Abstract
Purpose
To correlate spectral domain optical coherence tomography (SD-OCT) and photographic imaging before and after spontaneous regression of primary vitreoretinal lymphoma (PVRL) lesions.
Procedures
We report the case of a 60-year-old female.
Results
The patient presented with bilateral creamy deposits under the retina and retinal pigment epithelium (RPE), and lesions were visible along Bruch's membrane with SD-OCT and suspicious for PVRL. Systemic workup revealed nonspecific areas of enhancement on neuroimaging. The patient was largely asymptomatic and the decision was made to observe her. Three months later, a new lesion pattern had developed. The color fundus photographs and SD-OCT demonstrated spontaneous regression of the largest sub-RPE lesion, leaving areas of RPE atrophy, while a new larger sub-RPE lesion had formed in the other eye. Vitreous biopsy showed lymphocytes and no malignant cells, while sub-RPE biopsy of the newly formed lesion revealed highly atypical cells positive for CD19 and CD20.
Conclusions
Multimodal imaging documents that PVRL lesion regression and early RPE changes can develop within a 3-month period. Immune control is an important factor in lesion regression in the eye.
Key Words: Primary vitreoretinal lymphoma, Spectral domain optical coherence tomography, Spontaneous regression, Immune surveillance
Introduction
Primary vitreoretinal lymphoma (PVRL) is a rare subset of primary central nervous system (CNS) lymphoma [1,2]. While malignancies rarely spontaneously regress, subretinal PVRL lesions have been previously reported to migrate or regress without treatment [3]. However, there is little documentation of this observation in the literature with modern imaging techniques. Here, we correlate the photographic and spectral domain optical coherence tomography (SD-OCT) findings in a case of spontaneous lesion regression in a treatment-naïve patient with PVRL.
Case Report
The patient is a 60-year old female with a past medical history significant for hypothyroidism and type 2 diabetes. Her cancer family history was positive for lymphoma and prostate cancer in her father. She had a 1-year history of intermittent scotomata and decreased vision in OU and a 3-week history of photophobia and metamorphopsia in OU resistant to topical prednisolone that she received from an outside clinic. The review of systems was otherwise unremarkable.
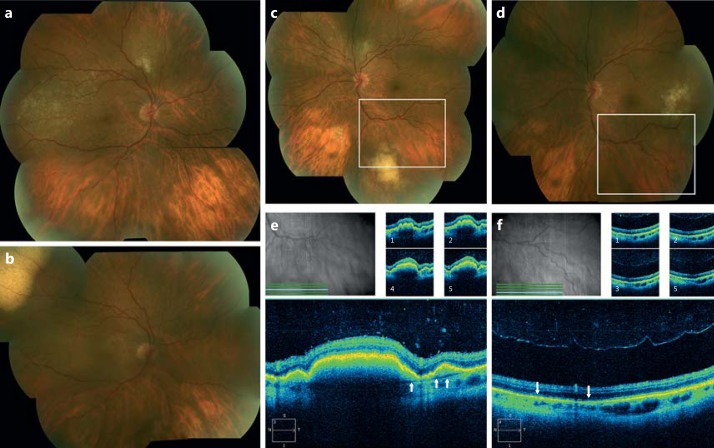
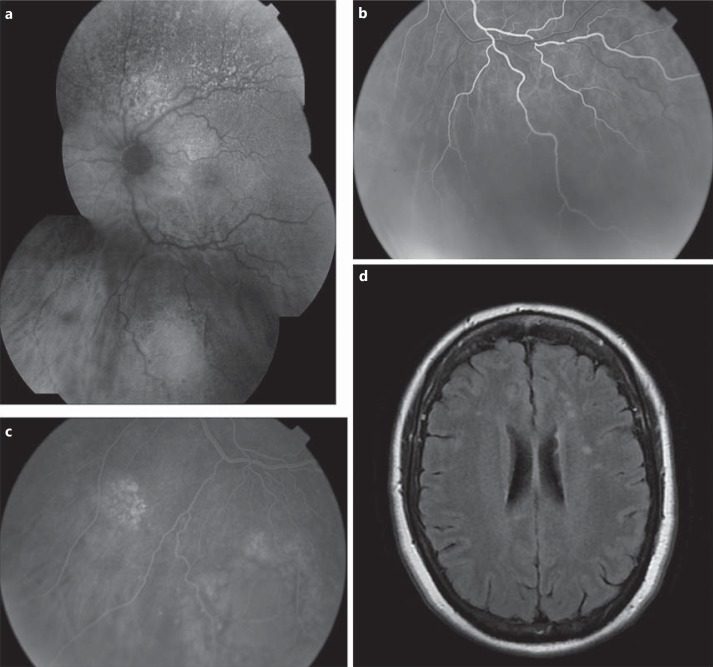
On presentation to our department, her visual acuity was 20/30 in the OD, 20/20 in the OS with quiet anterior segments and vitreous OU and multiple subretinal/subretinal pigment epithelium (RPE) creamy deposits in OU (fig. 1a, c). Fundus autofluorescence pictures showed a mixed pattern of increased and decreased autofluorescence (fig. 2a), while fluorescein angiography demonstrated early blockage in the subretinal material followed by late mild hyperfluorescence (fig. 2b, c). The SD-OCT showed accumulation of predominantly sub-RPE material along Bruch's membrane (fig. 1e).
Fig. 1.
Montage fundus photographs of the OD and OS at presentation (a, c). Note the creamy sub-RPE infiltrates in the macula, temporally, and superiorly in the OD (a) and the coalesced, fluffy sub-RPE infiltrates inferior to the inferior arcade and the discrete infiltrates superonasally in the OS (c). Three months later, many of these lesions resolved without any treatment (b OD, d OS), while a new sub-RPE lesion appeared at 10 o'clock in the OD (b) and temporal to the macula in the OS (d). SD-OCT in the area of the inferior lesion on presentation (e) showed RPE elevation secondary to prominent sub-RPE material accumulation along Bruch's membrane (arrows) and some small subretinal material accumulation, with blocked visualization of much of the choriocapillaris in the OS. Three months later, the area where the lesion regressed showed RPE atrophy and irregularity (arrows) and improved visualization of the choriocapillaris on SD-OCT (f).
Fig. 2.
a Fundus autofluorescence photograph of the OS at initial presentation showed a mixed pattern of increased and decreased autofluorescence in the areas of sub-RPE infiltrates. Laminar phase of the fluorescein angiogram at the same visit showed blockage of the choroidal circulation (b) while, in the late phase, there was mild hyperfluorescence of the subretinal lesions with fluffy appearing borders in a leopard pattern (c). d Brain MRI after the first visit was significant for some T2/flair hyperintensities in the white matter.
Brain MRI (fig. 2d) showed multiple nonspecific areas of enhancement within the brain parenchyma. These areas were suspicious for CNS lymphoma involvement given her ocular findings, but were not considered significant enough to biopsy. Chest CT was positive for nonspecific indeterminate nodules, while MRI of the orbits, CT of the abdomen and pelvis, as well as PET scan were unremarkable. Bone marrow biopsy and lumbar puncture were negative for any abnormal cell populations.
Laboratory testing was within normal limits including complete blood count, ACE, lysozyme, ANA, ESR, pANCA, cANCA, RPR, quantiferon TB-Gold, Lyme IgG/IgM, serum protein electrophoresis, and LDH. Due to excellent visual acuity and very limited disease burden, the decision was made to closely observe the patient and biopsy with any worsening. The neuro-oncologist also recommended observation until a tissue diagnosis was obtained.
At the 3-month follow-up, the patient's vision decreased to 20/50 in the OD and 20/25 in the OS. The previously documented lesions had regressed in OU, while new sub-RPE lesions appeared in other areas in OU (fig. 1b, d). SD-OCT through the largest prior lesion showed regression of the subretinal and sub-RPE material, improved visualization of the choriocapillaris, and mild atrophy of the RPE (fig. 1f).
Vitrectomy and sub-RPE biopsy of the largest lesion were performed in the OD. Cytology of the vitreous showed lymphocytes and an eosinophil. Flow cytometry and cytology of the sub-RPE biopsy were negative for CD8+ T cells or NK cells and positive for a dominant population of highly atypical B cells co-expressing CD19 and CD20, consistent with B-cell lymphoproliferative disorder. Thus, systemic treatment with rituximab and methotrexate was initiated by neuro-oncology given the mild CNS findings on MRI. The patient's lesions regressed well with systemic treatment.
Discussion
Spontaneous resolution of the primary neoplastic lesion is an unusual phenomenon in any malignancy, but this observation has been made for PVRL and other non-Hodgkin's lymphoma types [3,4]. The color fundus photographs and SD-OCT images of this report provide documentation that PVRL lesions can regress without treatment, leaving an area of RPE atrophy. The exact mechanism or clinical significance of these lesion changes is hypothesized to be due to tumor control by the host immune system, primarily by CD8+ T cells [3,4] as well as NK cells [5]. In this case, the patient's vitreous biopsy showed a predominant population of non-neoplastic lymphocytes, providing support of immune surveillance, while the sub-RPE biopsy of the newly formed lesion did not. Further elucidation of these mechanisms of immunologic tumor control and migration is valuable since it could open new therapeutic approaches against the malignant process.
Disclosure Statement
The authors have no conflicts of interest to disclose. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of these institutions.
Acknowledgments
This article was supported by the National Eye Institute of the National Institutes of Health under Award No. K08EY022672. Additional funds were provided by the Ohio Lions Eye Research Foundation, Fund #313310 in Ophthalmology, and the Patti Blow Fund.
References
- 1.Davis JL. Intraocular lymphoma: a clinical perspective. Eye. 2013;27:153–162. doi: 10.1038/eye.2012.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan CC, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, Cassoux N, Touitou V, Smith JR, Batchelor TT, Pulido JS. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16:1589–1599. doi: 10.1634/theoncologist.2011-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kase S, Namba K, Jin XH, Kubota KC, Ishida S. Spontaneous regression of intraocular lymphoma. Ophthalmology. 2012;119:1083–1084. doi: 10.1016/j.ophtha.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Iihara K, Yamaguchi K, Nishimura Y, Iwasaki T, Suzuki K, Hirabayashi Y. Spontaneous regression of malignant lymphoma of the breast. Pathol Int. 2004;54:537–542. doi: 10.1111/j.1440-1827.2004.01652.x. [DOI] [PubMed] [Google Scholar]
- 5.Ono K. Clinical significance of natural killing activity in patients with advanced lymphoma. J Clin Immunol. 1998;18:132–141. doi: 10.1023/a:1023298917191. [DOI] [PubMed] [Google Scholar]