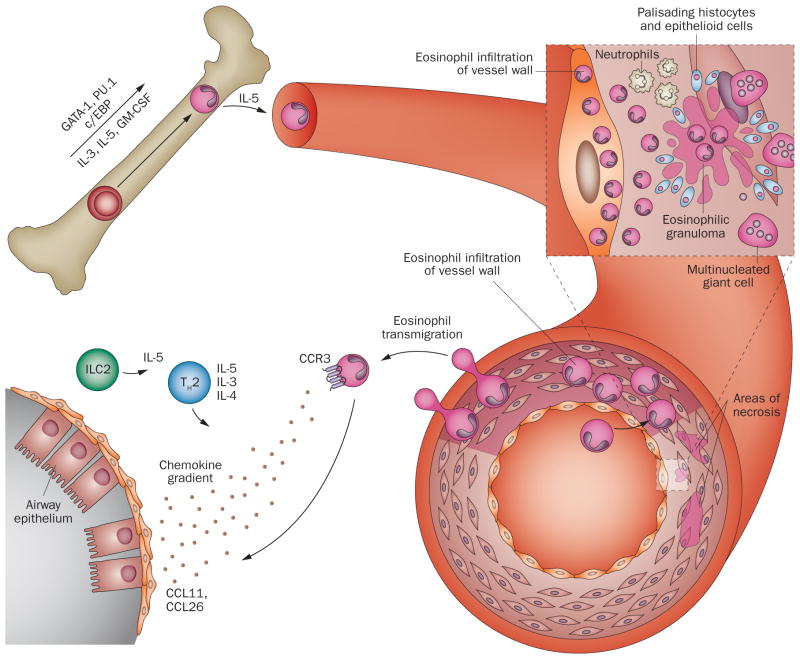
Figure 2.
Schematic representation of eosinophil trafficking. In the bone marrow, eosinophils differentiate from haematopoietic progenitor cells into mature eosinophils under the influence of transcription factors (GATA-1, PU.1, c/EBP) and their subsequent expansion is regulated by eosinophilopoietins (IL-3, IL-5, GM-CSF). Eosinophil migration into circulation is regulated primarily by IL-5. Circulating eosinophils interact with endothelial cells, migrate through the vessel wall, and infiltrate a target organ by a regulated process involving the interaction between adhesion molecules, chemokine receptors on eosinophils (CCR3) via their respective chemokine gradients (eotaxins), and cytokines (in particular products of TH2 and ILC2 cells, such as IL-4, IL-5, IL-13). The characteristic pathologic findings of eosinophil involvement in vasculitis include eosinophilic infiltration in tissue, and intravascular and extravascular granuloma formation with a zone of centralized eosinophilic necrosis and surrounding epithelioid cells, histiocytes, multinucleated giant cells, and neutrophils. Eosinophilic vasculitis of the small arteries and veins can be present, depending on the stage of disease. Abbreviations: CCL, CC-chemokine ligand; CCR, CC-chemokine receptor; c/EBP, CCAAT/enhancer-binding protein; GATA-1, GATA-binding factor 1 (also known as erythroid transcription factor); GM-CSF, granulocyte-macrophage colony-stimulating factor; ILC2, type 2 innate lymphoid cell; TH2, type 2 T helper cell.