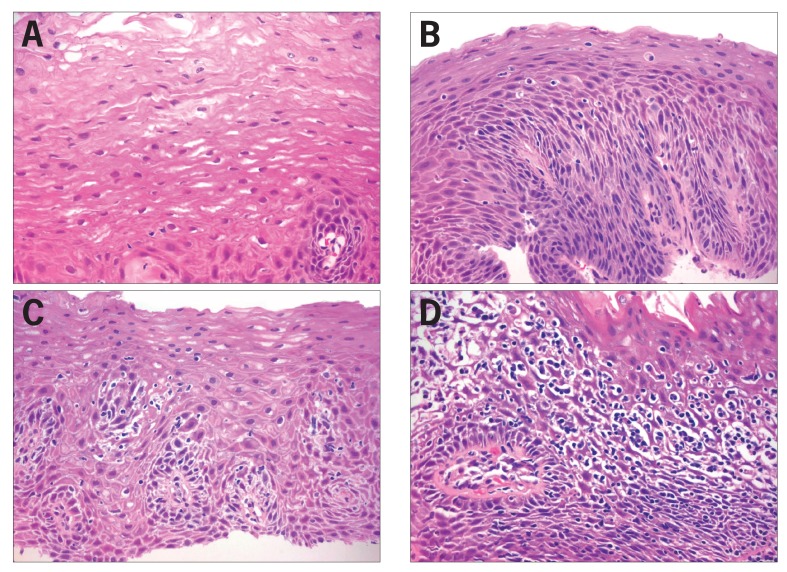
Figure 2.
Histopathologic findings.
(A) Normal esophageal mucosa. Nonkeratinizing stratified squamous epithelium is comprised of large polygonal eosinophilic cells, arising from a basal cell layer of cuboidal basophilic cells. The lower border of the squamous epithelium is irregular due to folds of the lamina propria housing fibrovascular cores (papillae). The basal zone normally occupies less than 15% of the thickness of the epithelium, whereas the lamina propria papillae normally project to no more than half of the thickness. The cell-to-cell borders are indistinct above the basal layer, and there are no inflammatory cells present. (400× magnification, hematoxylin and eosin stain.)
(B) Gastroesophageal reflux disease. Active esophagitis is shown with rare neutrophils and scattered intraepithelial lymphocytes, basal cell hyperplasia (>15% mucosal thickness), elongation of the lamina propria papillae, impaired surface maturation, and minimal intercellular edema. (400× magnification, hematoxylin and eosin stain.)
(C) Mild lymphocytic esophagitis. Increased intraepithelial lymphocytes, predominately peripapillary, and spongiosis of the peripapillary and basal zone intercellular spaces can be seen. Neither neutrophils nor basal cell hyperplasia are present. (400× magnification, hematoxylin and eosin stain.)
(D) Marked lymphocytic esophagitis. The mucosal architecture is almost completely obscured by marked spongiosis and basal and peripapillary intraepithelial lymphocytosis. No neutrophils are seen. (400× magnification, hematoxylin and eosin stain.)
Reproduced from Dunbar KB, Ayyar B, Spechler SJ, Genta R, Melton S. Clinical, endoscopic and histological features of patients with lymphocytic esophagitis compared to patients with GERD. Poster presented at: 45th Annual Digestive Disease Week; May 3-6, 2014; Chicago, IL. Abstract Mo1846.