Abstract
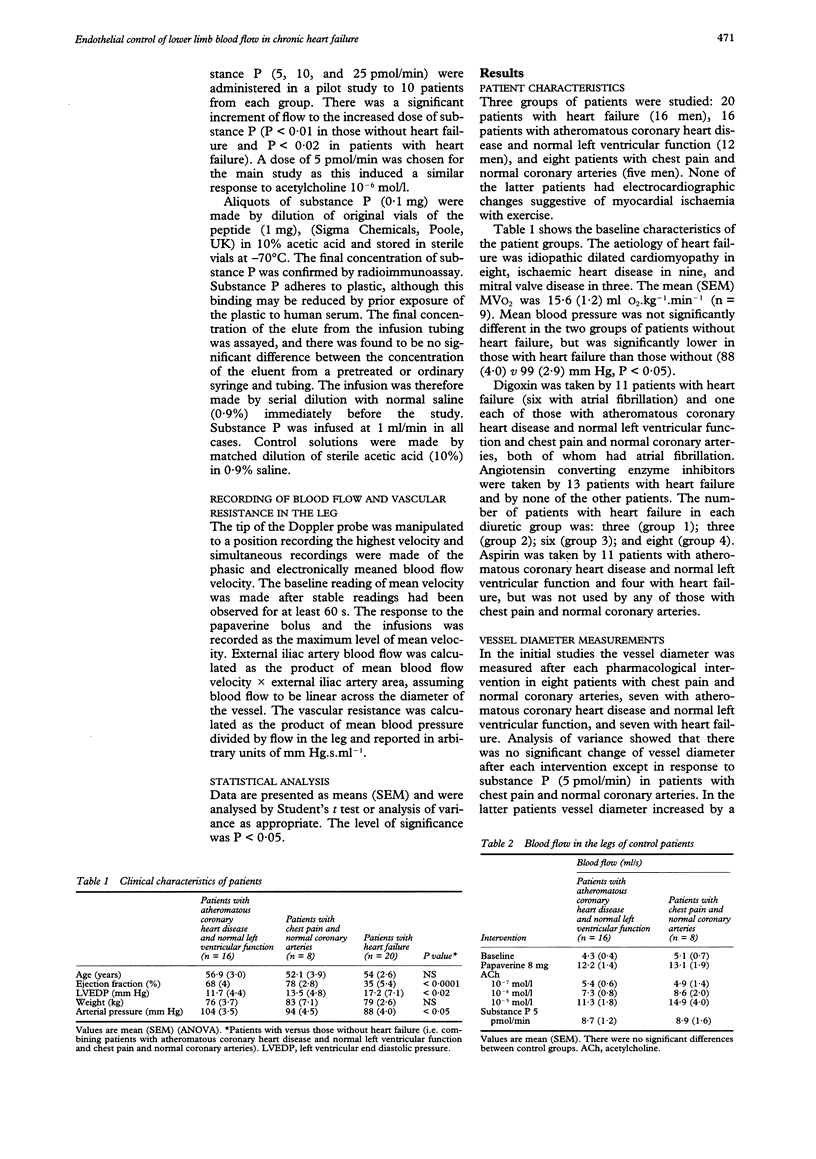
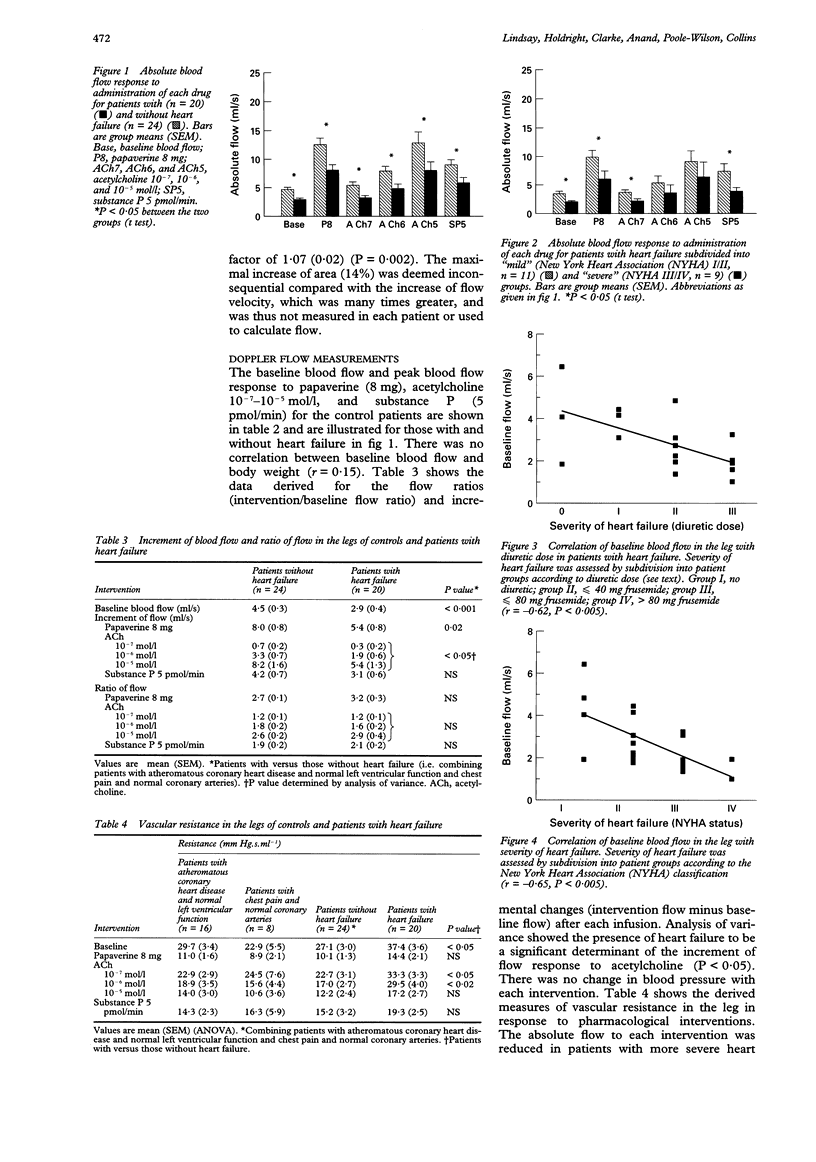
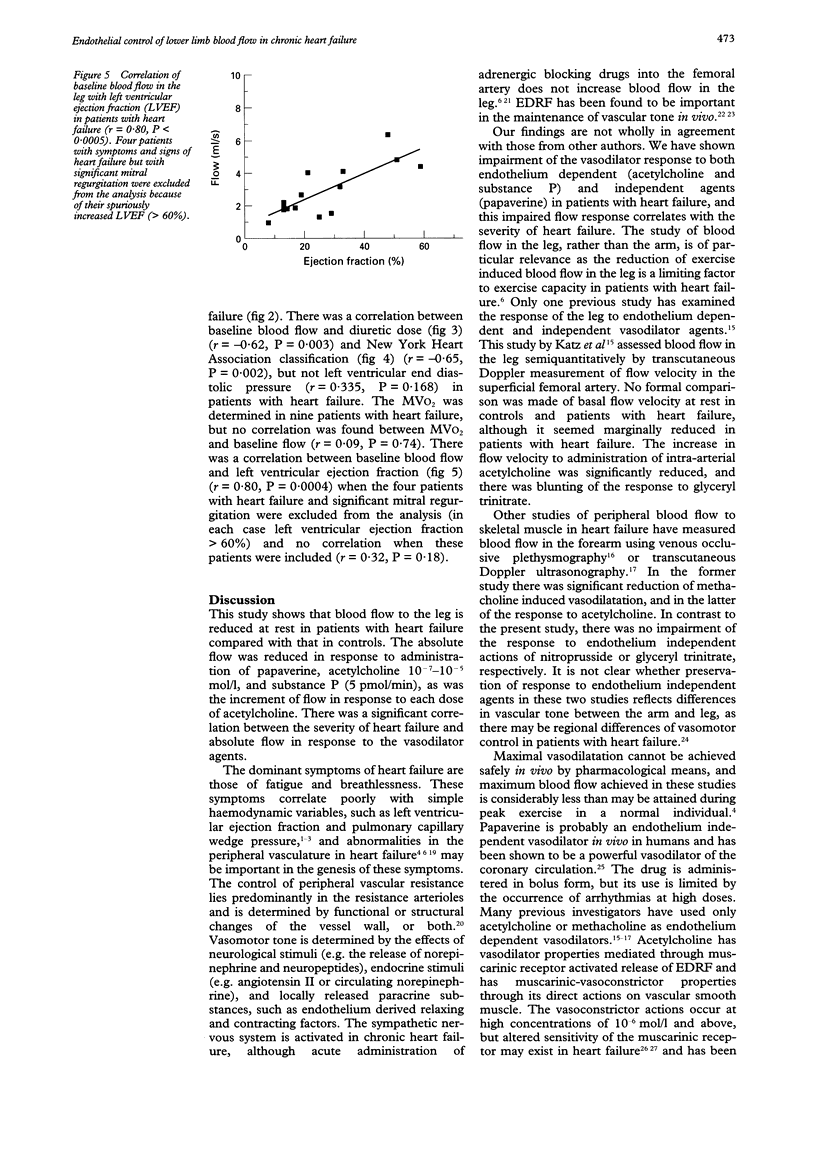
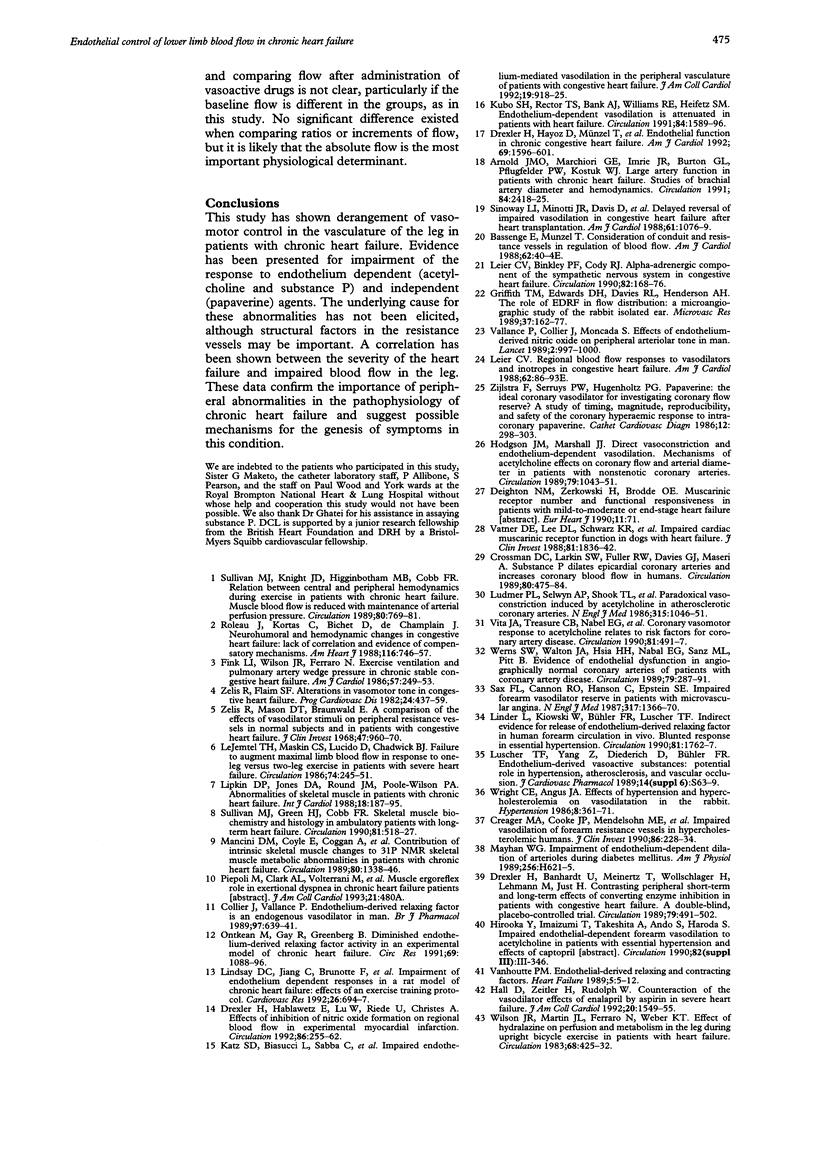
BACKGROUND: Limitation of the blood supply to skeletal muscle in chronic heart failure may contribute to the symptoms of fatigue and diminished exercise capacity. The pathophysiology underlying this abnormality is not known. The purpose of this study was to assess the effect of endothelium dependent and independent vasodilator agents on blood flow in the leg of patients with heart failure. METHODS AND RESULTS: Blood flow in the leg was measured in patients with heart failure (n = 20) and compared with that in patients with ischaemic heart disease and normal left ventricular function (n = 16) and patients with chest pain and normal coronary arteries (n = 8). External iliac artery blood flow was measured using intravascular Doppler ultrasound and quantitative angiography. Flow was recorded at rest and in response to bolus doses of the endothelium independent vasodilator, papaverine. Endothelium dependent responses were measured by infusion of acetylcholine and substance P. Mean (SEM) baseline blood flow was reduced at rest (2.9 (0.4) v 4.5 (0.3) ml/s, P < 0.001) and vascular resistance was raised (37.4 (3.6) v 27.1 (3.0) units, P < 0.05) in patients with heart failure compared with that in controls. The peak blood flow response to papaverine (8 mg), acetylcholine (10(-7)-10(-5) mol/l), and substance P (5 pmol/min) was reduced in heart failure, with greater impairment of the response to acetylcholine than substance P. There was a correlation between baseline blood flow in the heart failure group and diuretic dose (r = -0.62, P = 0.003), New York Heart Association classification (r = -0.65, P = 0.002), and left ventricular ejection fraction (r = 0.80, P = 0.0004). CONCLUSIONS: There is reduced blood flow and raised vascular resistance at rest in the legs of patients with heart failure. The degree of impaired blood flow in the leg correlates with the severity of heart failure. There is impairment of the response to both endothelium dependent and independent vasodilators. Abnormal function of the vascular myocyte in heart failure may explain these results as would structural abnormalities of the resistance vessels.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnold J. M., Marchiori G. E., Imrie J. R., Burton G. L., Pflugfelder P. W., Kostuk W. J. Large artery function in patients with chronic heart failure. Studies of brachial artery diameter and hemodynamics. Circulation. 1991 Dec;84(6):2418–2425. doi: 10.1161/01.cir.84.6.2418. [DOI] [PubMed] [Google Scholar]
- Creager M. A., Cooke J. P., Mendelsohn M. E., Gallagher S. J., Coleman S. M., Loscalzo J., Dzau V. J. Impaired vasodilation of forearm resistance vessels in hypercholesterolemic humans. J Clin Invest. 1990 Jul;86(1):228–234. doi: 10.1172/JCI114688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crossman D. C., Larkin S. W., Fuller R. W., Davies G. J., Maseri A. Substance P dilates epicardial coronary arteries and increases coronary blood flow in humans. Circulation. 1989 Sep;80(3):475–484. doi: 10.1161/01.cir.80.3.475. [DOI] [PubMed] [Google Scholar]
- Drexler H., Banhardt U., Meinertz T., Wollschläger H., Lehmann M., Just H. Contrasting peripheral short-term and long-term effects of converting enzyme inhibition in patients with congestive heart failure. A double-blind, placebo-controlled trial. Circulation. 1989 Mar;79(3):491–502. doi: 10.1161/01.cir.79.3.491. [DOI] [PubMed] [Google Scholar]
- Drexler H., Hablawetz E., Lu W., Riede U., Christes A. Effects of inhibition of nitric oxide formation on regional blood flow in experimental myocardial infarction. Circulation. 1992 Jul;86(1):255–262. doi: 10.1161/01.cir.86.1.255. [DOI] [PubMed] [Google Scholar]
- Drexler H., Hayoz D., Münzel T., Hornig B., Just H., Brunner H. R., Zelis R. Endothelial function in chronic congestive heart failure. Am J Cardiol. 1992 Jun 15;69(19):1596–1601. doi: 10.1016/0002-9149(92)90710-g. [DOI] [PubMed] [Google Scholar]
- Dzau V. J., Swartz S. L. Dissociation of the prostaglandin and renin angiotensin systems during captopril therapy for chronic congestive heart failure secondary to coronary artery disease. Am J Cardiol. 1987 Nov 1;60(13):1101–1105. doi: 10.1016/0002-9149(87)90361-4. [DOI] [PubMed] [Google Scholar]
- Fink L. I., Wilson J. R., Ferraro N. Exercise ventilation and pulmonary artery wedge pressure in chronic stable congestive heart failure. Am J Cardiol. 1986 Feb 1;57(4):249–253. doi: 10.1016/0002-9149(86)90900-8. [DOI] [PubMed] [Google Scholar]
- Griffith T. M., Edwards D. H., Davies R. L., Henderson A. H. The role of EDRF in flow distribution: a microangiographic study of the rabbit isolated ear. Microvasc Res. 1989 Mar;37(2):162–177. doi: 10.1016/0026-2862(89)90035-6. [DOI] [PubMed] [Google Scholar]
- Hall D., Zeitler H., Rudolph W. Counteraction of the vasodilator effects of enalapril by aspirin in severe heart failure. J Am Coll Cardiol. 1992 Dec;20(7):1549–1555. doi: 10.1016/0735-1097(92)90449-w. [DOI] [PubMed] [Google Scholar]
- Hodgson J. M., Marshall J. J. Direct vasoconstriction and endothelium-dependent vasodilation. Mechanisms of acetylcholine effects on coronary flow and arterial diameter in patients with nonstenotic coronary arteries. Circulation. 1989 May;79(5):1043–1051. doi: 10.1161/01.cir.79.5.1043. [DOI] [PubMed] [Google Scholar]
- Jorfeldt L., Wahren J. Leg blood flow during exercise in man. Clin Sci. 1971 Nov;41(5):459–473. doi: 10.1042/cs0410459. [DOI] [PubMed] [Google Scholar]
- Kaiser L., Spickard R. C., Olivier N. B. Heart failure depresses endothelium-dependent responses in canine femoral artery. Am J Physiol. 1989 Apr;256(4 Pt 2):H962–H967. doi: 10.1152/ajpheart.1989.256.4.H962. [DOI] [PubMed] [Google Scholar]
- Katz S. D., Biasucci L., Sabba C., Strom J. A., Jondeau G., Galvao M., Solomon S., Nikolic S. D., Forman R., LeJemtel T. H. Impaired endothelium-mediated vasodilation in the peripheral vasculature of patients with congestive heart failure. J Am Coll Cardiol. 1992 Apr;19(5):918–925. doi: 10.1016/0735-1097(92)90271-n. [DOI] [PubMed] [Google Scholar]
- Kubo S. H., Rector T. S., Bank A. J., Williams R. E., Heifetz S. M. Endothelium-dependent vasodilation is attenuated in patients with heart failure. Circulation. 1991 Oct;84(4):1589–1596. doi: 10.1161/01.cir.84.4.1589. [DOI] [PubMed] [Google Scholar]
- LeJemtel T. H., Maskin C. S., Lucido D., Chadwick B. J. Failure to augment maximal limb blood flow in response to one-leg versus two-leg exercise in patients with severe heart failure. Circulation. 1986 Aug;74(2):245–251. doi: 10.1161/01.cir.74.2.245. [DOI] [PubMed] [Google Scholar]
- Levine B., Kalman J., Mayer L., Fillit H. M., Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med. 1990 Jul 26;323(4):236–241. doi: 10.1056/NEJM199007263230405. [DOI] [PubMed] [Google Scholar]
- Linder L., Kiowski W., Bühler F. R., Lüscher T. F. Indirect evidence for release of endothelium-derived relaxing factor in human forearm circulation in vivo. Blunted response in essential hypertension. Circulation. 1990 Jun;81(6):1762–1767. doi: 10.1161/01.cir.81.6.1762. [DOI] [PubMed] [Google Scholar]
- Lindsay D. C., Jiang C., Brunotte F., Adamopoulos S., Coats A. J., Rajagopalan B., Poole-Wilson P. A., Collins P. Impairment of endothelium dependent responses in a rat model of chronic heart failure: effects of an exercise training protocol. Cardiovasc Res. 1992 Jul;26(7):694–697. doi: 10.1093/cvr/26.7.694. [DOI] [PubMed] [Google Scholar]
- Lipkin D. P., Jones D. A., Round J. M., Poole-Wilson P. A. Abnormalities of skeletal muscle in patients with chronic heart failure. Int J Cardiol. 1988 Feb;18(2):187–195. doi: 10.1016/0167-5273(88)90164-7. [DOI] [PubMed] [Google Scholar]
- Ludmer P. L., Selwyn A. P., Shook T. L., Wayne R. R., Mudge G. H., Alexander R. W., Ganz P. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986 Oct 23;315(17):1046–1051. doi: 10.1056/NEJM198610233151702. [DOI] [PubMed] [Google Scholar]
- Lüscher T. F., Yang Z. H., Diederich D., Bühler F. R. Endothelium-derived vasoactive substances: potential role in hypertension, atherosclerosis, and vascular occlusion. J Cardiovasc Pharmacol. 1989;14 (Suppl 6):S63–S69. [PubMed] [Google Scholar]
- Mancini D. M., Coyle E., Coggan A., Beltz J., Ferraro N., Montain S., Wilson J. R. Contribution of intrinsic skeletal muscle changes to 31P NMR skeletal muscle metabolic abnormalities in patients with chronic heart failure. Circulation. 1989 Nov;80(5):1338–1346. doi: 10.1161/01.cir.80.5.1338. [DOI] [PubMed] [Google Scholar]
- Mayhan W. G. Impairment of endothelium-dependent dilatation of cerebral arterioles during diabetes mellitus. Am J Physiol. 1989 Mar;256(3 Pt 2):H621–H625. doi: 10.1152/ajpheart.1989.256.3.H621. [DOI] [PubMed] [Google Scholar]
- McMurray J. J., Ray S. G., Abdullah I., Dargie H. J., Morton J. J. Plasma endothelin in chronic heart failure. Circulation. 1992 Apr;85(4):1374–1379. doi: 10.1161/01.cir.85.4.1374. [DOI] [PubMed] [Google Scholar]
- Ontkean M., Gay R., Greenberg B. Diminished endothelium-derived relaxing factor activity in an experimental model of chronic heart failure. Circ Res. 1991 Oct;69(4):1088–1096. doi: 10.1161/01.res.69.4.1088. [DOI] [PubMed] [Google Scholar]
- Reibel D. K., O'Rourke B., Foster K. A., Hutchinson H., Uboh C. E., Kent R. L. Altered phospholipid metabolism in pressure-overload hypertrophied hearts. Am J Physiol. 1986 Jan;250(1 Pt 2):H1–H6. doi: 10.1152/ajpheart.1986.250.1.H1. [DOI] [PubMed] [Google Scholar]
- Rouleau J. L., Kortas C., Bichet D., de Champlain J. Neurohumoral and hemodynamic changes in congestive heart failure: lack of correlation and evidence of compensatory mechanisms. Am Heart J. 1988 Sep;116(3):746–757. doi: 10.1016/0002-8703(88)90333-x. [DOI] [PubMed] [Google Scholar]
- Sax F. L., Cannon R. O., 3rd, Hanson C., Epstein S. E. Impaired forearm vasodilator reserve in patients with microvascular angina. Evidence of a generalized disorder of vascular function? N Engl J Med. 1987 Nov 26;317(22):1366–1370. doi: 10.1056/NEJM198711263172202. [DOI] [PubMed] [Google Scholar]
- Sinoway L. I., Minotti J. R., Davis D., Pennock J. L., Burg J. E., Musch T. I., Zelis R. Delayed reversal of impaired vasodilation in congestive heart failure after heart transplantation. Am J Cardiol. 1988 May 1;61(13):1076–1079. doi: 10.1016/0002-9149(88)90129-4. [DOI] [PubMed] [Google Scholar]
- Sullivan M. J., Green H. J., Cobb F. R. Skeletal muscle biochemistry and histology in ambulatory patients with long-term heart failure. Circulation. 1990 Feb;81(2):518–527. doi: 10.1161/01.cir.81.2.518. [DOI] [PubMed] [Google Scholar]
- Sullivan M. J., Knight J. D., Higginbotham M. B., Cobb F. R. Relation between central and peripheral hemodynamics during exercise in patients with chronic heart failure. Muscle blood flow is reduced with maintenance of arterial perfusion pressure. Circulation. 1989 Oct;80(4):769–781. doi: 10.1161/01.cir.80.4.769. [DOI] [PubMed] [Google Scholar]
- Vallance P., Collier J., Moncada S. Effects of endothelium-derived nitric oxide on peripheral arteriolar tone in man. Lancet. 1989 Oct 28;2(8670):997–1000. doi: 10.1016/s0140-6736(89)91013-1. [DOI] [PubMed] [Google Scholar]
- Vatner D. E., Lee D. L., Schwarz K. R., Longabaugh J. P., Fujii A. M., Vatner S. F., Homcy C. J. Impaired cardiac muscarinic receptor function in dogs with heart failure. J Clin Invest. 1988 Jun;81(6):1836–1842. doi: 10.1172/JCI113528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vita J. A., Treasure C. B., Nabel E. G., McLenachan J. M., Fish R. D., Yeung A. C., Vekshtein V. I., Selwyn A. P., Ganz P. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation. 1990 Feb;81(2):491–497. doi: 10.1161/01.cir.81.2.491. [DOI] [PubMed] [Google Scholar]
- Werns S. W., Walton J. A., Hsia H. H., Nabel E. G., Sanz M. L., Pitt B. Evidence of endothelial dysfunction in angiographically normal coronary arteries of patients with coronary artery disease. Circulation. 1989 Feb;79(2):287–291. doi: 10.1161/01.cir.79.2.287. [DOI] [PubMed] [Google Scholar]
- Wilson J. R., Ferraro N., Wiener D. H. Effect of the sympathetic nervous system on limb circulation and metabolism during exercise in patients with heart failure. Circulation. 1985 Jul;72(1):72–81. doi: 10.1161/01.cir.72.1.72. [DOI] [PubMed] [Google Scholar]
- Wilson J. R., Martin J. L., Ferraro N., Weber K. T. Effect of hydralazine on perfusion and metabolism in the leg during upright bicycle exercise in patients with heart failure. Circulation. 1983 Aug;68(2):425–432. doi: 10.1161/01.cir.68.2.425. [DOI] [PubMed] [Google Scholar]
- Wright C. E., Angus J. A. Effects of hypertension and hypercholesterolemia on vasodilatation in the rabbit. Hypertension. 1986 May;8(5):361–371. doi: 10.1161/01.hyp.8.5.361. [DOI] [PubMed] [Google Scholar]
- Zelis R., Delea C. S., Coleman H. N., Mason D. T. Arterial sodium content in experimental congestive heart failure. Circulation. 1970 Feb;41(2):213–216. doi: 10.1161/01.cir.41.2.213. [DOI] [PubMed] [Google Scholar]
- Zelis R., Flaim S. F. Alterations in vasomotor tone in congestive heart failure. Prog Cardiovasc Dis. 1982 May-Jun;24(6):437–459. doi: 10.1016/0033-0620(82)90012-3. [DOI] [PubMed] [Google Scholar]
- Zelis R., Lee G., Mason D. T. Influence of experimental edema on metabolically determined blood flow. Circ Res. 1974 Apr;34(4):482–490. doi: 10.1161/01.res.34.4.482. [DOI] [PubMed] [Google Scholar]
- Zelis R., Mason D. T., Braunwald E. A comparison of the effects of vasodilator stimuli on peripheral resistance vessels in normal subjects and in patients with congestive heart failure. J Clin Invest. 1968 Apr;47(4):960–970. doi: 10.1172/JCI105788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelis R., Mason D. T. Diminished forearm arteriolar dilator capacity produced by mineralocorticoid-induced salt retention in man. Implications concerning congestive heart failure and vascular stiffness. Circulation. 1970 Apr;41(4):589–592. doi: 10.1161/01.cir.41.4.589. [DOI] [PubMed] [Google Scholar]
- Zijlstra F., Serruys P. W., Hugenholtz P. G. Papaverine: the ideal coronary vasodilator for investigating coronary flow reserve? A study of timing, magnitude, reproducibility, and safety of the coronary hyperemic response after intracoronary papaverine. Cathet Cardiovasc Diagn. 1986;12(5):298–303. doi: 10.1002/ccd.1810120505. [DOI] [PubMed] [Google Scholar]


