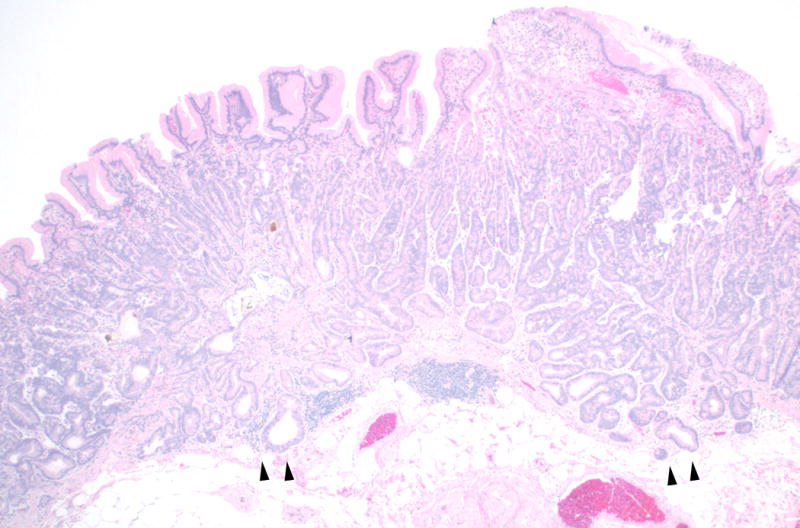
A previously healthy sixty-six year old Caucasian man was referred for an outpatient upper endoscopy and colonoscopy for mild iron deficiency anemia. He had episodic heartburn for which he occasionally took calcium carbonate. He denied any weight loss. His family history was positive for colon cancer in his mother at age 74. He had a twenty pack year tobacco history but quit one year ago. His colonoscopy identified two small tubular adenomas. On upper endoscopy, his esophagus and duodenum appeared normal. On retroflexion in the stomach, there was an irregular 7mm erythematous polypoid lesion in the fundus (Figure 1). Image enhanced endoscopy with narrow band imaging identified increased vascularity and a gyrus-like mucosal pit pattern (Figure 2). Band EMR was performed after initial biopsy revealed dysplasia and the polypoid lesion was removed en bloc. Histologic examination (hematoxylin and eosin stain, Figure 3) revealed well-differentiated gastric adenocarcinoma with chief cell differentiation arising from oxyntic mucosa and invading into the superficial submucosa (arrows). Mucosal and deep resection margins were clear of carcinoma and there was no lymphovascular or perineural invasion. The patient did well post procedure and will undergo a repeat upper endoscopy within six months.
Figure 1.

Figure 2.
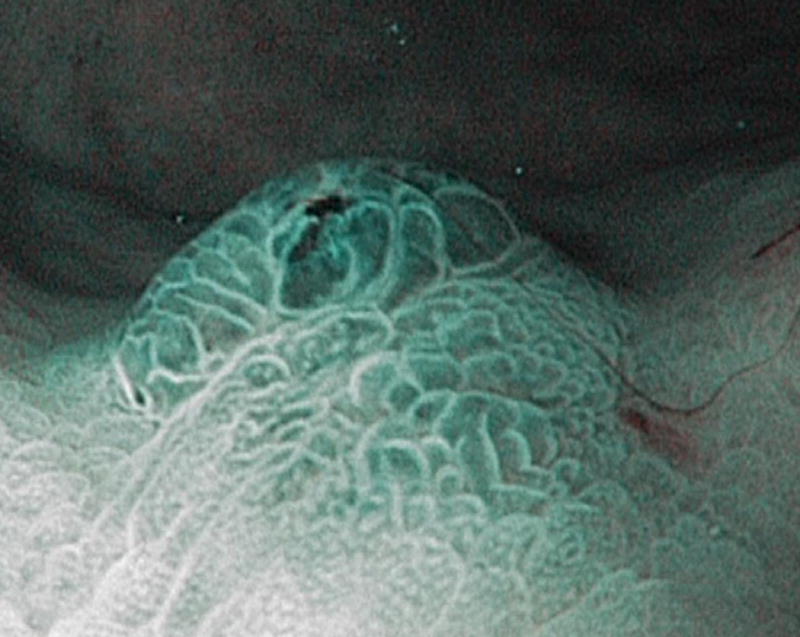
Figure 3.
While gastric adenocarcinoma is not an uncommon cancer worldwide, gastric adenocarcinoma with chief cell differentiation is a recently described rare epithelial neoplasm of the stomach with unique clinicopathologic characteristics. Unlike conventional types of gastric adenocarcinoma, which typically present with advanced, including metastatic, disease, gastric adenocarcinoma with chief cell differentiation may be a locally curable entity. The initial description in the literature was a case series of twelve Japanese patients.1 More recently, a second case series identified ten additional patients, two of whom were Caucasian.2 Like our patient, all reported patients to date had a solitary polyp, and in the majority, the polyp was located in the gastric fundus. Invasion limited to the submucosa was seen in the initial case series in the majority of patients, but was not identified in the second series, although in that study, specimens examined were superficial biopsy samples only and the submucosa was not evaluated. In both studies, none of the patients developed tumor recurrence or metastasis, leading authors to question if the term oxyntic gland polyp is more appropriate for this lesion, rather than gastric adenocarcinoma with chief cell differentiation. Regardless of the nomenclature, our case highlights that this rare variant of gastric adenocarcinoma may occur in non-Asian patients and emphasizes the utility of narrow band imaging and the importance of endoscopic mucosal resection, given the possibility of submucosal invasion and the ability to achieve curative resection of this rare and unique type of gastric neoplasm.
Footnotes
Author Contributions:
Neil D. Parikh was directly involved in patient care, literature review, drafting of manuscript and editing of manuscript. Joanna Gibson was involved in analysis, description and production of the gross and histopathologic images as well as editing of manuscript. Harry Aslanian was directly involved in patient care and critical revision of the manuscript for intellectual content.
Conflict of Interest:
Neil D. Parikh and Joanna Gibson have no conflicts of interest to report. Harry Aslanian has no specific conflicts of interest related to this submission but does serve as a consultant for both Boston Scientific and Olympus with regards to Endoscopic Ultrasound.
References
- 1.Ueyama H, Yao T, Nakashima Y, et al. Gastric adenocarcinoma of fundic gland type (chief cell predominant type): proposal for a new entity of gastric adenocarcinoma. The American journal of surgical pathology. 2010;34(5):609–19. doi: 10.1097/PAS.0b013e3181d94d53. [DOI] [PubMed] [Google Scholar]
- 2.Singhi AD, Lazenby AJ, Montgomery EA. Gastric adenocarcinoma with chief cell differentiation: a proposal for reclassification as oxyntic gland polyp/adenoma. The American journal of surgical pathology. 2012;36(7):1030–5. doi: 10.1097/PAS.0b013e31825033e7. [DOI] [PubMed] [Google Scholar]


