Abstract
Introduction:
Most greater tuberosity humerus fractures can be treated successfully with either surgical or conservative methods and good results can be expected if fracture heals anatomically but a displaced fracture or an improperly reduced fracture can lead to a symptomatic mal-union.
Case Presentation:
36years old man with mal-united greater tuberosity fracture presented to us 18 months following injury and percutaneous screw fixation and 9 months after screw removal. She complained of severe restriction of shoulder movements. A good result was achieved after corrective open reduction and fixation of the greater tuberosity and rotator cuff repair.
Conclusion:
Open reduction, re-fixation and soft tissue reconstruction can give excellent results in cases of malunited greater tuberosity fractures even as late as 20 months after trauma.
Keywords: Malunited greater tuberosity, Rotator cuff repair, Open reduction
INTRODUCTION:
Isolated greater tuberosity humerus fractures are rare with less than 100 cases reported till 2008 [1]. Very little agreement exists in literature regarding classification and management of these fractures [2]. Generally accepted norm is that fractures with displacement less than 5 mm should be treated conservatively and results are good [1,3]. In cases with displaced greater tuberosity fractures, shoulder function may be impaired due to impingement of superiorly and posteriorly displaced tuberosity under the acromion. Rotator cuff dysfunction adds to this impairment [3]. For this reasons reduction and internal fixation of displaced greater tuberosity fractures is advised. Very few cases of redisplacement and malunion after internal fixation of greater tuberosity are reported. These cases have similar impairment due to impingement and present with limitation of movements and rotator cuff dysfunction [4]. Treatment is either open surgery in form of osteotomy and re-reduction of the tuberosity [5-7] or recently arthroscopic management (‘tuberoplasty’) [8-10].
We report a case with failure of primary fixation of a displaced greater tuberosity fracture leading to malunion. Patient presented 18 months after primary surgery with limitation of abduction, forward flexion and external rotation. This was treated with open reduction and re fixation with excellent result
CASE PRESENTATION:
We report the case of a 36 years old man, right hand dominant manual worker. He fell in June 2005. The initial radiographs showed a displaced greater tuberosity fracture of right humerus. He underwent operative management by a percutaneous technique elsewhere. Unfortunately, the radiographs of primary surgery were not available. Nine months later, the screws were removed. The patient was referred to our center 18 months after the initial injury for further management for loss of motion. Clinical examination revealed no pain, forward active elevation of 50°, no active external rotation and a positive lag sign or Hertel sign [11]. Passive range of motion was preserved except in external rotation with arm by the side of the chest. The computerized tomography showed a partial fusion of the greater tuberosity which was displaced posteriorly and superiorly (Fig. 1). The sagittal images demonstrated fatty infiltration in supraspinatus stage 2 [12,13].
Figure 1.
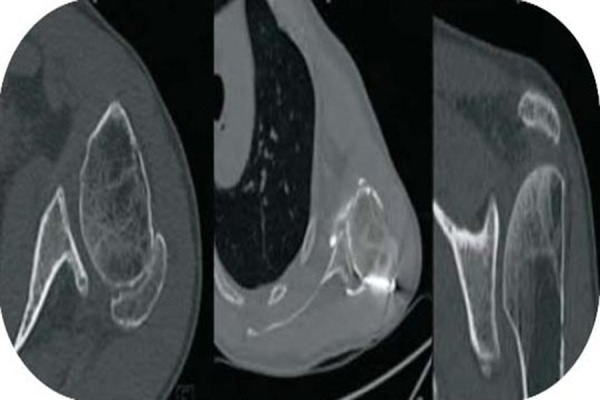
CT scan images showing posteriorly displaced tuberosity fracture
We operated 20 months after the initial injury through posterior approach. The greater tuberosity fixed with 3 cancellous screws (Fig. 2). The supraspinatus tear was repaired through the same approach using 5mm titanium anchor (Fig. 2). Post operatively the patient was managed in a sling with 60° of abduction for 6 weeks and the rehabilitation was started 4 weeks after surgery.
Figure 2.

Radiograph of the shoulder showing fusion of the tuberosity fragment at 2 years post re-fixation.
Two years after surgery patient was pain free, range of movement & rotator cuff strength was normal when compared to opposite side. Patient was able to do all manual work which he did before sustaining fracture (Fig. 3). Radiograph at 2 years follow up shows that the fracture has healed well with all 3 screws and an anchor insitu.
Figure 3.

Clinical photograph of the incision (A), and functional outcome of the patient at 2 years follow up (B & C)
DISCUSSION:
The treatment of proximal humeral fractures has been standardized and there are several studies of outcome following proximal humerus fractures, but the management of proximal humerus fracture complications is not well studied, especially the most common, greater tuberosity fracture mal-union [14].
The greater tuberosity is an important component of sub acromial gliding mechanism and serves as the major insertion for the rotator cuff, a dynamic stabilizer of the joint [15,16]. Greater tuberosity fractures are usually displaced superiorly and posteriorly due to pull of supraspinatus, infraspinatus & teres minor muscles. A posteriorly mal-united fracture can act as block to limit external rotation. A superiorly displaced greater tuberosity can block abduction and forward elevation and cause subacromial impingement [17]. These mal-unions can cause rotator cuff weakness, either by shortening the musculo-tendinous length of cuff muscles or the sub-acromial impingement which can lead to cuff attrition and tears or by effects of altered biomechanics of the shoulder due to malunited greater tuberosity. Bono et al [18] in their biomechanical study showed the effect of displaced greater tuberosity on the deltoid abduction force, abduction force was significantly decreased by 16% & 27% by superior displacement of greater tuberosity by 0.5cm and 1cm respectively and in case of posterosuperior displacement of 1cm abduction force was decreased by 29%. With postero superior displacement, the central axis of pull of supraspinatus is translated posterior to the central axis of humeral head, this may account for the further decrease in abduction forces. Hence, it is always important to evaluate the integrity and efficacy of cuff muscles [7].
Management of greater tuberosity mal-unions is determined by size of tuberosity fragments and degree of displacement. A minimally displaced malunion of 5mm or less can be excised and rotator cuff repaired back to bone with suture anchors or an isolated acromioplasty. If the fragment is more than 5mm or larger an osteotomy of greater tuberosity is necessary. The osteotomy can be performed through a deltopectoral approach or anterosuperior approach as described by Craig [19]. The tuberosity can be reshaped and fixed with 4.5mm cancellous screws. In some instances a capsular release and sub deltoid release may be necessary in addition, however because of rarity of this presentation a standard surgical procedure for a posteriorly mal-united fragment is not yet agreed upon. Morries and colleagues reported on 3 tuberosity mal-unions that underwent osteotomy, forward elevation and external rotation arc were improved up to 60° in their study [20]. Beredjiklian et al treated 8 patients with osteotomy and soft tissue reconstruction and reported 75% satisfactory result with 88% with good pain relief [5]. We used an extensile posterior approach, the greater tuberosity was dissected and reshaped and fixed with three 4.5mm cannulated cancellous screws and tear in the supraspinatus tendon was repaired with a suture anchor. At two years post operatively the patient has regained full range of motion, with no rotator cuff weakness and no pain. He has returned to his manual labor work without limitations. Recently arthroscopic management has been reported, however it is technically demanding [8-10]
CONCLUSION
Better results can be achieved if malunited fragment is osteotomised, reshaped and fixed anatomically. Rotator cuff tear if present needs to addressed and with minimal or no fatty infiltration in rotator cuff, normal strength can be recovered. We report in this case that excellent results can be achieved even as late as 20 months after the injury.
CLINICAL MESSAGE:
Open reduction and re fixation can give good results in malunited greater tuberosity fracture.
Footnotes
Conflict of Interest : NONE
Source of Funding : NONE
REFERENCES
- 1.Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008 Mar;39(3):284–98. doi: 10.1016/j.injury.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Shrader MW, Sanchez-Sotelo J, Sperling JW, Rowland CM, Cofield RH. Understanding proximal humerus fractures: Image analysis, classification, and treatment. J Shoulder Elbow Surg. 2005;14:497–505. doi: 10.1016/j.jse.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 3.George MS. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 2007 Oct;15(10):607–13. doi: 10.5435/00124635-200710000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Bigliani LU, Flatow EL, Pollock RG. Fractures of the proximal humerus. In: Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, editors. Rockwood and Green's Fractures in Adults. 4th ed. Vol. 1. Philadelphia, PA: Lippincott-Raven; 1996. pp. 1055–1107. [Google Scholar]
- 5.Beredjiklian PK, Iannotti JP, Norris TR, Williams GR. Operative treatment of malunion of a fracture of the proximal aspect of the humerus. J Bone Joint Surg Am. 1998 Oct;80(10):1484–97. doi: 10.2106/00004623-199810000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Craig EV. Operative treatment of tuberosity fractures, malunions and nonunions. In: Craig EV, editor. The shoulder. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 495–511. [Google Scholar]
- 7.Siegel J, Dines D. Proximal humerus malunions. Orthop clinics north America. 2000;31(1):35. doi: 10.1016/s0030-5898(05)70126-7. [DOI] [PubMed] [Google Scholar]
- 8.Martinez AA, Calvo A, Domingo J, Cuenca J, Herrera A. Arthroscopic treatment for malunions of the proximal humeral greater tuberosity. Int Orthop. 2010 Dec;34(8):1207–11. doi: 10.1007/s00264-009-0900-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calvo E, Merino-Gutierrez I, Lagunes I. Arthroscopic tuberoplasty for subacromial impingement secondary to proximal humeral malunion. Knee Surg Sports Traumatol Arthrosc. 2010 Jul;18(7):988–91. doi: 10.1007/s00167-009-0939-1. [DOI] [PubMed] [Google Scholar]
- 10.Kim KC, Rhee KJ, Shin HD. Arthroscopic treatment of symptomatic malunion of the greater tuberosity of the humerus using the suture-bridge technique. Orthopedics. 2010 Apr;33(4):242–5. doi: 10.3928/01477447-20100225-13. [DOI] [PubMed] [Google Scholar]
- 11.Hertel R, Ballmer FT, Lambert SM, Gerber C. Lag sign in diagnosis of rotator cuff rupture. J shoulder elbow surg. 1996;5:307–313. doi: 10.1016/s1058-2746(96)80058-9. [DOI] [PubMed] [Google Scholar]
- 12.Goutallier D, Postel JM, Bernageau J. Influence of muscular degeneration of supra and infra-spinatus on the prognosis of surgical repair of the rotator cuff. Acta Ortop Belg. 1998;64:42–5. [PubMed] [Google Scholar]
- 13.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeration in cuff ruptures. pre and post operative evaluation by CT Scan. Clinic Orthop. 1994;303:78–83. [PubMed] [Google Scholar]
- 14.Lannotti, Joseph, Williams Gerald R. 2nd edition. 2007. Disorders of the shoulder diagnosis and management; pp. 916–920. [Google Scholar]
- 15.Kristian Sen B, Christensen S. Proximal humeral fractures;late results in relation to classification and treatment. Acta orthop scand. 1987;58:124. doi: 10.3109/17453678709146455. [DOI] [PubMed] [Google Scholar]
- 16.McLaughlin H. Dislocation of the shoulder with tuberosity fracture. Surg clinics North America. 1963;43:1615. doi: 10.1016/s0039-6109(16)37150-x. [DOI] [PubMed] [Google Scholar]
- 17.Keene J, Huizenga R, Engber W, Rogers S. Proximal humeral fractures;a correlation of residual deformity with long term function. 1983;6:173. doi: 10.3928/0147-7447-19830201-07. [DOI] [PubMed] [Google Scholar]
- 18.Bono CM, Renard R, Leveine RG, Levy AS. Effect of displacement of the greater tuberosity on the mechanics of shoulder. J Bone joint surg(Br) 2001;83-B:1056–62. doi: 10.1302/0301-620x.83b7.10516. [DOI] [PubMed] [Google Scholar]
- 19.Craig E. Open reduction and internal fixation of greater tuberosity fractures, malunions and nonunions. In: craig E, editor. Master techniques in orthopaedic surgery, the shoulder. New York: Raven press, ltd; 1995. [Google Scholar]
- 20.Morris M, Kilkoyne R, Shuman W. Humeral tuberosity fractures;evaluation by CT scans and managements of malunion. Orthop trans. 1987;11:242. [Google Scholar]


