037/a0014007. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor. Highlights of women's earnings in 2010 (Vol Report #1031) Washington, DC: 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Stepped Care Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) Model
Table S1 Difference Test and Non-inferiority Test Results for Primary and Secondary Outcomes