Abstract
OBJECTIVES:
Childhood obesity is now recognized as a global public health issue. Social patterning of obesity, consistent with the theory of epidemiologic transition, has not been well described in children, and the limited research has focused on developed settings. The aim of this study was to describe the relationship between childhood obesity and household income using objective measures of adiposity and to explore how this relationship differs across levels of country human development.
METHODS:
The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) was a multi-national cross-sectional study conducted in 12 urban/suburban study sites that represented all inhabited continents and wide ranges of development. ISCOLE collected objectively measured height, body mass and percentage body fat in 7341 10-year-old children. Multi-level random-effects models were used to examine income gradients in several obesity measures.
RESULTS:
The mean age of the children was 10.4 years, and 12.6% were obese, ranging from 5.4% (Finland) to 23.8% (China). For both boys and girls, obesity prevalence, body fat percentage and body mass index (BMI) z-score increased linearly with higher income at lower levels of development (all P for trend ⩽0.0012), but decreased linearly with higher income at higher levels of development (all P for trend ⩽0.0003). Country human development explained 75% of the variation in the country-specific income–obesity relationships (r=−0.87, P=0.0003).
CONCLUSIONS:
Results are consistent with the theory of epidemiologic transition. Global efforts to control obesity must account for socioeconomic factors within a country's context. Future research should seek to understand global socioeconomic patterns in obesity-related lifestyle behaviors.
Introduction
Childhood obesity is now recognized as a global public health concern.1 Because of the recent rise in obesity rates in both developed and developing countries,2 the obesity epidemic is thought to be driven largely by environmental and social factors.1 Social patterning of obesity, consistent with the theory of epidemiologic transition,3 has been described in adults,4, 5, 6, 7 though research in children is more limited.4, 8
For children, the limited research on socioeconomic gradients in obesity has been conducted predominantly in developed (high or very high human development) countries, with a preponderance of single-country studies, and studies have used inconsistent measures of individual socioeconomic status (SES) and adiposity.4, 6, 8 These prior studies have highlighted inconsistent results across levels of development. To our knowledge, only one other published study9 has investigated the relationship between a country's economic level and socioeconomic differences in overweight based on a large, multi-national sample of children. That study, however, failed to find a relationship. In contrast to the current (International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE)) study, the prior study used self-reported measures of body mass and height and did not include countries with low or middle levels of human development.
Both low childhood SES10, 11, 12, 13 and childhood obesity14, 15 impart significant future health consequences. To address this current global epidemic and to plan for future health needs, it is essential to understand how childhood obesity relates to SES across countries of varying levels of economic and social development. Thus, the aim of this study was to describe the relationship between childhood obesity and household income using several objective measures of adiposity and to explore how this relationship might differ across a wide range of country human development.
Materials and methods
The International Study of Childhood Obesity, Lifestyle and the Environment
ISCOLE was a multi-national cross-sectional study that collected objectively measured height, body mass and percentage body fat in 7341 children across 12 urban/suburban study sites. The rational, design and methods have been published in detail.16 Each ISCOLE study site was responsible for recruiting and enrolling at least 500 children; a target sample size of 500 children per site was chosen based on a power calculation that suggested this size would provide 90% power to detect as significant predictors explaining 3% of the variability in body mass index (BMI).16 The primary sampling frame was schools, which was typically stratified by an indicator of SES in order to maximize variability within sites.16 The institutional review board at the Pennington Biomedical Research Center (coordinating center) approved the overarching ISCOLE protocol, and the institutional/ethical review boards at each participating institution also approved the local protocol. Written informed consent was obtained from parents or legal guardians, and child assent was obtained as required by the local institutional/ethical review boards.
Setting
The 12 urban/suburban sites included in ISCOLE represented countries ranging from low (0.509, Kenya) to very high (0.929, Australia) country human development (2011 Human Development Index (HDI)17). Data were collected from September 2011 through December 2013. Data collection occurred during the school year, and each site completed their data collection over a single 12-month period. Across the study, data collection proceeded in a staggered fashion, with 2–5 sites engaged in data collection at any particular time.
Participants
ISCOLE targeted 10-year-old children, and each study site determined the grade level to target that would ensure a sample with minimal variability around a mean age of 10 years. All children within the targeted grade level in a sampled school were eligible to participate; thus, the sample necessarily included children aged 9–11 years. A total of 7372 boys and girls participated in the ISCOLE study, of which 7341 remained in the analytic data set after excluding participants who did not have valid BMI (n=31).
Measurement
Anthropometry
All ISCOLE sites collected objectively measured height, body mass and percentage body fat according to a common protocol, and all study personnel were required to complete a rigorous system of training and certification that included web-based training modules and regional in-person training meetings.16 Standing height, body mass and body fat percentage were measured using standard procedures and instrumentation across all study sites. Height was measured without shoes, using a Seca 213 portable stadiometer (Seca Corporation, Hamburg, Germany), with the head in the Frankfort Plane. Body mass and body fat percentage were determined with a portable Tanita SC-240 bioelectrical impedance scale (TANITA Corporation, Tokyo, Japan), after all outer clothing, heavy pocket items and shoes were removed. Each measurement was repeated, and the average was used for analysis (a third measurement was obtained if the first two measurements were greater than 0.5 cm, 0.5 kg or 2.0% apart for height, body mass and body fat percentage, respectively, and the average of the two closest measurements was used in analyses). The BMI(kg m−2) was calculated, and BMI z-scores were computed using age- and sex-specific reference data from the World Health Organization.18 Participants were classified as obese (BMI z-score >+2 s.d.) or non-obese (BMI z-score ⩽2 +s.d.).
Household Income
Parents self-reported household income levels across eight to ten country-specific categories determined by the study site. Within each country, income was collapsed into four levels to facilitate multi-country analysis. Although not corresponding exactly to quartiles, the four levels were created to ensure the most balanced distribution possible within each country.
Country Human Development Index
The relationship between household income and adiposity was investigated across levels of human development, measured by the 2011 HDI.17 Values for the 2011 HDI corresponding to the 10th, 50th and 90th percentiles within the ISCOLE country sample were chosen to represent lower, middle and higher levels of human development. Percentiles were calculated based on weighted averages. The use of sample-based percentiles ensures that the results are not extrapolated beyond the sample HDI range, and also reduces the likelihood of results being interpreted to correspond to specific countries in the sample.
Treatment of missing data
A total of 7372 children participated in ISCOLE. BMI was missing for 31 (<1%) participants; these participants were excluded from all analyses. Body fat percentage was missing for an additional 76 (1%) participants; analysis of this outcome was conducted among participants with non-missing data.
Overall, 810 participants (11.0%) were missing data on household income. Four sites had missing income data in excess of 10%: the United Kingdom (15.3%), Brazil (22.0%), Portugal (23.3%) and South Africa (32.6%). Participants missing income data were similar to those with complete data with respect to sex, age, obesity, BMI z-score and body fat percentage.
Missing values for income were multiply imputed to reduce the chance of bias owing to exclusion of the cases with missing income data. Missing values were multiply imputed (five imputations) using fully conditional specification (FCS) methods, under missing-at-random assumptions19 and using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA; PROC MI). Country-specific models were used to impute income categories, which were subsequently collapsed into the four income levels, as described above.
Statistical analysis
Multi-level random-effects models (PROC MIXED and PROC GLIMMIX) that accounted for clustering at both the school and country levels were used to examine income gradients in the various obesity measures. Denominator degrees of freedom for statistical tests pertaining to fixed effects were calculated using the Kenward and Roger approximation.20 Interactions were used to test for differences in the income–obesity relationship across HDI levels (income-by-HDI interaction) and for differences between boys and girls (income-by-HDI-by-sex interaction). For presentation, least-square means for the obesity measures were estimated separately for boys and girls at values corresponding to the 10th, 50th and 90th percentiles for the 2011 HDI within the ISCOLE sample. Linear regression ‘slopes-as-outcome' models overall and by sex, with the country-specific SES–obesity slope (SES level as ordinal, analyses stratified by study site) as the outcome and HDI as the predictor, were used to investigate the association of HDI with the between-country differences in the SES–obesity relationships.
To properly account for the multiply imputed income data, results from all statistical analyses were averaged across the five imputed data sets, and the standard errors were adjusted using the MIANALYZE procedure in SAS. Sensitivity analyses were used to compare results from imputed data sets to those from analyses of participants with complete data, and results were similar.
Results
Descriptive characteristics of the study sample, stratified by sex and study site, are provided in Table 1. The mean age of the children was 10.4 years, and 12.6% of children were obese, which ranged from 5.4% (Finland) to 23.8% (China). ISCOLE study sites represented all inhabited continents and levels of human development (HDI) ranging from low (0.509, Kenya) to very high (0.929, Australia; Table 2).
Table 1. Descriptive characteristics of ISCOLE participants stratified by sex and study site (n=7341).
| Country (site) | n |
Age (years) |
Obesity (%) |
BMI z-score |
Body fat (%) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | |
| Australia (Adelaide) | 243 | 285 | 10.4 (0.5) | 10.3 (0.6) | 11.5 | 9.5 | 0.6 (1.1) | 0.6 (1.1) | 18.9 (6.5) | 23.9 (7.2) |
| Brazil (São Paulo) | 277 | 287 | 10.0 (0.5) | 10.0 (0.5) | 28.9 | 14.6 | 1.0 (1.5) | 0.7 (1.3) | 21.3 (9.6) | 24.7 (8.4) |
| Canada (Ottawa) | 238 | 327 | 10.1 (0.4) | 10.0 (0.4) | 14.3 | 10.1 | 0.6 (1.2) | 0.3 (1.2) | 18.7 (7.2) | 21.9 (7.3) |
| China (Tianjin) | 293 | 258 | 9.4 (0.5) | 9.4 (0.5) | 33.4 | 12.8 | 1.1 (1.6) | 0.3 (1.3) | 20.2 (8.0) | 20.7 (8.1) |
| Colombia (Bogotá) | 454 | 462 | 10.0 (0.6) | 10.0 (0.7) | 7.9 | 3.7 | 0.3 (1.1) | 0.1 (1.0) | 18.4 (5.7) | 21.6 (5.5) |
| Finland (Helsinki, Espoo and Vantaa) | 253 | 282 | 10.0 (0.5) | 10.0 (0.4) | 7.5 | 3.6 | 0.3 (1.1) | 0.2 (1.0) | 16.9 (6.2) | 20.9 (6.8) |
| India (Bangalore) | 292 | 328 | 10.0 (0.6) | 10.0 (0.6) | 12.3 | 8.5 | 0.2 (1.5) | 0.3 (1.3) | 19.5 (7.5) | 23.7 (7.0) |
| Kenya (Nairobi) | 262 | 301 | 9.7 (0.7) | 9.8 (0.7) | 7.3 | 6.0 | 0.1 (1.3) | 0.0 (1.2) | 16.1 (7.0) | 17.1 (8.5) |
| Portugal (Porto) | 358 | 419 | 10.0 (0.2) | 10.0 (0.3) | 21.5 | 14.1 | 1.0 (1.2) | 0.8 (1.1) | 20.5 (7.2) | 24.9 (7.1) |
| South Africa (Cape Town) | 222 | 327 | 9.9 (0.7) | 9.8 (0.7) | 10.4 | 11.0 | 0.2 (1.3) | 0.3 (1.3) | 17.7 (7.2) | 22.8 (7.8) |
| United Kingdom (Bath and NE Somerset) | 237 | 287 | 10.4 (0.5) | 10.4 (0.5) | 10.1 | 9.4 | 0.5 (1.1) | 0.4 (1.2) | 18.2 (6.4) | 23.3 (6.7) |
| United States (Baton Rouge) | 281 | 368 | 9.6 (0.7) | 9.5 (0.6) | 19.6 | 18.2 | 0.9 (1.4) | 0.8 (1.3) | 20.9 (8.5) | 24.9 (7.9) |
Abbreviations: BMI, body mass index; ISCOLE, International Study of Childhood Obesity, Lifestyle and the Environment.
Table 2. ISCOLE country socioeconomic indicators and country-specific sample income levels.
| Country (site) | 2011 Human Development Index |
ISCOLE sample income levels: Within-country (%)a
and Country currency range |
|||
|---|---|---|---|---|---|
| L1 (ISO code)b | L2 | L3 | L4 | ||
| Australia | 0.929 | 23.9% | 30.2% | 24.5% | 21.4% |
| ⩽$49 999 (AUD) | $50 000–89 999 | $90 000–139 999 | ⩾$140 000 | ||
| Brazil | 0.718 | 38.4 | 24.4 | 21.5 | 15.7 |
| ⩽R$19 620 (BRL) | R$19 621–32 700 | R$32 701–58 860 | >R$58 860 | ||
| Canada | 0.908 | 19.7 | 28.1 | 14.3 | 37.9 |
| ⩽$59 999 (CAN) | $60 000–109 999 | $110 000–139 999 | >$140 000 | ||
| China | 0.687 | 19.8 | 19.5 | 28.5 | 32.2 |
| <¥20 000 (CNY) | ¥20 000–39 999 | ¥40 000–79 999 | >¥80 000 | ||
| Colombia | 0.710 | 35.0 | 24.8 | 17.7 | 22.6 |
| ⩽$8 400 000 (COP) | $8 400 001–12 000 000 | $12 000 001–18 000 000 | >$18 000 000 | ||
| Finland | 0.882 | 20.7 | 19.8 | 19.5 | 40.1 |
| ⩽€39 999 (EUR) | €40 000–59 999 | €60 000–79 999 | >€80 000 | ||
| India | 0.547 | 23.5 | 19.9 | 18.7 | 38.0 |
| ⩽Rs239 999 (INR) | Rs240 000–479 999 | Rs480 000–719 999 | >Rs720 000 | ||
| Kenya | 0.509 | 23.2 | 25.1 | 22.6 | 29.1 |
| ⩽Ksh121 991 (KES) | Ksh121 992–466 727 | Ksh466 728–1 199 999 | >Ksh1 200 000 | ||
| Portugal | 0.809 | 20.8 | 30.8 | 27.7 | 20.6 |
| <€6000 (EUR) | €6000–11 999 | €12 000–23 999 | >€24 000 | ||
| South Africa | 0.619 | 50.4 | 21.4 | 16.1 | 12.1 |
| <R11 500 (ZAR) | R11 500–30 000 | R30 001–300 000 | >R300 000 | ||
| United Kingdom | 0.863 | 27.0 | 28.7 | 23.3 | 21.0 |
| ⩽£19 999 (GBP) | £20 000–39 999 | £40 000–59 999 | >£60 000 | ||
| United States | 0.910 | 20.3 | 31.1 | 27.2 | 21.4 |
| <$10 000 (USD) | $10 000–49 999 | $50 000–139 999 | >$140 000 | ||
Abbreviations: ISCOLE, International Study of Childhood Obesity, Lifestyle and the Environment; ISO, International Organization for Standardization.
Across imputed data sets (m=5).
ISO 4217 standard currency codes.
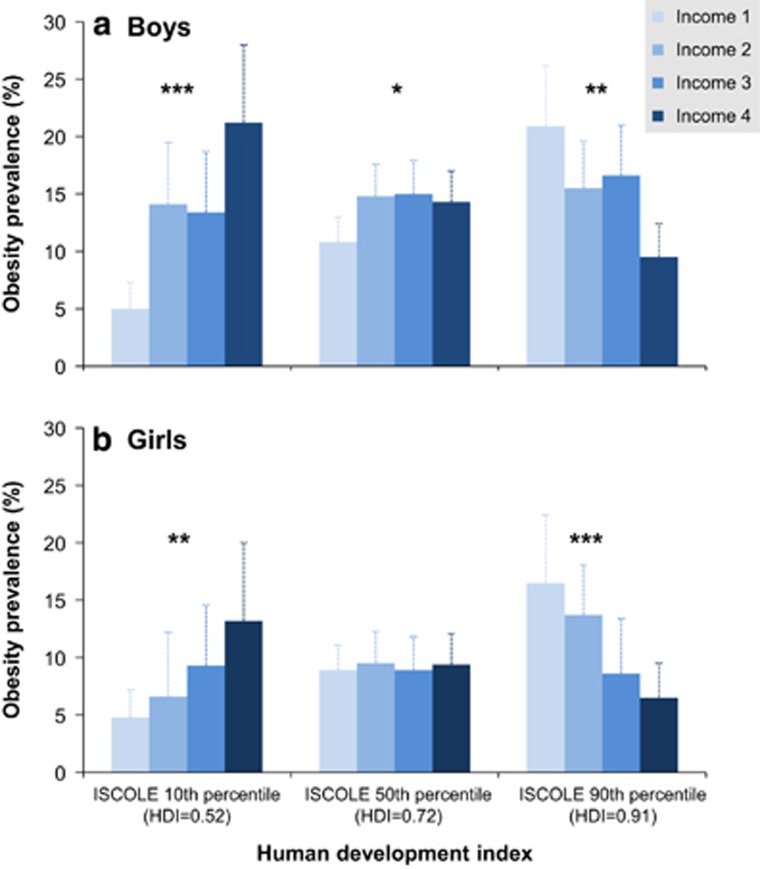
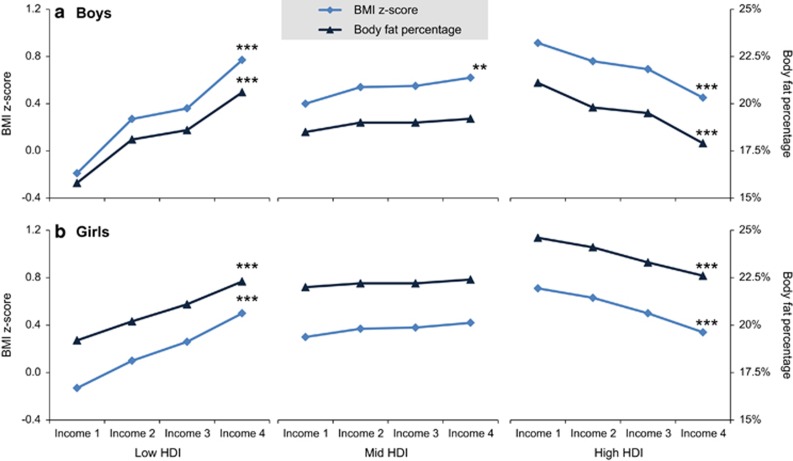
For both boys and girls, obesity was positively associated with income at lower levels of HDI and negatively associated with income at higher levels of HDI (Table 3 and Figure 1). There was a significant interaction between obesity prevalence and HDI in both boys (P=0.0351) and girls (P=0.0041), but no indication of different relationships between the two groups. Furthermore, this pattern—that the income gradient in obesity reverses itself as one moves from low-to-high levels of development—was consistent across all measures of adiposity (Figure 1 and Figure 2). For all adiposity measures, there was a significant interaction with HDI (boys: BMI z-score (P=0.0002), body fat (P=0.0009); girls: BMI z-score (P=0.0013), body fat (P=0.0071)); however, there was no indication of different income gradients for boys and girls. Finally, across successively higher levels of country human development, obesity levels decline in the highest income group, whereas they increase in the lowest income group.
Table 3. Least-square mean estimates for measures of adipositya across income levels, by sex and human development index.
| Level 1 | Level 2 | Level 3 | Level 4 | P for trendb | |
|---|---|---|---|---|---|
| Boys | |||||
| ISCOLE 10th percentile of HDI | |||||
| Obesity prevalence | 5.0 (2.3) | 14.1 (5.4) | 13.4 (5.3) | 21.2 (6.8) | <0.001 |
| BMI z-score | −0.19 (0.20) | 0.27 (0.21) | 0.36 (0.21) | 0.77 (0.20) | <0.001 |
| Body fat (%) | 15.8 (1.1) | 18.1 (1.1) | 18.6 (1.1) | 20.6 (1.1) | <0.001 |
| ISCOLE 50th percentile of HDI | |||||
| Obesity prevalence | 10.8 (2.2) | 14.8 (2.8) | 15.0 (2.9) | 14.3 (2.7) | 0.05 |
| BMI z-score | 0.40 (0.11) | 0.54 (0.11) | 0.55 (0.11) | 0.62 (0.11) | 0.003 |
| Body fat (%) | 18.5 (0.6) | 19.0 (0.6) | 19.0 (0.6) | 19.2 (0.6) | 0.15 |
| ISCOLE 90th percentile of HDI | |||||
| Obesity prevalence | 20.9 (5.3) | 15.5 (4.1) | 16.6 (4.4) | 9.5 (2.9) | <0.001 |
| BMI z-score | 0.96 (0.16) | 0.80 (0.15) | 0.73 (0.15) | 0.48 (0.15) | <0.001 |
| Body fat (%) | 21.1 (0.8) | 19.8 (0.8) | 19.5 (0.8) | 17.9 (0.8) | <0.001 |
| Girls | |||||
| ISCOLE 10th percentile of HDI | |||||
| Obesity prevalence | 4.8 (2.0) | 6.5 (2.6) | 8.9 (3.4) | 13.0 (4.3) | 0.001 |
| BMI z-score | −0.13 (0.16) | 0.10 (0.16) | 0.26 (0.16) | 0.50 (0.15) | <0.001 |
| Body fat (%) | 19.2 (1.3) | 20.2 (1.2) | 21.1 (1.3) | 22.3 (1.2) | <0.001 |
| ISCOLE 50th percentile of HDI | |||||
| Obesity prevalence | 8.8 (1.6) | 9.2 (1.7) | 8.6 (1.6) | 8.9 (1.7) | 0.95 |
| BMI z-score | 0.30 (0.08) | 0.37 (0.08) | 0.38 (0.08) | 0.42 (0.08) | 0.07 |
| Body fat (%) | 22.0 (0.6) | 22.2 (0.6) | 22.2 (0.7) | 22.4 (0.7) | 0.29 |
| ISCOLE 90th percentile of HDI | |||||
| Obesity prevalence | 15.2 (3.5) | 12.7 (3.0) | 8.3 (2.3) | 6.1 (1.8) | <0.001 |
| BMI z-score | 0.71 (0.12) | 0.63 (0.11) | 0.50 (0.12) | 0.34 (0.12) | <0.001 |
| Body fat (%) | 24.6 (0.9) | 24.1 (0.9) | 23.3 (0.9) | 22.6 (0.9) | <0.001 |
Abbreviations: BMI, body mass index; HDI, Human Development Index.
Least-square mean estimates of adiposity measures at HDI levels corresponding to the 10th, 50th and 90th percentiles of the ISCOLE country sample (HDI=0.52, 0.72 and 0.91, respectively).
Test for linear trend (linear contrast) across the four income levels.
Figure 1.
Income gradients in obesity prevalence across HDI levels in boys (a) and girls (b). Data are shown as least-square means at HDI levels corresponding to the 10th, 50th and 90th percentiles of the ISCOLE sample (HDI=0.52, 0.72 and 0.91, respectively). Tests for linear trend are indicated: *P<0.05, **P<0.001; ***P<0.0001.
Figure 2.
Income gradients in adiposity measures across HDI levels in boys (a) and girls (b). Data are shown as least-square means at HDI levels corresponding to the 10th, 50th and 90th percentiles of the ISCOLE sample (HDI=0.52, 0.72 and 0.91, respectively). Tests for linear trend are indicated: **P<0.001; ***P<0.0001.
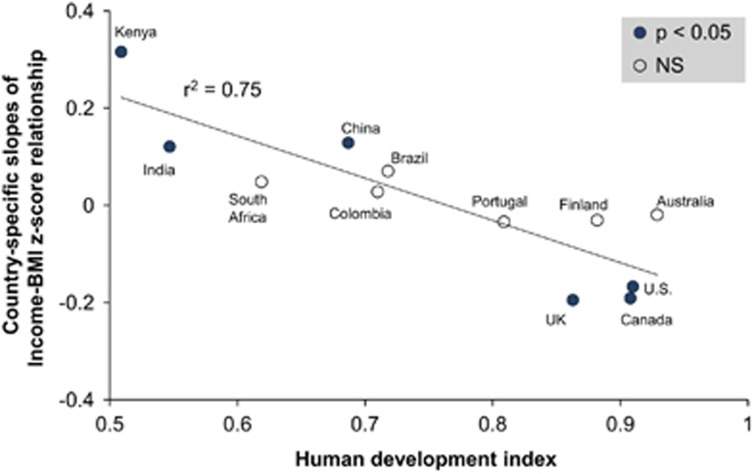
Our analysis reveals a very strong negative relationship between HDI and the country-specific income–obesity gradients (Figure 3). Across countries, HDI explained 75% of the variation in the country-specific income–obesity relationships (r=−0.87, P=0.0003). The relationships were similar in boys and girls (P for interaction=0.56). The income–obesity gradient is estimated to be zero for countries near a 2011 HDI of 0.76, with positive income gradients in obesity at lower levels of development and negative income gradients at higher levels. In stratified analysis, BMI z-score was significantly associated with income in six of the twelve ISCOLE countries.
Figure 3.
Relationship between country-specific income–obesity gradients and HDI.
Discussion
This is the first study of childhood obesity that included children from countries of low to very high levels of human development, that collected objective anthropometric measures and that collected these measures according to a common protocol. Results demonstrated a strong relationship between childhood obesity and income, which is modified by the level of a country's development. For both boys and girls, obesity prevalence, body fat percentage and BMI z-score were positively associated with income at lower levels of human development and negatively associated with income at higher levels of development.
For children, the limited research on socioeconomic gradients in obesity has been conducted predominantly in developed (high or very high HDI) countries, with a preponderance of single-country studies, and studies have used inconsistent measures of individual SES and adiposity, precluding meta-analyses.4, 6, 8 These prior studies have highlighted inconsistent results across levels of development. Results from the current study show that for countries with moderate levels of human development in which the income gradient would be plateauing before reversing, income gradients are generally non-significant. This observation could help to explain the inconsistent results from prior studies while also placing them within a clear pattern of income–obesity gradients across levels of country development.
To our knowledge, only one other published study9 has investigated the relationship between a country's economic level and levels of socioeconomic differences in overweight based on a large, multi-national sample of children. That study, however, failed to find a relationship. In contrast to the current (ISCOLE) study, the prior study used self-reported measures of body mass and height, and represented countries with more limited variability in human development (2011 HDI from 0.729 to 0.943). If the current analysis had been restricted to sites with comparable levels of human development, we would also have failed to identify the strong relationship between human development and income gradients in obesity, reinforcing the importance of including less-developed countries in this research.
Our results are consistent with the theory of epidemiologic transition, which characterizes changes across levels of a country's development in patterns of morbidity and mortality from infectious causes to chronic and ‘man-made' diseases.3 With respect to obesity, the epidemiologic transition encompasses both dietary changes (shifts from undernutrition and malnutrition to overnutrition, and from traditional diets to more energy-dense ‘western' diets) and changes in physical activity (shifts away from high levels of occupation- and transportation-based physical activity to more sedentary lifestyles) often referred to as the ‘nutrition transition'21 and the ‘physical activity' transition.22
The epidemiologic transition predicts a social patterning of obesity in countries in transition, such that groups with higher income, standards of living and levels of nutrition shift first, resulting in higher levels of obesity compared with the lower-income groups.3 Furthermore, in these settings, obesity may be valued as an indicator of relative affluence, reinforcing the prevalence of obesity in the higher-income groups. As a country's development increases, food scarcity, famine and malnutrition become less common, such that the lower-income groups experience less malnutrition, increasing their relative adiposity. The lack of a consistent relationship between income and obesity in mid-HDI countries may be related to increased access to low-cost, energy-dense foods coupled with the necessity of physically intense labor among the low-income groups resulting in an increased obesity prevalence approaching that of high-income populations in these countries. Then, as countries complete the transition to a more Western ‘modern' lifestyle and standards of living increase, overfeeding and being less active become economically possible. At high HDI, the income–obesity gradient shifts with the lower-income groups experiencing higher levels of obesity, potentially related to lower costs of energy-dense foods23 and decreased access to safe places to be physically active.24, 25
The incidence of major cardiovascular events is currently highest in low-income countries, despite lower levels of obesity.26 At present, policies in most low- and mid-HDI countries favor prevention of undernutrition, and only some countries have implemented policies to prevent obesity.27 Consequently, as childhood obesity levels increase globally, lower-income countries will be more impacted by cardiovascular disease and associated medical and social costs. Also, as global development increases, poorer segments of the population are projected to see the highest increases in obesity, further compounding the global burden of cardiovascular disease.
A particular strength of the current research is the wide variability in levels of human development present in the country sample and the analysis of objective obesity data collected under a rigorous, common protocol; as such, the ISCOLE sample provides clearer insights into how social determinants of health28, 29 may be impacting childhood obesity globally. The ISCOLE sample was limited to children in urban and suburban settings, so results may not generalize to rural settings; however, this aspect of the study design also prevents confounding by the extent of urbanization on the estimated relationships. Recent research in adults suggests that urban–rural differences in obesity seen in less-developed countries may be mainly attributable to SES,30 so our results may be relevant for rural settings as well.
In conclusion, childhood obesity prevalence is related to household income, though the strength and direction of this relationship differs according a country's level of human development. Consequently, as childhood obesity levels continue to rise, it will be important to account for socioeconomic factors within a country's context in the global effort to control the epidemic. This effort should include a better understanding of socioeconomic gradients in specific behaviors that contribute to obesity, namely diet, physical activity and sedentary behavior. Finally, as global development increases, poorer segments of the population are projected to see the highest increases in obesity.
Acknowledgments
We thank the ISCOLE External Advisory Board and the ISCOLE participants and their families who made this study possible. A membership list of the ISCOLE Research Group and External Advisory Board is included in Katzmarzyk et al. (this issue). ISCOLE was funded by The Coca-Cola Company. MF has received a research grant from Fazer Finland. RK has received a research grant from Abbott Nutrition Research and Development.
MF has received an honorarium for speaking for Merck. AK has been a member of the Advisory Boards of Dupont and McCain Foods. VM is a member of the Scientific Advisory Board of Actigraph and has received an honorarium for speaking for The Coca-Cola Company. TO has received an honorarium for speaking for The Coca-Cola Company. The remaining authors declare no conflict of interest.
References
- World Health Organization. Consultation on Obesity. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: i–xii, 1–253. [PubMed] [Google Scholar]
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q 1971; 49: 509–538. [PubMed] [Google Scholar]
- Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull 1989; 105: 260–275. [DOI] [PubMed] [Google Scholar]
- Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ 2004; 82: 940–946. [PMC free article] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiol Rev 2007; 29: 29–48. [DOI] [PubMed] [Google Scholar]
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev 2012; 13: 1067–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990-2005. Obesity 2008; 16: 275–284. [DOI] [PubMed] [Google Scholar]
- Due P, Damsgaard MT, Rasmussen M, Holstein BE, Wardle J, Merlo J et al. Socioeconomic position, macroeconomic environment and overweight among adolescents in 35 countries. Int J Obes 2009; 33: 1084–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEniry M. Early-life conditions and older adult health in low- and middle-income countries: a review. J Dev Orig Health Dis 2013; 4: 10–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: a review. Obes Rev 2012; 13: 347–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael D. Poverty in childhood and adverse health outcomes in adulthood. Maturitas 2011; 69: 22–26. [DOI] [PubMed] [Google Scholar]
- Tamayo T, Christian H, Rathmann W. Impact of early psychosocial factors (childhood socioeconomic factors and adversities) on future risk of type 2 diabetes, metabolic disturbances and obesity: a systematic review. BMC Public Health 2010; 10: 525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidding SS, Bao W, Srinivasan SR, Berenson GS. Effects of secular trends in obesity on coronary risk factors in children: the Bogalusa Heart Study. J Pediatr 1995; 127: 868–874. [DOI] [PubMed] [Google Scholar]
- Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 2005; 111: 1999–2012. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M et al. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health 2013; 13: 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Development Programme. Human Development Report 2011. Available at http://www.undp.org/content/dam/undp/library/corporate/HDR/2011%20Global%20HDR/English/HDR_2011_EN_Complete.pdf (accessed on 4 August 2014).
- de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. J Wiley & Sons: New York, NY, USA, 1987. [Google Scholar]
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 1997; 53: 983–997. [PubMed] [Google Scholar]
- Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev 1997; 55: 31–43. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Mason C. The physical activity transition. J Phys Act Health 2009; 6: 269–280. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Specter S. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition 2004; 79: 6–16. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 2006; 117: 417–424. [DOI] [PubMed] [Google Scholar]
- Loukaitou-Sideris A, Eck JE. Crime prevention and active living. Am J Health Promot 2007; 21: 380–389 iii. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 2014; 371: 818–827. [DOI] [PubMed] [Google Scholar]
- Rivera JA, de Cossio TG, Pedraza LS, Aburto TC, Sanchez TG, Martorell R. Childhood and adolescent overweight and obesity in Latin America: a systematic review. Lancet Diabetes Endocrinol 2014; 2: 321–332. [DOI] [PubMed] [Google Scholar]
- Marmot M. Social determinants of health inequalities. The Lancet 2005; 365: 1099–1104. [DOI] [PubMed] [Google Scholar]
- World Health Organization, Commission on Social Determinants of Health. A conceptual framework for action on the social determinants of health 2007. Available at http://www.who.int/social_determinants/resources/csdh_framework_action_05_07.pdf (accessed on 2 July 2008).
- Neuman M, Kawachi I, Gortmaker S, Subramanian SV. Urban-rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am J Clin Nutr 2013; 97: 428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]