Abstract
The most important target of minimally invasive surgery is to obtain the best therapeutic effect with the least iatrogenic injury. In this background, a pivotal role in contemporary neurosurgery is played by the supraorbital key-hole approach proposed by Perneczky for anterior cranial base surgery. In this article, it is presented as a possible valid alternative to the traditional craniotomies in anterior cranial fossa meningiomas removal. From January 2008 to January 2012 at our department 56 patients underwent anterior cranial base meningiomas removal. Thirty-three patients were submitted to traditional approaches while 23 to supraorbital key-hole technique. A clinical and neuroradiological pre- and postoperative evaluation were performed, with attention to eventual complications, length of surgical procedure, and hospitalization. Compared to traditional approaches the supraorbital key-hole approach was associated neither to a greater range of postoperative complications nor to a longer surgical procedure and hospitalization while permitting the same lesion control. With this technique, minimization of brain exposition and manipulation with reduction of unwanted iatrogenic injuries, neurovascular structures preservation, and a better aesthetic result are possible. The supraorbital key-hole approach according to Perneckzy could represent a valid alternative to traditional approaches in anterior cranial base meningiomas surgery.
Keywords: anterior cranial base, meningioma, minimally invasive surgery, supraorbital key-hole approach
Introduction
“The same therapeutic effect with less iatrogenic injury.” This is the motto of clinical practice nowadays and one of the incentives for future scientific progress. One of the medical fields where this concept appears stronger is neurosurgery. Regarding brain tumor removal, for example, in the past wider craniotomies were necessary than the actual ones. This difference was caused by the availability of coarse surgical instruments, inadequate lighting of the surgical field, and inaccurate neuroradiological tools for precise characterization of the neoplasms. All these elements increased iatrogenic injuries related to brain retraction and manipulation.1–4) In this framework, the improvement of anatomical knowledge, surgical instrumentation (i.e., microinstruments, piezosurgery, and advanced endoscope with three-dimensional vision) and radiological techniques [tractography and functional magnetic resonance imaging (MRI)] granted the introduction and subsequent progressive evolution of microsurgical techniques and minimally invasive surgery.5–7) This allows surgeons to address the lesion with more specific and tailored minimally invasive approaches with potential less brain traumatization. The concept must be stressed: Minimally invasive surgery is not just a minimal skin incision. The minimally invasive attitude is a philosophy that begins from the first patient evaluation, through the maniacal respect of all tissues up to the precise layer by layer reconstruction aiming at selecting the less invasive approach tailored for that specific patient. Minimally invasive attitude must not be confused with minimalism: the effect on the neoplastic lesion has to be always maximally extensive otherwise it is better to select a traditional approach. In the minimally invasive neurosurgery, a pivotal role was played by the supraorbital key-hole approach proposed by Perneckzy at first for treatment of some intracranial aneurysms and then for anterior cranial base tumor removal as well.8) In this article, we report our experience with this surgical technique used in anterior cranial base meningiomas surgery, with the aim to propose this approach as a valid less invasive alternative to the conventional approaches.
Materials and Methods
From January 2008 to January 2012, 56 patients were admitted for the surgical removal of anterior cranial base meningiomas at our institution. In 33 patients, a traditional craniotomy tailored to the lesion was performed while in the other 23 patients a minimally invasive supraorbital approach according to Perneczky technique was done. We obtained written informed consent from subjects of this study (including the persons mentioned in Figs. 1 and 5).
Fig. 1.
Eyebrow skin incision in supraorbital key-hole approach.
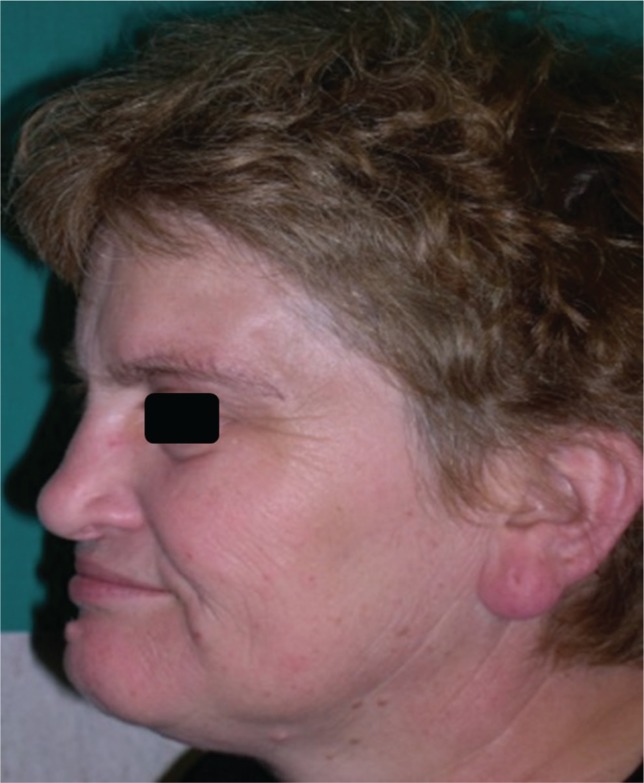
Fig. 5.
Postoperative evidence of pleasant aesthetic result granted by supraorbital key-hole approach.
In the first group, there were 23 females and 10 males with a mean age of 62.5 years while in the second one there were 14 females and 9 males with a mean age of 64.5 years.
Clinical onset was predominantly characterized by headache, seizures, visual loss, and personality changes. Before the surgical procedure, all patients were submitted to an MRI with angiogram phase integration. In some patients an integration with functional MRI, tractography, and computed tomography (CT) scan and\or angio CT were also done. Neuroimaging studies were performed with attention not only to dimension and specific localization of the meningioma but also to the angioarchitecture of the tumor, the entity of perilesional edema, and mass effect, its relationship with, and eventual compression of neurovascular structures. The locations and dimensions of the anterior cranial base tumors operated in both groups are indicated in Tables 1 and 2.
Table 1.
Location of meningiomas in patients submitted to supraorbital key-hole or traditional approaches
| Meningioma location | Traditional approach | Key-hole approach |
|---|---|---|
| Fronto-basal region | 16 | 6 |
| Olfactory groove | 6 | 5 |
| Medial third of little sphenoid wing | 5 | 2 |
| Tuberculum sellae | 2 | 4 |
| Ethmoidal planum | 1 | 3 |
| Anterior clinoid process | 3 | 2 |
| Fronto-orbital | 0 | 1 |
| Total | 33 | 23 |
Table 2.
Diameter of meningiomas treated by supraorbital key-hole or traditional approaches
| Tumor dimension | Traditional approach | Key-hole approach |
|---|---|---|
| < 1 cm | 1 | 0 |
| 1.5 cm | 0 | 1 |
| 2–2.5 cm | 6 | 6 |
| 3–3.5 cm | 6 | 5 |
| 4–4.5 cm | 7 | 5 |
| 5–5.5 cm | 6 | 3 |
| 6–6.5 cm | 5 | 2 |
| 7–7.5 cm | 1 | 1 |
| < 8 cm | 1 | 0 |
| Total | 33 | 23 |
Concerning the surgical procedure, a correct placement of the patient is important. In a supine position and after the head fixation with the Mayfield headholder, the head was rotated to the opposite side of the planned craniotomy with a degree depending on the size and location of the lesions. In fact, the access to the suprasellar region require 30 degrees of head rotation while in case of anterior cranial fossa tumors, like for example olfactory groove ones, require 45–60 degrees. To facilitate venous drainage, the head has to be elevated to about 15 degrees and to allow a spontaneous retraction of the frontal lobe neck of the patient it has to be retroflected to about 20 degrees.8)
The skin incision may follow the orbital rim, going from the supraorbital incisura along the eyebrow with respect to some important neurovascular structures like the superficial temporal artery, the supraorbital nerve, and the frontal branches of the facial nerve (Fig. 1).
To obtain excellent exposure of frontal and temporal muscles, the skin flap has to be dissected upward and gently retracted with stitches to avoid postoperative chewing problems or periorbital hematoma.8)
A high-speed drill could be used to perform single burr hole, located preferably posterior to the temporal line, and to complete the craniotomy. The size of minicraniotomy was around 2.5 cm (Fig. 2). In most recent cases, we further minimized the bone damage by using the ultrasonic scalpel (piezosurgery) without burr hole. A wide frontal sinus could be a relative contraindication of this approach, and in case of frontal sinus violation it could be exenterated by stripping and cauterizing the mucosa and covering it with a periosteal flap.9) It is important to perform a correct placement and direction of the burr hole and craniotomy to avoid orbit penetration.8) After supraorbital craniotomy, the tumor was removed piecemeal by the assistance of both microscope and endoscope.
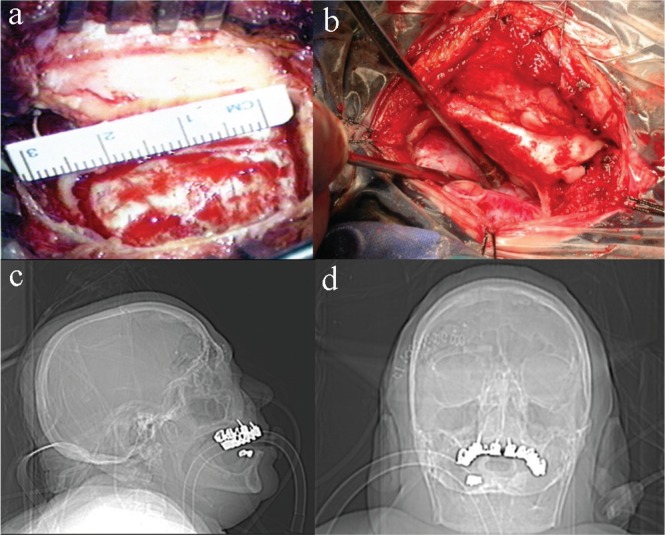
Fig. 2.
a, b: Intraoperative images and c, d: scout computed tomography scan showing the dimensions of the craniotomy performed through the supraorbital key-hole approach.
The extension of meningioma removal was intraoperatively determined by the operator and by a CT scan few days after the surgical procedure and by MRI 3 years, 6 years and every year after the operation (Figs. 3, 4). The follow-up period was from a minimum of 6 months to a maximum of 4 years.
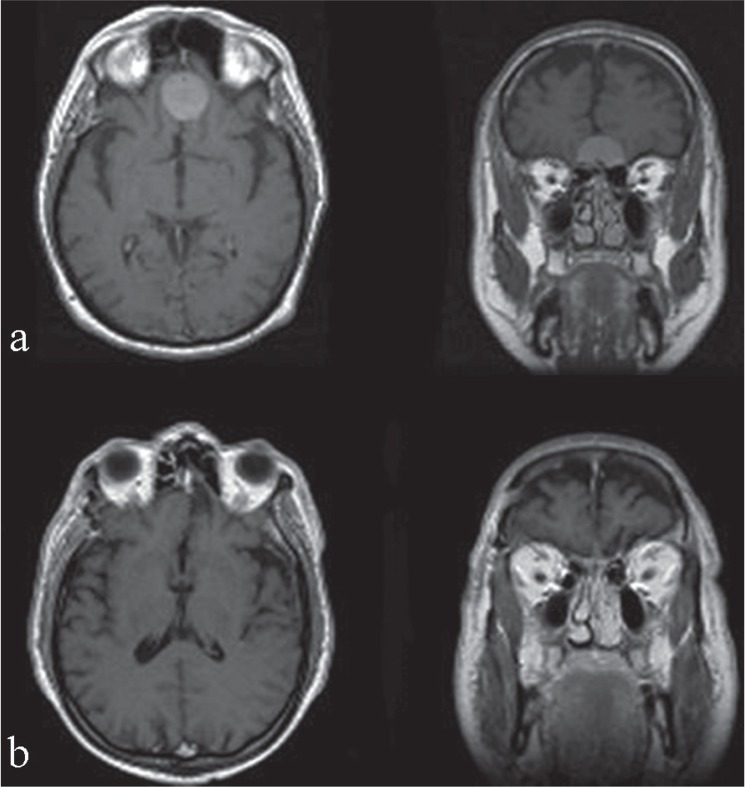
Fig. 3.
Illustrative case 2. A 62-year-old man with an olfactory groove meningioma (a) surgically treated by supraorbital key-hole approach (b).
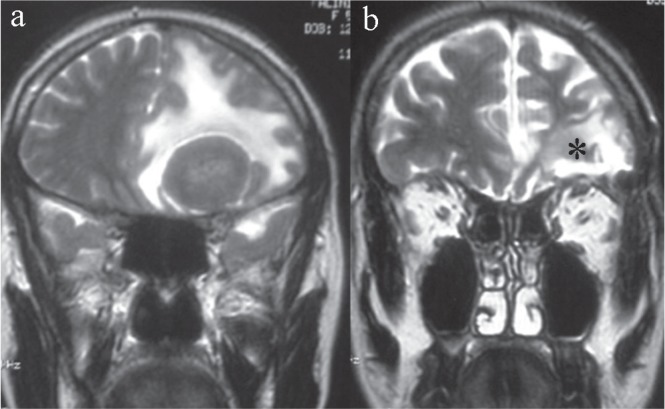
Fig. 4.
Illustrative case 1. A 71-year-old man with a left tuberculum sellae meningioma (a) who underwent a supraorbital craniotomy to completely remove the lesion (b). The asterisk shows the small surgical corridor that did not worsen the edema of the already suffering brain parenchyma.
Results
In our 4-year experience, 33 patients were submitted to anterior cranial base meningiomas removal through traditional craniotomies while 23 patients were operated on through a supraorbital key-hole approach according to Perneczky minimally invasive technique.
Total tumor resection, with resection of the basal dura and drilling of the hyperostotic bone, was reached in 27 out of 33 patients in the first group while it was 19 out of 23 for the second group.
Postoperatively, in patients submitted to traditional craniotomies, we experienced four complications (12.5%) represented by three cases of cerebrospinal fluid (CSF) leakage, solved after positioning of an external lumbar drainage, and one case of contralateral hemiparesis caused by an ischemic insult.
After a supraorbital key-hole approach, we had three postoperative problems (8%) represented by one case of CSF leakage (solved in the same way written before) and one case of visual deterioration.
Comparing these two groups, the rate of complications with the dimensions of tumors, divided in small (< 2.5 cm), intermediate (2.5–4.5 cm) and large (> 4.5 cm), we observed how in both groups all the complications happened after the removal of a small or an intermediate meningioma. We did not observe any complications after the resection of larger tumors.
Considering the duration of the surgical procedure in the key-hole group it had a mean duration of 5.8 hours while in the traditional craniotomies group we experienced a mean value of 5.03 hours.
Another important parameter that we observed is the hospitalization length with a mean hospitalization of 7 days in patients submitted to traditional approach without postoperative complications and 22 days in patients who experienced CSF leakage or other problems.
In patients submitted to a supraorbital key-hole approach we observed a mean hospitalization of 23 days in case of postoperative complications and 5 days in case of regular hospitalization.
Cosmetic outcome was slightly better in the supraorbital key-hole group compared to the traditional craniotomy group. In fact, among 23 patients who underwent supraorbital key-hole craniotomy, only 1 patient (4.34%) experienced aesthetic problems. This patient, treated at the beginning of our experience with the supraorbital key-hole approach, presented with a small depression behind the temporal line, where burr hole trephination was performed. This complication has been overcome in subsequent operations through the use of piezosurgery. Piezosurgery allowed a regular and thin bone cutting facilitating the bone flap healing and preventing indentation of the overlying skin with subsequent good aesthetic results as well as increased comfort for the patient. In the other patients, we never observed loss of eyebrows, and the surgical scar was hidden by the eyebrows always with an acceptable aesthetic result. A limited skin incision within the eyebrow, avoiding the use of cautery, minimal temporalis muscle dissection, and closure with the orbicularis oculi muscle and pericranium layers have contributed to the success of the eyebrow incision. In traditional craniotomy group, there were three cases of cosmetic deformities (9.09%) due to a complete lesion of the frontotemporal branch of the facial nerve in one case and an atrophy of the temporal muscle in the other two cases.
Discussion
Nowadays, one of the most emphasized concepts in neurosurgery is represented by the necessity to obtain the best therapeutic effect with the least iatrogenic and aesthetical injury.
In the past, in fact, resection especially of large or deep-seated lesions was possible only by large craniotomies with an inherent elevated risk of neurovascular injuries. This is because these approaches entailed per se extensive soft tissue and neurovascular retraction, causing an increasing surgical morbidity connected not to the lesions but to the surgical approach itself.2,4)
The evolution for the actualization of the supraorbital key-hole minimally invasive approach according to Perneckzy has been a long journey. From the first description of a subfrontal approach by Francesco Durante in 1884 to the introduction of the pterional one proposed by Yasargil, a lot of advancements in the surgical technique were observed.10,11) The first description of a supraorbital subfrontal approach was proposed by Krause during the first years of 1900, followed few years later by Tandler and Ranzi.12,13) In the same period, to reduce the damage caused by frontal lobe retraction, McArthur and Frazier proposed modifications as the removal of the supraorbital arch.14,15) Some of the most important surgeons of that period like Cushing, Heuer, and Dandy reported their large series of patients submitted to a subfrontal approach for anterior cranial base lesions, indicating how the unnecessary exposition of excessive brain surface could allow subsequent injuries eventually leading to epilepsy.10,16–18) Unfortunately, during the first years of past century, large craniotomies were necessary considering the difficulty in the deep surgical field illumination and the absence of microsurgical instrumentation. Only after the progressive development of neuroradiological techniques and the introduction of specific instruments, smaller but tailored approaches appeared possible. After the introduction of the operating microscope for example the subfrontal approach previously proposed by Dandy was modified by Yasargil in 1975, by reducing the craniotomy size to two-third.19) With the advent of endoscope, the refinement of microinstruments and the advent of piezosurgery, in these last two decades, the supraorbital exposure was further improved and its indications expanded. Different types of supraorbital subfrontal approaches are indicated by different names but they appear quite similar. In this background, a pivotal role was played above all by Perneczky, and also by van Lindert and Czirjak et al.20–31)
All these approaches were proposed with the aim to, by performing smaller craniotomies, reduce brain exposure and spatulation. Indeed, one of the most important problems is represented by the excessive brain retraction that could lead to brain injuries causing permanent neurological deficits. Like Perneckzy said “the best retraction is no retraction,”8) surgical approach should be selected on the basis of the capacity to reach the lesion through a natural direct way (i.e., cisternal space or through the nose) along the greatest diameter of the lesion.
The volume of the lesion per se is not an absolute issue being possible to work in depth and remove large tumors through keyhole-like craniotomies. Nevertheless, in the supraorbital key-hole craniotomy the extension of the exposure is anatomically restricted laterally by the temporal branch of the facial nerve and superiorly limited by skin retraction. For these reasons, the visual axis runs almost parallel to the inserted micro-instruments and the surgeon is compelled to operate mostly in a horizontal plane than in a vertical one. Then, in case of meningiomas with development prevailing in the vertical plane and significant lateral extension, we preferred traditional craniotomy in order to maintain a good balance between exposure of the surgical field and ability of dissection and manipulation of the anatomical structures.
The supraorbital approach is not suitable for all lesions, and indications must be individualized. In case of significant calcification or lateral extension of the tumor behind the anterior circulation vessels and optic nerve, complete encasement of carotid artery, invasion of the ethmoid sinuses, severe bifrontal edema, and suspected subclinoidal or optic canal implant of the lesion, we preferred conventional approaches.
Probably, the biggest limitation was the problem of lighting with the operating microscope down such a narrow corridor. Endoscopy assistance has dramatically improved visualization of this region through this approach and allows for safer dissection with better visualization than that achievable by the microscope alone. Some concern still exist with some instruments not fully designed for key-hole surgery, but this is only time consuming, not influencing the suitability and safety of the instruments during surgery.
From an aesthetic point of view, this approach is really minimally invasive, granting minimal patient discomfort and optimal aesthetic result (Fig. 5).
The supraorbital key-hole minimally invasive approach through an eyebrow skin incision represents a valid alternative to the traditional craniotomies in anterior cranial fossa meningioma surgery.
This minimally invasive procedure provides the same exposition and chances of tumor control, as wider craniotomies, without increasing the complication rate, hospital stay, and patient discomfort.
Indeed, through this limited craniotomy wide brain areas and even deep-seated lesions can be approached, giving minimal iatrogenic trauma and pleasant aesthetic result.
References
- 1). Al-Mefty O: Supraorbital-pterional approach to skull base lesions. Neurosurgery 21: 474– 477, 1987. [DOI] [PubMed] [Google Scholar]
- 2). Fujitsu K, Kuwabara T: Zygomatic approach for lesions in the interpeduncular cistern. J Neurosurg 62: 340– 343, 1985. [DOI] [PubMed] [Google Scholar]
- 3). Maroon JC, Kennerdell JS: Surgical approaches to the orbit. Indications and techniques. J Neurosurg 60: 1226– 1235, 1984. [DOI] [PubMed] [Google Scholar]
- 4). Zabramski JM, Kiriş T, Sankhla SK, Cabiol J, Spetzler RF: Orbitozygomatic craniotomy. Technical note. J Neurosurg 89: 336– 341, 1998. [DOI] [PubMed] [Google Scholar]
- 5). Cohen AR, Perneczky A, Rodziewicz GS, Gingold SI: Endoscope-assisted craniotomy: approach to the rostral brain stem. Neurosurgery 36: 1128– 1129; discussion 1129–1130, 1995. [DOI] [PubMed] [Google Scholar]
- 6). Jho HD: Orbital roof craniotomy via an eyebrow incision: a simplified anterior skull base approach. Minim Invasive Neurosurg 40: 91– 97, 1997. [DOI] [PubMed] [Google Scholar]
- 7). Paladino J, Pirker N, Stimac D, Stern-Padovan R: Eyebrow keyhole approach in vascular neurosurgery. Minim Invasive Neurosurg 41: 200– 203, 1998. [DOI] [PubMed] [Google Scholar]
- 8). Reisch R, Perneczky A: Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery 57 (4 Suppl): 242– 255; discussion 242–255, 2005. [DOI] [PubMed] [Google Scholar]
- 9). Park HS, Park SK, Han YM: Microsurgical experience with supraorbital keyhole operations on anterior circulation aneurysms. J Korean Neurosurg Soc 46: 103– 108, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Thorwald J: Im zerbrechlichen Haus der Seele. Munich, Droemer-Knaur-Verlag, 1986. [Google Scholar]
- 11). Yaşargil MG, Reichman MV, Kubik S: Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg 67: 463– 466, 1987. [DOI] [PubMed] [Google Scholar]
- 12). Krause F. Chirurgie des Gehirns und Rückenmarks nach eigenen Erfahrungen. Berlin, Urban & Schwarzenberg, 1908. [Google Scholar]
- 13). Tandler J, Ranzi E: Surgical Anatomy and Operation Technology of the Central Nervous System (in German). Berlin, Springer, 1920. [Google Scholar]
- 14). McArthur LL: An aseptic surgical access to the pituitary body and its neighbourhood. JAMA LVIII: 2009– 2011, 1912. [Google Scholar]
- 15). Frazier CH: An approach to the hyphophysis through the anterior cranial fossa. Ann Surg 1: 145– 150, 1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Cushing H, Eisenhardt L: Meningiomas: Their Classification, Regional Behaviour, Life History, and Surgical End Results. Illinois, Charles C Thomas, 1938. [Google Scholar]
- 17). Heuer GJ: Surgical experience with an intracranial approach to chiasmal lesions. Arch Surg 1: 368– 381, 1920. [Google Scholar]
- 18). Kurze T: Microtechniques in neurological surgery. Clin Neurosurg 11: 128– 137, 1964. [DOI] [PubMed] [Google Scholar]
- 19). Yasargil MG, Fox JL, Ray MW: The operative approach to aneurysm of the anterior communicating artery, in Krayenbühl H. (ed): Advances and Technical Standards in Neurosurgery, Vol II. New York, Springer Verlag, 1975, pp 115– 128 [Google Scholar]
- 20). Czirják S, Nyáry I, Futó J, Szeifert GT: Bilateral supraorbital keyhole approach for multiple aneurysms via superciliary skin incisions. Surg Neurol 57: 314– 323; discussion 323–324, 2002. [DOI] [PubMed] [Google Scholar]
- 21). Czirják S, Szeifert GT: Surgical experience with frontolateral keyhole craniotomy through a superciliary skin incision. Neurosurgery 48: 145– 149; discussion 149–150, 2001. [PubMed] [Google Scholar]
- 22). Fries G, Perneczky A: Endoscope-assisted brain surgery: part 2—analysis of 380 procedures. Neurosurgery 42: 226– 231; discussion 231–232, 1998. [DOI] [PubMed] [Google Scholar]
- 23). Menovsky T, Grotenhuis JA, de Vries J, Bartels RH: Endoscope-assisted supraorbital craniotomy for lesions of the interpeduncular fossa. Neurosurgery 44: 106– 110; discussion 110–112, 1999. [DOI] [PubMed] [Google Scholar]
- 24). Perneczky A: Planning strategies for the suprasellar region: philosophy of approaches. Neurosurgeons 11: 343– 348, 1992. [Google Scholar]
- 25). Perneczky A, Fries G: Use of a new aneurysm clip with an inverted-spring mechanism to facilitate visual control during clip application. Technical note. J Neurosurg 82: 898– 899, 1995. [DOI] [PubMed] [Google Scholar]
- 26). Pernecczky A, Müller-Forell W, van Lindert E, Fries G: Keyhole Concept in Neurosurgery. Stuttgart, Thieme Medical Publishers, 1999. [Google Scholar]
- 27). Iacoangeli M, Neri P, Balercia P, Lupi E, Di Rienzo A, Nocchi N, Alvaro L, Scerrati M: Piezosurgery for osteotomies in orbital surgery: Our experience and review of the literature. Int J Surg Case Rep 4: 188– 191, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28). Roselli R, Iacoangeli M, Pompucci A, Trignani R, Restuccia D, Di Lazzaro V, Scerrati M: Anterior cervical epidural abscess treated by endoscopy-assisted minimally invasive microsurgery via posterior approach. Minim Invasive Neurosurg 41: 161– 165, 1998. [DOI] [PubMed] [Google Scholar]
- 29). Iacoangeli M, Di Rienzo A, Nocchi N, Balercia P, Lupi E, Regnicolo L, Di Somma LG, Alvaro L, Scerrati M: Piezosurgery as a further technical adjunct in minimally invasive supraorbital keyhole approach and lateral orbitotomy. J Neurol Surg A Cent Eur Neurosurg 76: 112– 118, 2015. [DOI] [PubMed] [Google Scholar]
- 30). Iacoangeli M, Di Rienzo A, Alvaro L, Scerrati M: Fully endoscopic endonasal anterior C1 arch reconstruction as a function preserving surgical option for unstable atlas fractures. Acta Neurochir (Wien) 154: 1825– 1826, 2012. [DOI] [PubMed] [Google Scholar]
- 31). Iacoangeli M, Di Rienzo A, di Somma LG, Moriconi E, Alvaro L, Re M, Salvinelli F, Carassiti M, Scerrati M: Improving the endoscopic endonasal transclival approach: the importance of a precise layer by layer reconstruction. Br J Neurosurg 28: 241– 246, 2014. [DOI] [PubMed] [Google Scholar]