Abstract
Objective. To evaluate how municipality-based post-discharge follow-up visits including a general practitioner and municipal nurse affect early readmission among high-risk older people discharged from a hospital department of internal medicine. Design and setting. Centrally randomized single-centre pragmatic controlled trial comparing intervention and usual care with investigator-blinded outcome assessment. Intervention. The intervention was home visits with a general practitioner and municipal nurse within seven days of discharge focusing on medication, rehabilitation plan, functional level, and need for further health care initiatives. The visit was concluded by planning one or two further visits. Controls received standard health care services. Patients. People aged 65 + years discharged from Holbæk University Hospital, Denmark, in 2012 considered at high risk of readmission. Main outcome measures. The primary outcome was readmission within 30 days. Secondary outcomes at 30 and 180 days included readmission, primary health care, and municipal services. Outcomes were register-based and analysis used the intention-to-treat principle. Results. A total of 270 and 261 patients were randomized to intervention and control groups, respectively. The groups were similar in baseline characteristics. In all 149 planned discharge follow-up visits were carried out (55%). Within 30 days, 24% of the intervention group and 23% of the control group were readmitted (p = 0.93). No significant differences were found for any other secondary outcomes except that the intervention group received more municipal nursing services. Conclusion. This municipality-based follow-up intervention was only feasible in half the planned visits. The intervention as delivered had no effect on readmission or subsequent use of primary or secondary health care services.
Keywords: Community health nursing, Denmark, frail elderly, patient readmission, population register, primary health care, quality of health care, randomized controlled trial
Collaboration between hospital and primary care providers is imperative to ensure high-quality post-discharge care to the fragile elderly.
This randomized controlled trial compared municipality-based post-discharge follow-up visits with usual care among high-risk older people in a pragmatic study.
The intervention was only feasible in 55% of the planned visits and showed no effect on the primary outcome of readmission within 30 days or subsequent use of primary or secondary health care services.
Preventing early readmissions is important, and effective screening tools for appropriate targeted discharge follow-up need to be developed further.
Introduction
The need for complex interventions is expected to increase because of a growing older population, improving survival rate following acute health conditions, and improved treatment options leading to a growing population living with chronic disease [1,2]. Older people admitted to hospital often have complex treatment, rehabilitation, and nursing needs [3]. Poor care coordination at the time of hospital discharge can jeopardize patient safety and result in substandard health care [4,5], and patients and their caregivers are often ill prepared for the transition from hospital to home [6].
Collaboration between hospital and primary care providers is imperative to ensure high-quality post-discharge care, indicating a growing need for coordination between primary and secondary health care systems [7]. A high readmission rate is often seen as a proxy of lack of quality in the transition from the secondary to the primary sector. The hospital often loses contact with the patient at discharge, and the municipality is responsible for helping frail older people.
Several randomized intervention studies have investigated hospital discharge planning [8–14] or interventions by clinical pharmacists [15,16] on hospital readmission, primary care, prescription errors, and quality of life among older people and people with chronic diseases. Community-based disease-management programmes significantly reduced readmission among patients with heart failure, coronary heart disease, and asthma, while interventions among unselected older patients with chronic diseases did not affect hospital readmission [17,18]. Some studies suggest that systematic post-discharge support and effort may result in better coordination and coherence in treatment and may reduce unplanned readmission although the results are not consistent [7,19–22].
We performed a randomized controlled trial among a high-risk population of older people discharged from a hospital department of internal medicine to evaluate whether a systematic municipality-based post-discharge follow-up intervention including the primary general practitioner and municipal nurse in a real-world setting could reduce readmission and the use of primary and secondary health care.
Material and methods
Design
The study was a single-centre, 1:1 parallel-group individual patient randomized controlled trial stratified by gender and age (65–74 years and 75 + years) followed for 180 days. The trial was pragmatic and mirrored everyday clinical practice of the hospital personnel, general practitioners, or municipal nurses. The study was conducted and reported in accordance with the CONSORT guidelines [23].
Participants and recruitment
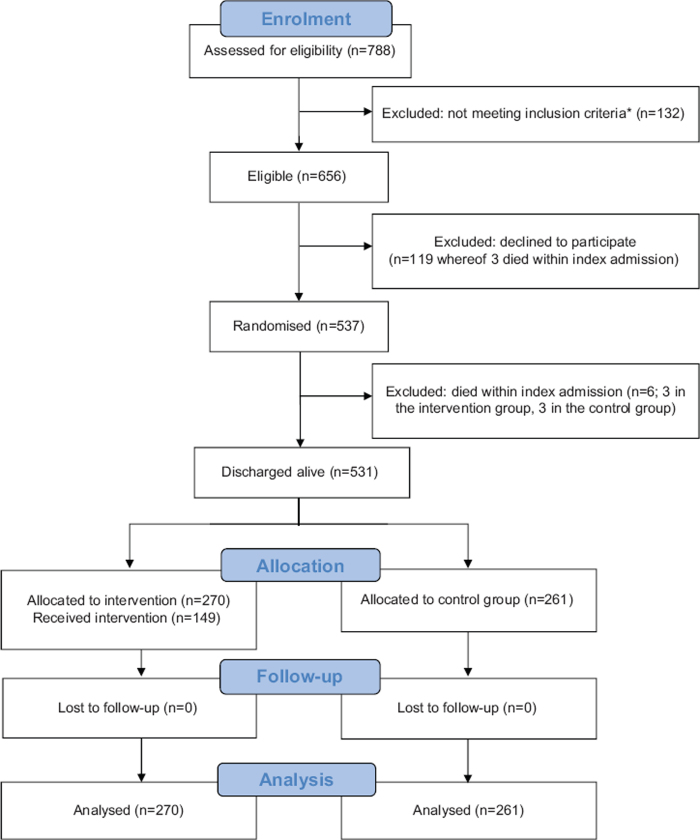
The study included patients aged 65 years or older discharged alive from the Department of Internal Medicine of Holbæk University Hospital, Denmark from 16 February 2012 to 14 September 2012 and living in one of the three surrounding municipalities, Holbæk, Odsherred, or Kalundborg, and who had dementia or two of the conditions presented in Figure 1. The screening was based on medical assessment by physicians at the hospital department.
Figure 1.
Flow diagram. Note: *Inclusion criteria were patients aged 65 years or older discharged alive from the Department of Internal Medicine of Holbæk University Hospital, Denmark and living in one of the three surrounding municipalities and who had dementia or two of the following conditions: two or more hospital admissions within the 12 months before the index admission, loss of physical functioning, treatment of two or more concurrent medical or surgical conditions, mental disorder, six or more prescription medications, symptoms of cognitive disturbance, substance abuse problem, disadvantaged social network, or need for increasing home care following the index admission.
When a patient was randomized to the intervention group, contact was made with the municipality of residence, and the patient's general practitioner who received a standard discharge letter including information on planned post-discharge follow-up intervention. The municipal nurse coordinated the visits with the general practitioner.
All patients received the standard health care services, and the patients in the intervention group received the additional interventional health care service. All patients provided informed consent.
Baseline and follow-up measures
Data on the length of index admission, gender, and age were registered at inclusion in the study [24].
Baseline information on marital status and citizenship on admission was obtained through the Civil Registration System [26]. The Charlson comorbidity score was calculated using information on primary and secondary diagnoses from all in- and outpatient contacts with Danish hospitals from 10 years before index admission and including the index admission [23]. Information on municipal services was obtained from municipal registration available on a monthly basis. We calculated the referred services (measured as minutes of referred care), divided into home care (practical help and personal care), nursing home (services at a care home) and nursing (services offered by a municipal nurse). This information was available only among trial participants and not for eligible non-participants.
Follow-up measures were in-hospital readmissions obtained from the Danish National Patient Register, which contains information on all contacts with Danish hospitals [24]. Information on contacts with the general practitioner and visits by the emergency service doctor were obtained from the Danish National Health Service Register [26]. Information on municipal services was obtained from the three surrounding municipalities. Information on mortality was obtained from the Civil Registration System [25]. No patients emigrated during follow-up.
The predefined primary outcome was unplanned readmission to any hospital in Denmark within 30 days after the discharge from the index admission.
The predefined secondary outcomes were readmission, number of readmissions, and length of stay both for all admissions combined, unplanned admissions, and admissions to departments of medicine. We performed all analysis within 30 and 180 days of follow-up after discharge.
Further, the mean number of consultations with general practitioners and visits by the emergency service doctor during follow-up were calculated. Finally, municipal services were calculated as the proportion of people who received the services and, among those who received the services, the mean number of monthly minutes of services the month after and one to six months after the index admission. As a descriptive measure, mortality was also evaluated as an outcome.
Randomization
The physicians at the Department of Internal Medicine screened the patients, nurses collected informed consent, and the patients were then randomized. The Data Management Department of the Central Denmark Region centrally administered a computer-generated randomization sequence by using Trial Partner. The medical secretary faxed the screening information to the municipal services independently of randomization group. For the intervention group, the municipality organized the intervention with the general practitioner.
The doctors screening for eligibility were blinded toward intervention groups. Further, the data analyst obtaining register-based outcome information was blinded towards the randomization groups in the analysis. No methods were changed after the trial began.
Interventions
High-risk people were referred to intervention through systematic electronic referral from the hospital to the municipality. The municipal services contacted the primary general practitioner and then the patient, to arrange the first home visit together with the municipal nurse within seven days of discharge in the patient's home. Only visits where both municipal nurse and general practitioner participated were included in the study. The visit was scheduled for one hour and focused on medication, rehabilitation plan and hospital appointments, functional level, and need for further health care initiatives. The visit concluded with assessment of the need for further visits (up to three visits) and division of responsibilities between the general practitioner and the municipal nurse. The second consultation was planned for the third week and the third consultation in the eighth week after discharge.
Patients in the control group were assigned to usual care including a discharge letter from the hospital to the general practitioner but not including coordinated home visits from the municipal nurse and the primary general practitioner. In Denmark's health care system, all residents can seek consultation with a general practitioner, and residents with physical disabilities can receive home care without any user charges. This means that participants from both groups could be in regular contact with a general practitioner and/or a municipal nurse during follow-up.
Statistical analysis
The baseline characteristics of participants versus eligible non-participants were compared.
We performed all analysis based on the intention-to-treat principle. For the primary outcome analysis, patients were followed for hospital admission 30 days following the discharge from the index admission. As secondary outcomes, we followed the cohort for unplanned admissions, admissions to departments of medicine, and number of consultations with general practitioners for both 30 and 180 days. We also analysed mortality as a descriptive measure and to evaluate the influence of competing risk. We tested all differences using the chi-square test. For the primary outcome, we also estimated the Kaplan–Meier survival plots and tested differences using the log-rank test. We also evaluated the mean number of admissions and length of stay and tested differences using the t-test.
We compared the proportion receiving municipal services using the chi-square test and, among those who received services, we compared the mean minutes of services using the t-test. We performed these calculations only for patients who were alive during the whole follow-up period.
The epidemiologist responsible for all statistical analysis (LCT) was blinded towards the intervention status. We performed post-hoc unblinded per-protocol analysis, with per protocol defined as visits by the general practitioner at least once during the intervention period and the follow-up started at the time of the first visit or on day 14 after discharge for the control group.
We used two-sided p-values, and ≤ 0.05 was defined as statistically significant. We used SAS, version 9.3.
Sample size
Using electronic data delivered from the Ministry of Health, the 30-day readmission rate for the hospital was estimated to be 13%. We calculated that a sample size of 240 in each group would have 90% power and a significance level of 5% to detect a clinically relevant reduction of 20% in the readmission rate in the intervention group versus the control group as found in a previous Danish randomized controlled trial on follow-up intervention [21].
Results
Of the 789 patients assessed for eligibility, 132 did not meet the inclusion criteria, 119 declined to participate (18%) and six died during index admission (see Figure 1). Study participants were similar to eligible non-participants in admissions at 30 days, but non-participants had higher mortality (10.3% compared with 4.1% among participants – not shown). Thus, 531 patients were randomized into intervention (n = 270) and control (n = 261). No patients were lost to follow-up.
The intervention and control groups were similar in baseline characteristics, although there were minor differences for marital status and for comorbidity (Table I).
Table I.
Baseline characteristics of the included patients.
| Baseline characteristics | Control (n = 261) | Intervention (n = 270) | Eligible non-participants (n = 117) |
|---|---|---|---|
| Median length of index admission (interquartile range) | 6 (3–12) | 5 (3–10) | 5 (3–11) |
| Female gender, n (%) | 124 (47.5) | 131 (48.5) | 66 (56.9) |
| Mean age, years (standard deviation) | 77.7 (7.2) | 77.8 (7.9) | 78.7 (8.6) |
| Age, n (%) | |||
| 65–69 years | 43 (16.5) | 50 (18.5) | 24 (20.7) |
| 70–77 years | 82 (31.4) | 77 (28.5) | 34 (29.3) |
| 78–84 years | 81 (31.0) | 85 (31.5) | 25 (21.6) |
| 85–89 years | 46 (17.6) | 35 (13.0) | 17 (14.7) |
| 90–97 years | 9 (3.5) | 23 (8.5) | 16 (13.8) |
| Marital status, n (%) | |||
| Married | 120 (46.0) | 109 (40.4) | 54 (46.6) |
| Divorced | 27 (10.3) | 42 (15.6) | 14 (12.1) |
| Unmarried | 11 (4.2) | 10 (3.7) | 7 (6.0) |
| Widowed | 103 (39.5) | 109 (40.4) | 41 (35.3) |
| Danish citizenship, n (%) | 260 (99.6) | 268 (99.3) | 115 (99.1) |
| Charlson comorbidity score, n (%) | |||
| 0 | 31 (11.9) | 28 (10.4) | 21 (18.1) |
| 1 | 58 (22.2) | 68 (25.2) | 30 (25.9) |
| 2 | 61 (23.4) | 60 (22.2) | 27 (23.2) |
| 3 | 34 (13.0) | 44 (16.3) | 9 (7.8) |
| 4–12 | 77 (29.5) | 70 (25.9) | 29 (25.0) |
The primary reasons for patients being selected for the trial were previous readmission, active medical or surgical treatment, or six or more prescription drugs; only 12% of the patients had dementia (Table II). For patients without dementia, 57% had two other reasons and 43% had three or more reasons (not shown).
Table II.
Reasons for selecting patients for the intervention and numbers and types of home visits and contacts during the intervention period (numbers [percentages] unless stated otherwise).
| Control | Intervention | |
|---|---|---|
| Reasons selected for intervention, n (%): | ||
| Dementia or suspected dementia | 30 (11.5) | 34 (12.6) |
| Admitted to hospital at least two times in the past 12 months | 143 (54.8) | 147 (54.4) |
| Large loss in ability to carry out the activities of daily living | 58 (22.2) | 56 (20.7) |
| Active medical or surgical treatment | 206 (78.9) | 211 (78.2) |
| Active psychiatric treatment | 11 (4.2) | 18 (6.7) |
| Six or more prescription drugs | 167 (64.0) | 161 (59.6) |
| Suspected cognitive disturbance or problems | 24 (9.2) | 21 (7.8) |
| Substance abuse that influences functional level | 1 (0.4) | 5 (1.9) |
| Disadvantaged social network | 5 (1.9) | 5 (1.9) |
| Increased municipal services | 15 (5.8) | 13 (4.8) |
| Number and types of home visits, n (%): | ||
| First home visit carried out | NA | 149 (55.2) |
| Second home visit carried out | NA | 49 (18.1) |
| Third home visit carried out | NA | 8 (3.0) |
| Activities at the first home visit, n (%):* | ||
| Follow-up on discharge summary | NA | 121 (81.2) |
| Drug evaluation | NA | 122 (81.9) |
| Change in drug use | NA | 57 (38.3) |
| Evaluate patient's resources and limitations | NA | 104 (69.8) |
| Number of contacts, including contacts outside the intervention, n (mean): | ||
| By telephone | 281 (1.08) | 383 (1.42) |
| Consultation | 189 (0.72) | 222 (0.82) |
| Consultation by nurse | 145 (0.56) | 176 (0.65) |
| Consultation in patient's own home | 50 (0.19) | 119 (0.44) |
Notes: NA = not available or not applicable. *Percentage with the activity among patients receiving the first visits (n = 149).
In the intervention group, 149 (55%) of the patients received the first home visit, 49 (18%) the second visit, and eight (3%) the third visit (see Table II). During the first visit follow-up on discharge summary and drug evaluation were carried through for the majority of visits and change in drug use was performed for 57 patients (38%) (see Table II).
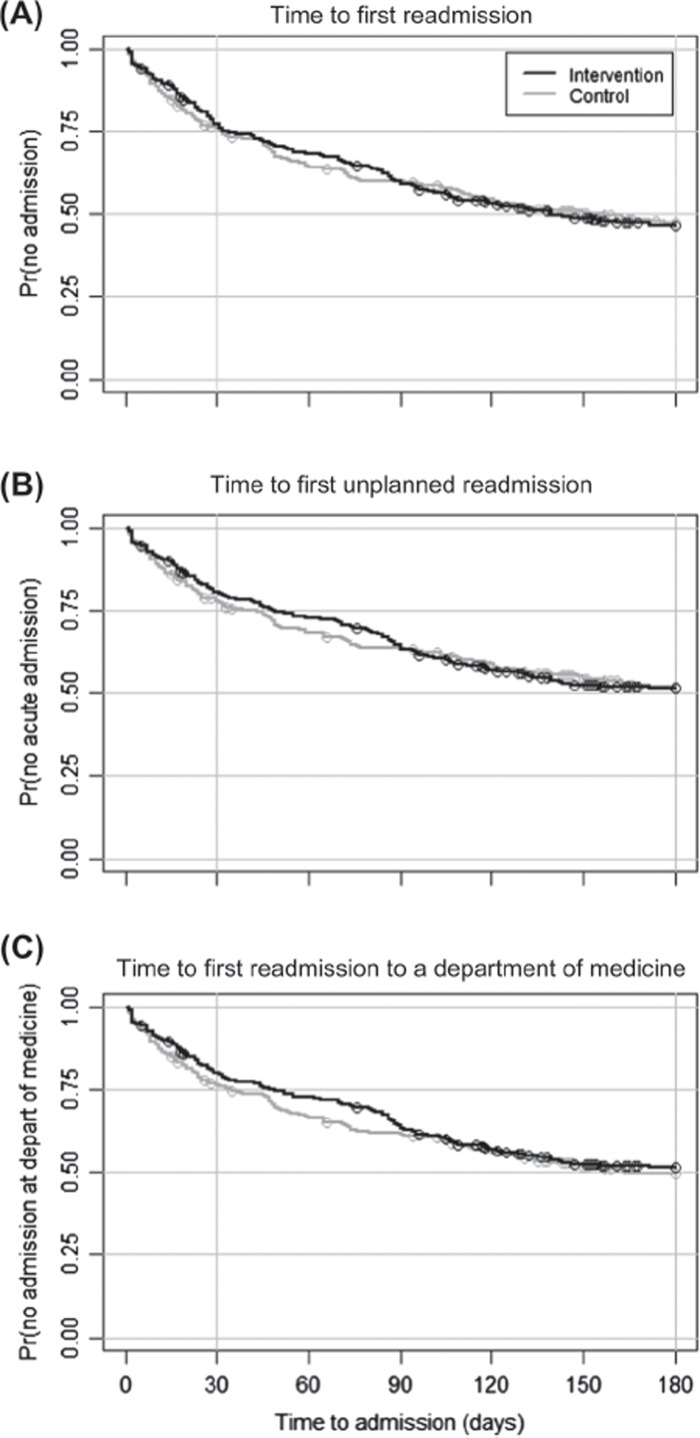
The intervention and control groups did not differ in the primary outcome, with 23% of control patients and 24% of intervention patients readmitted within 30 days of discharge (p = 0.93) (Table III). The number of admissions and length of stay were also similar. The survival curve for time until first readmission also showed no difference between the two groups during the first 30 days (Figure 2A) (log-rank test, p = 0.70).
Table III.
Admissions, contacts with general practitioner, and deaths at 30 and 180 days and referred municipal services (home care, nursing home, and nursing) 1–6 months after the index admission.
| 30 days | 180 days | |||||
|---|---|---|---|---|---|---|
| Control | Intervention | p* | Control | Intervention | p* | |
| Admission, n (%) | 61 (23.4) | 64 (23.7) | 0.93 | 134 (51.3) | 140 (51.9) | 0.91 |
| Number of admissions, n (mean) | 73 (0.3) | 84 (0.3) | 0.72 | 252 (1.0) | 288 (1.1) | 0.81 |
| Length of stay, n (mean) | 465 (1.8) | 355 (1.3) | 0.90 | 1638 (6.3) | 1846 (6.8) | 0.63 |
| Unplanned admission, n (%) | 56 (21.5) | 56 (20.7) | 0.84 | 122 (46.7) | 127 (47.0) | 0.95 |
| Number of unplanned admissions, n (mean) | 67 (0.3) | 67 (0.3) | 0.97 | 220 (0.8) | 241 (0.9) | 0.89 |
| Length of stay, n (mean) | 454 (1.7) | 310 (1.1) | 0.79 | 1536 (5.9) | 1697 (6.3) | 0.75 |
| Admission to departments of internal medicine, n (%) | 60 (23.0) | 57 (21.1) | 0.60 | 128 (49.0) | 127 (47.0) | 0.64 |
| Number of admissions to departments of internal medicine, n (mean) | 70 (0.3) | 76 (0.3) | 0.85 | 226 (0.9) | 244 (0.9) | 0.86 |
| Length of stay at departments of internal medicine, n (mean) | 464 (1.8) | 316 (1.2) | 0.48 | 1586 (6.1) | 1659 (6.1) | 0.96 |
| Number of general practitioner consultations (n, mean)† | 516 (2.0) | 588 (2.2) | 0.04 | 2405 (9.2) | 2654 (9.8) | 0.18 |
| Number of visits by emergency service doctor (n, mean) | 64 (0.2) | 72 (0.3) | 0.51 | 185 (0.7) | 259 (1.0) | 0.19 |
| Death, n (%) | 9 (3.5) | 13 (4.8) | 0.45 | 39 (14.9) | 35 (13.0) | 0.58 |
| Patients receiving services, n (%) | Mean minutes per month among patients receiving services | |||||
|---|---|---|---|---|---|---|
| The month after discharge: | ||||||
| Home care | 114 (46) | 131 (52) | 0.24 | 1291 | 970 | 0.14 |
| Nursing home | 18 (7) | 21 (8) | 0.69 | 1875 | 1527 | 0.63 |
| Nursing | 85 (35) | 154 (61) | < 0.001 | 367 | 229 | 0.03 |
| 1–6 months after discharge: | ||||||
| Home care | 103 (47) | 130 (56) | 0.04 | 7082 | 5001 | 0.10 |
| Nursing home | 20 (9) | 23 (10) | 0.75 | 9953 | 8732 | 0.73 |
| Nursing | 85 (38) | 149 (64) | < 0.001 | 1811 | 1107 | 0.04 |
Notes: *Chi-square test for difference in proportions between the intervention and control groups and t-test for mean differences between the intervention and control groups. †The number of consultations as part of the intervention is not included in this row.
Figure 2.
Time to (A) first readmission, (B) first unplanned readmission, and (C) first readmission to a department of medicine.
The intervention and control groups did not differ in admissions after 180 days, unplanned admissions at 30 and 180 days, and admissions to departments of medicine at 30 and 180 days (see Table III). Figures 2B and 2C indicated a trend toward more rapid unplanned admissions and admissions to departments of medicine in the control group compared with the intervention group in the first 90 days, although these differences were not statistically significant.
The intervention group received more general practitioner consultations (p = 0.04), but there was no difference at 180 days or for visits to the emergency service doctor at 30 and 180 days (see Table III). The intervention and control groups had similar mortality at 30 and 180 days.
Per-protocol analysis showed the same conclusion as intention-to-treat analyses of no difference in readmission and mortality between groups. However, there was evidence that a lower proportion of patients who received a visit by the general practitioner were readmitted within 30 days compared with the control group (20.1% versus 23.4%) (not shown). These differences were not significant.
The intervention group had more referred nursing services in the month after discharge and one to six months after discharge (p < 0.0001), but the mean number of referred minutes among those receiving nursing services was significantly lower (see Table III). More patients in the intervention group were referred to home care one to six months after discharge, and there was a trend towards a lower mean number of referred minutes (p = 0.10).
Discussion
This randomized real-world controlled trial comparing municipality-based post-discharge follow-up visits by a general practitioner and a municipal nurse versus usual care among high-risk older people discharged from a department of internal medicine had no benefits in term of the primary outcome of readmission within 30 days. No other secondary outcomes differed significantly except that more patients in the intervention group than the control group received municipal nursing services. This municipality-based follow-up intervention was only implemented in half the planned visits.
Comparison with previous literature
Several intervention studies have reported effects of hospital discharge planning [8–14] on hospital readmissions, primary care, prescription errors, and quality of life among older people and people with chronic disease. Community-based disease management programmes significantly reduced readmission among people with specific chronic diseases, whereas interventions had no effect on readmission among older people [17,18]. Our results on readmission are consistent with these results, and another meta-analysis reported that regular home visits to frail older people do not influence hospital readmission [19].
Another study in Denmark by Rytter and colleagues reported that similar systematic post-discharge support and effort resulted in better coordination and coherence in treatment and reduced readmission [21]. The study was smaller and the proportion of home visits carried out was markedly higher (93%) than in our study. Furthermore they included only general practitioners who volunteered to participate in the study and these general practitioners led the intervention [21]. In contrast, in our study, we included all general practitioners in the three municipalities and the intervention was led by the municipality.
Strengths and limitations
Our study has several strengths, including: randomizing patients with a similar distribution of baseline covariates; blinding hospital doctors who screened patients for the trial by assessing screening criteria towards randomization status; collecting complete register-based follow-up information for all patients; and blinding researchers’ analysis and interpretation of data towards randomization status. Few eligible patients refused to participate (18%). A further strength is the pragmatic design conducted in a real-world set-up.
The study had limitations. First, by its nature the intervention could not be blinded for the patients, the municipal nurses, or the general practitioners. Second, the proportion of patients (55%) who received the home visit in the intervention group limits the ability to study the effect of home visits. This also highlights that the implementation proportion may not be higher in a real-world set-up, e.g. compared with the study by Rytter and colleagues [21] and stresses the importance of implementation research. Third, the screening tool was not validated but based on previous studies of risk factors for readmission. Finally, the primary outcome was readmissions in general, which is an unspecific outcome. The same results were observed for unplanned readmissions and for readmissions at departments of internal medicine.
Meaning of the study
Our study reflects everyday clinical practice by hospital personnel, general practitioners, or municipal nurses. For the intervention group, 55% of the patients received the home visit. The main reason for cancelling the visits was that the general practitioner did not think they were relevant (23% of the patients in the intervention group) because the patient may have seemed too healthy to benefit from the home visit [27]. Some general practitioners noted that visiting patients who could come to the medical practice by themselves was demotivating. The control group probably comprises many of the same patients, because the number of consultations was only slightly higher in the intervention group (see Table III). This could reflect unintended crossover of the intervention group to the control group.
The screening tool for the trial may not be precise enough to make the home visit relevant in the primary care sector. Some patients younger than 65 years may have benefited from home visits because of complicated disease status or treatments. Further, patients may appear in a different state during admission than when they are back in their customary surroundings. The screening tool was not validated but was based on professional assessment (doctors and nurses from both primary and hospital sectors). About 23% of the patients were readmitted within 30 days and 52% within 180 days (see Table III), which, however, supports that the screening did distinguish a patient group at high risk of readmission.
Several barriers to the implementation of the intervention should be highlighted [27,28]: (i) the communication, e.g. transmission of information between and across the three sectors (hospital, municipality, and general practitioner) was suboptimal despite the great potential for such knowledge sharing; (ii) the assessment of the intervention differed between the involved professions, in particular the attitude of general practitioners greatly influenced the intervention; (iii) the practical organization of the visits, e.g. the demand for a joint visit by a municipal nurse and general practitioner; and (iv) the uncertainty as to whether the screening tool was sensitive and specific in identifying those patients at highest risk of readmission. Each of these barriers may have influenced the relatively low proportion of patients receiving the visits.
The only significant differences between the intervention and control groups were that more intervention patients received municipal nursing services but those receiving services received shorter visits (see Table III). Thus, the intervention group may have received higher-quality municipal care, since more received appropriate services, reflecting a more relevant and tailored service level.
Implications for future research
Hospital readmission is not the most important patient-related outcome of health care [17]. Even if a given intervention fails to reduce readmission rates, continuing implementation may still improve other patient outcomes, such as mortality, satisfaction with care, and cost-effectiveness [17]. Further, the assumption that readmission rates reflect patient well-being may be erroneous.
Implementation fidelity (the degree to which an intervention or programme is delivered as intended) is an important moderator between the intervention and the intended outcome. In some cases, the lack of implementation fidelity probably resulted from medical assessment and setting priorities [27–29], but knowledge is lacking on the mechanism that moderates the extent of implementation fidelity in complex cross-sectorial interventions.
This randomized pragmatic controlled trial comparing municipality-based post-discharge follow- up visits with usual care among high-risk older people reported no effect on the primary outcome of readmission within 30 days.
Acknowledgement
The authors would like to thank the following members of the Prevention of Early Readmission Research Group: Peter Schou, general practitioner, Holbæk, Denmark; Natasha Georgieva Roseva-Nielsen, Chief Physician, Department of Internal Medicine, Holbæk University Hospital, Denmark; Gerda Pedersen, Medical Officer, Municipality of Holbæk, Denmark; Lia Clemensen, District Manager, Municipality of Holbæk, Denmark; Jytte Hykkelbjerg Bruhn, Nurse, Department of Internal Medicine, Holbæk University Hospital, Denmark; Inge Jekes, Nurse and Development Consultant, Municipality of Kalundborg, Denmark; Lone Haagensen, Quality Management Nurse, Department of Internal Medicine, Holbæk University Hospital, Denmark; Anette Rise, Team Leader, Municipality of Odsherred, Denmark; Vivi Kenhof, Medical Officer, Municipality of Odsherred, Denmark; Henrik Ancher Sørensen, Department of Internal Medicine, Holbæk University Hospital, Denmark; and Knut Borch-Johnsen, Assistant General Manager, Holbæk University Hospital, Denmark.
Funding
The Fund for Intersectoral Projects in Region Zealand, Denmark funded the project in 2011 and 2012. The funding agency had no influence on the analyses and interpretation of the results.
Ethical approval
Regulatory and research ethics committee approvals were obtained from the Danish Data Protection Agency (J.nr. 2011-52-0267) and the Regional Research Ethical Committee (J.nr. 1-01-83-002-07).
Trial registration
The trial was registered at Trial.com: Clinicaltrials.gov ID NCT02094040.
Data sharing
A technical appendix, the statistical code, and an anonymized aggregated dataset are available from the epidemiologist who was responsible for all the blinded statistical analysis at lct@niph.dk. Consent was not obtained for data sharing, but the data presented were anonymized in accordance with the Act on Processing of Personal Data and the risk of identifying individuals is low.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- Centers for Disease Control and Prevention Trends in aging: United States and worldwide. MMWR Morb Mortal Wkly Rep 2003;52:101–4. [PubMed] [Google Scholar]
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: The challenges ahead. Lancet 2009; 374:1196–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell SE, Seymour DG, Primrose WR. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing 2004;33:110–15. [DOI] [PubMed] [Google Scholar]
- Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 2003;18:646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frydenberg K, Brekke M. Poor communication on patients ’ medication across health care levels leads to potentially harmful medication errors. Scand J Prim Health Care 2012;30:234–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. JAMA 2007;297:831–41. [DOI] [PubMed] [Google Scholar]
- Huntley AL, Thomas R, Mann M, Huws D, Elwyn G, Paranjothy S, et al. . Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract 2013; 30:266–75. [DOI] [PubMed] [Google Scholar]
- Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: A randomized controlled study. J Gen Intern Med 2008;23:1228–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans RL, Hendricks RD. Evaluating hospital discharge planning: A randomized clinical trial. Med Care 1993;31:358–70. [DOI] [PubMed] [Google Scholar]
- Hendriksen C, Stromgard E, Sorensen KH. Hospitalization of elderly people: A 3-year controlled trial. J Am Geriatr Soc 1989;37:117–22. [DOI] [PubMed] [Google Scholar]
- Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE et al. . A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med 2009;150:178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: A randomized controlled trial. Arch Intern Med 2003;163:809–17. [DOI] [PubMed] [Google Scholar]
- Legrain S, Tubach F, Bonnet-Zamponi D, Lemaire A, Aquino JP, Paillaud E, et al. . A new multimodal geriatric discharge- planning intervention to prevent emergency visits and rehospitalizations of older adults: The optimization of medication in AGEd multicenter randomized controlled trial. J Am Geriatr Soc 2011;59:2017–28. [DOI] [PubMed] [Google Scholar]
- Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: A randomized clinical trial. Ann Intern Med 1994;120:999–1006. [DOI] [PubMed] [Google Scholar]
- Bolas H, Brookes K, Scott M, McElnay J. Evaluation of a hospital-based community liaison pharmacy service in Northern Ireland. Pharm World Sci 2004;26:114–20. [DOI] [PubMed] [Google Scholar]
- Eggink RN, Lenderink AW, Widdershoven JW, van den Bemt PM. The effect of a clinical pharmacist discharge service on medication discrepancies in patients with heart failure. Pharm World Sci 2010;32:759–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benbassat J, Taragin MI. The effect of clinical interventions on hospital readmissions: A meta-review of published meta-analyses. Isr J Health Policy Res 2013;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda A, Taylor SJC, Taylor RS, Khan F, Krum H, Underwood M. Clinical service organisation for heart failure. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No. CD002752. [DOI] [PubMed] [Google Scholar]
- Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, et al. . Effectiveness of home based support for older people: Systematic review and meta-analysis. BMJ 2001; 323:719–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K. Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern Med 2014;174:1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rytter L, Jakobsen HN, Ronholt F, Hammer AV, Andreasen AH, Nissen A, et al. . Comprehensive discharge follow-up in patients’ homes by GPs and district nurses of elderly patients: A randomized controlled trial. Scand J Prim Health Care 2010;28:146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J, et al. . Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet 2008; 371:725–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39(7 Suppl):30–3. [DOI] [PubMed] [Google Scholar]
- Pedersen CB. The Danish civil registration system. Scand J Public Health 2011;39(7 Suppl):22–5. [DOI] [PubMed] [Google Scholar]
- Andersen JS, Olivarius NF, Krasnik A. The Danish National Health Service Register. Scand J Public Health 2011;39(7 Suppl):34–7. [DOI] [PubMed] [Google Scholar]
- Fokdal S, Sørensen SK, Al-Najer A. Implementering af opfølgende hjemmebesøg i 9 kommuner i Region Sjælland [Implementation of follow-up home visits in 9 municipalities in Region Zealand, Denmark]. Holbæk: Municipality of Holbæk; 2013. [Google Scholar]
- Lehn SF, Rod MH, Thygesen LC, Zwisler A-D. Implementering af opfølgende hjemmebesøg i Region Sjælland [Implementation of follow-up home visits in Region Zealand]. Copenhagen: National Institute of Public Health, University of Southern Denmark; 2014. [Google Scholar]
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2:40. [DOI] [PMC free article] [PubMed] [Google Scholar]