Abstract
Context
It has been proposed that altered dynamic-control strategies during functional activity such as jump landings may partially explain recurrent instability in individuals with functional ankle instability (FAI).
Objective
To capture jump-landing time to stabilization (TTS) and ankle motion using a multisegment foot model among FAI, coper, and healthy control individuals.
Design
Cross-sectional study.
Setting
Laboratory.
Patients or Other Participants
Participants were 23 individuals with a history of at least 1 ankle sprain and at least 2 episodes of giving way in the past year (FAI), 23 individuals with a history of a single ankle sprain and no subsequent episodes of instability (copers), and 23 individuals with no history of ankle sprain or instability in their lifetime (controls). Participants were matched for age, height, and weight (age = 23.3 ± 3.8 years, height = 1.71 ± 0.09 m, weight = 69.0 ± 13.7 kg).
Intervention(s)
Ten single-legged drop jumps were recorded using a 12-camera Vicon MX motion-capture system and a strain-gauge force plate.
Main Outcome Measures
Mediolateral (ML) and anteroposterior (AP) TTS in seconds, as well as forefoot and hindfoot sagittal- and frontal-plane angles at jump-landing initial contact and at the point of maximum vertical ground reaction force were calculated.
Results
For the forefoot and hindfoot in the sagittal plane, group differences were present at initial contact (forefoot: P = .043, hindfoot: P = .004). At the hindfoot, individuals with FAI displayed more dorsiflexion than the control and coper groups. Time to stabilization differed among groups (AP TTS: P < .001; ML TTS: P = .040). Anteroposterior TTS was longer in the coper group than in the FAI or control groups, and ML TTS was longer in the FAI group than in the control group.
Conclusions
During jump landings, copers showed differences in sagittal-plane control, including less plantar flexion at initial contact and increased AP sway during stabilization, which may contribute to increased dynamic stability.
Key Words: chronic ankle instability, ankle sprains, ankle-sprain copers
One of the most common injuries experienced by individuals involved in physical activity is a lateral ankle sprain.1–3 After an acute ankle sprain, 32%–47% of patients report functional ankle instability (FAI),4–6 a clinical diagnosis characterized by symptoms of giving way, instability, or resprains (or a combination of these).7 Functional ankle instability can limit physical activity and activities of daily living for years postinjury4,6 and is associated with significant health risks such as posttraumatic osteoarthritis.8
Although the mechanisms for this condition are not clearly understood, several pathologic factors have been associated with FAI,9 including altered joint kinematics during motion10–14 and altered kinetics upon ground contact.10,15–18 Both kinematics and kinetics can demonstrate the strategies by which an individual attempts to maintain dynamic joint stability during functional activity.15,19 Landing from a jump is 1 common task in physical activity that requires dynamic stabilization and is also a common mechanism of ankle-inversion injury.20 As such, the mechanics of jump landing have received considerable attention in the ankle-instability literature.11,13,15,16,18,21–23
Specifically, a number of authors10,13,16,18,22,23 have hypothesized that kinematic differences exist during jump landings between individuals with FAI and healthy controls. However, findings have been inconsistent and methods varied. At initial contact (IC), Caulfield and Garrett13 reported ankle sagittal-plane group differences, whereas others10,14,16 failed to find such differences. Fewer researchers have investigated frontal-plane differences; again only 1 group reported increased ankle inversion in individuals with FAI, and this was before (not at) IC.10 Methodologic changes may clarify the currently mixed literature. First, the use of a more reliable and precise biomechanical model to capture foot and ankle motion may enhance our ability to detect group differences. In the FAI literature, reporting of the kinematic model used is deficient, including marker placement, mathematical modeling assumptions, and perhaps most importantly, the repeatability of the model. Especially because the angular differences reported in studies between FAI and healthy participants tend to be small (2°–7° in the frontal plane),10,11,13 the interpretation of results is difficult without adequate information about the repeatability and precision of the biomechanical modeling. If an accurate and precise model is not used, errors may either obscure true group differences or create spurious differences.
Furthermore, most investigators10–14,16,18,23 of jump landings used a 1-segment foot model. This model assumes that the foot is a single rigid segment, despite the numerous articulations within the foot and ankle complex. Thus, although it can provide a picture of the overall motion of the foot and ankle, by definition, a single-segment foot model cannot capture the differences in hindfoot and forefoot motion that can be reliably captured with a multisegment model such as the Oxford foot model.24–26 Because hindfoot, forefoot, and hallux motion are not identical during activity,24 a model able to capture these movements may be essential in accurately representing motion in individuals with FAI. Simpler models may have obscured differences by pooling hindfoot and forefoot motion into a single composite value.
In addition to kinematic differences, kinetics may also elucidate dynamic-control strategies. Studies of forces at ground contact have included relatively simple measures, such as peak force and time to peak force,14,17 as well as more complex measures such as time to stabilization (TTS).16,21,27–29 The TTS calculates the time (in seconds) it takes postlanding for an individual's ground reaction forces (GRF) in either the mediolateral (ML) or anteroposterior (AP) direction to stabilize to the level of normal quiet stance. An ability to stabilize quickly is generally seen as a positive or protective trait. Multiple investigators15,16,29 have found TTS deficiencies in individuals with FAI. Increased TTS in the AP direction is most common,15,16,29 but increased ML TTS has also been reported.15 Additionally, other authors30–32 have used a unique but similar measure of GRF stability, the dynamic postural-stability index and its directional components (MLSI and APSI). Differences in the dynamic postural stability index30–32 and APSI30,31 have been reported most often, whereas MLSI has not differed among controls and FAI participants. Therefore, despite the evidence of deficits in individuals with FAI, the exact nature of those deficits and why they have not been found consistently are not clear.
One methodologic change that may help to clarify the current literature for both ankle kinematics and TTS is the addition of a comparison group frequently referred to as copers. Copers are individuals who have experienced a lateral ankle sprain but have not developed instability.33,34 Studying the characteristics of copers compared with individuals with FAI may help further elucidate the mechanism of instability, because copers' lack of instability may be due to an ability to dynamically stabilize the foot and ankle during activity despite past ankle injury.
To our knowledge, only Brown et al14 have compared ankle-joint kinematics during jump landings between copers and individuals with FAI (ie, noncopers). They found no difference in ankle-joint motion at IC between their FAI and coper groups during a drop jump. However, they did not include a healthy control group, so whether the values they reported for copers and individuals with FAI were within or outside of a healthy normal range is unknown. In a subsequent report, Brown et al35 did include all comparison groups but did not report angles; rather, they focused on movement variability. It is interesting that they found individuals with ankle instability had restricted movement variability at the hip and knee compared with controls.35 In the TTS literature, only Steib et al21,28 have included a coper group. In 1 report, they observed that copers had slightly faster AP TTS than controls.28 However, in another report using similar methods, Steib et al21 noted no group differences among FAI, coper, and control participants. They did not address the reason(s) for their apparently conflicting findings. Therefore, it is still unclear whether true TTS differences exist among FAI, coper, and control participants.
In summary, perhaps due in part to limitations in biomechanical modeling and participant comparisons, how individuals with FAI cope or fail to cope with the condition and dynamically stabilize their ankles during jump landings remains unknown. Therefore, the purpose of our study was to attempt to clarify the literature by capturing TTS and kinematic data using a reliable foot and ankle model during jump landings among 3 groups of participants (FAI, copers, and controls).
We hypothesized that individuals with FAI would be more plantar flexed at IC and more inverted immediately post-IC at the point of maximal vertical GRFs (vGRFmax) than copers and controls. It has been shown36 that both increased inversion and increased plantar flexion can contribute to the creation of a potentially damaging inversion moment at the ankle. Regarding TTS, we hypothesized that individuals with FAI would have longer AP and ML TTS than copers or controls. Because both copers and controls are dynamically stable, we did not expect to find TTS or kinematic differences between these groups.
METHODS
Participants
We studied 23 participants with FAI, 23 participants with a history of an ankle sprain but no instability (copers), and 23 participants with no history of ankle sprain or instability (controls). Each group contained 12 men and 11 women. Participant demographics are reported in Table 1. This research was part of a larger investigation of coping mechanisms and movement patterns among individuals with and without instability, and additional participant characteristics can be found in previous reports.37,38 Based on our pilot data for the primary variables in this report, we needed a minimum of 16 participants per group to detect differences with 80% power. However, we chose to recruit a greater number per group to be more consistent with the current literature.10,13,14 Before data collection began, this study was approved by the university's institutional review board. All participants were recruited from a large metropolitan area, including a university campus.
Table 1. .
Participant Demographics
| Descriptor |
Functional Ankle Instability |
Coper |
Control |
| Age, y | 23.30 ± 3.84 | 23.52 ± 3.68 | 23.17 ± 4.01 |
| Height, m | 1.71 ± 0.11 | 1.72 ± 0.07 | 1.72 ± 0.08 |
| Weight, kg | 68.66 ± 14.60 | 69.57 ± 13.94 | 68.78 ± 13.26 |
| Cumberland Ankle Instability Tool score (maximum score = 30) | 20.52 ± 2.94a | 27.74 ± 1.69 | 28.78 ± 1.78 |
| Limited weight bearing, d | 11.74 ± 14.06 | 5.86 ± 6.58 | NA |
| Initial ankle sprain evaluated by a medical professional? | 19 yes | 16 yes | NA |
| 4 no | 7 no | ||
| Severity of initial ankle sprain | 2 mild | 3 mild | NA |
| 6 moderate | 4 moderate | ||
| 4 severe | 2 severe | ||
| 11 unknown | 14 unknown |
Abbreviation: NA, not applicable.
Functional ankle instability group scored lower than the coper and control groups.
Functional ankle instability and coper participants were required to have a history of a unilateral inversion ankle sprain that required protected weight bearing, immobilization, or limited activity (or all 3) for ≥24 hours. Also, FAI participants had to report multiple episodes of giving way (at least 2 in the past year)14 and be classified as having FAI using a cutoff score of ≤27 on the Cumberland Ankle Instability Tool (CAIT).39 Although this investigation was conducted before the recently published International Ankle Consortium position statement40 on selection criteria, our inclusion and exclusion criteria were largely in agreement with the recommendations of this group despite a few minor variances. Specifically, the number of months or years since initial injury was not formally tracked as part of the current investigation (although anecdotal data indicate a period of multiple years); the CAIT cutoff was higher because we used the value originally validated by Hiller et al39; our minimum number of episodes of giving way was slightly lower (although 91% of participants met the stricter International Ankle Consortium recommendation of 2 in the past 6 months); and lastly, we excluded anyone with acute symptoms on the day of testing, but we cannot say with certainty that each participant's most recent acute injury was >3 months before testing. Copers had no complaints of ankle instability or repeated episodes of giving way and had resumed all preinjury activities without limitation for at least 12 months before testing.14,41 The CAIT was used to assess stability. Similar to previous research,30,42 if all other inclusion criteria were met, copers were allowed a single episode of giving way in their lifetime as long as it occurred at least 12 months before study participation. Our coper inclusion criteria align with the recent recommendations of Wikstrom and Brown,34 with a minor variance as to the initial severity of injury. Control participants had no history of ankle sprain or instability in their lifetime. Additionally, all participants were required to be involved in ≥1.5 hours of moderate to vigorous physical activity per week.14,41 Participants self-reported their weekly activity level and intensity using simple recall. Potential participants were excluded if they had a history of surgery or ankle fracture in either lower extremity, any acute symptoms of lower extremity injury on the day of testing, or a known systemic disease or condition affecting the musculoskeletal system.43
Participants reported for a single visit to the Sports Medicine Research Laboratory. After providing informed consent, the participant completed an injury-history questionnaire and the CAIT to verify inclusion criteria. The injury-history form collected information about the initial ankle-sprain injury, symptoms of giving way and resprains, history of lower extremity fractures or surgeries, and limb dominance. A customized computer program (Access, Microsoft Corporation, Redmond, WA) recorded and scored participant responses for the CAIT. The CAIT has excellent test-retest reliability (intraclass correlation coefficient [2,1] = 0.96) and is scored from 0–30 points, with higher scores indicating better stability.39 We measured participant height using a Seca mechanical column scale (Hanover, MD). To record weight, the participant stood quietly on a force plate (Bertec Corporation, Columbus, OH), and we calculated the vertical component of the GRF.
We matched copers and healthy controls to FAI participants by sex, age (±10 years), height (±10 cm), and weight (±15 kg). Additionally, each group had equal numbers of left-dominant and right-dominant individuals (2 left, 21 right). Limb dominance was assessed by asking the individual to self-report his or her dominant or preferred limb for activities such as kicking a soccer ball. Testing was performed on the involved limb (side of the ankle sprain) of the FAI and coper groups and the matched side of the healthy control group. For FAI individuals with bilateral instability, the participant was asked to subjectively identify the most unstable ankle, and that side was designated as the involved limb.
Motion-Capture Preparation
The examiner attached 5 rigid plastic plates of markers to the participant using tape prewrap and attached 34 individual 9.5-mm reflective markers using double-sided adhesive tape at specific anatomical landmarks. Marker placement was according to the Oxford foot model with additional conventional gait model markers on the knee, hip, and pelvis.25,26 Marker plates were attached to the posterior pelvis at the height of the posterior-superior iliac spine and bilaterally on the distal thigh and shank. Anatomical markers were placed bilaterally on the greater trochanters, anterior-superior iliac spines, lateral and medial femoral epicondyles, lateral and medial malleoli, proximal and distal fifth metatarsals, distal second metatarsal, proximal and distal first metatarsals, and lateral, medial, posterior-superior, and posterior-inferior calcaneus.
The participant stood in the capture volume in anatomical position as a static calibration trial was captured. We then removed the calibration-only markers (ie, bilateral greater trochanter, lateral and medial femoral epicondyles, medial malleolus, and posterior-superior calcaneus). For all movement trials, a 12-camera motion-monitoring system (model Vicon MX; Oxford Metrics Group, Oxford, UK) collected the 3-dimensional location of reflective markers at 100 Hz, and 2 strain-gauge force plates (model 4060-NC; Bertec Corporation) captured GRF at 1000 Hz. Vicon Nexus 1.4 software (Oxford Metrics Group) synchronized all data collection.
Single-Legged Drop Jump
A single-legged drop jump was performed by having the participant step off a 40-cm box using the uninvolved leg and land on the force plate on the involved leg (Figure 1).13 Upon landing, the participant balanced on the involved leg for at least 10 seconds. The examiner described and demonstrated the single-legged drop-jump task, and then the participant performed a minimum of 3 practice trials to feel comfortable with the task. Ten successful jump landings were recorded, with trials separated by approximately 30 seconds of rest. An unsuccessful trial was any trial in which the participant did not maintain balance for the full 10 seconds, hopped or shifted the involved foot on the force plate, stepped down with the opposite limb, or landed with the involved foot not completely on the force plate. The number of unsuccessful trials was recorded for each participant. After completing 10 successful trials, participants were asked to rate how stable their ankle felt while completing the task on a scale of 0–10, with 0 indicating very unstable and 10 indicating very stable. The purpose of this rating was to assess each individual's perceived stability during the single-legged drop-jump task.
Key Points
Ankle-sprain copers differed from those with functional ankle instability (FAI) in anterior-posterior and medial-lateral time-to-stabilization characteristics.
Both ankle-sprain copers and participants with FAI demonstrated increased dorsiflexion during a jump landing, but the location of the motion (forefoot versus hindfoot, respectively) was different.
Clinicians may want to target motor-program flexibility and normal joint range of motion in rehabilitation protocols for those with FAI.
Figure 1. .
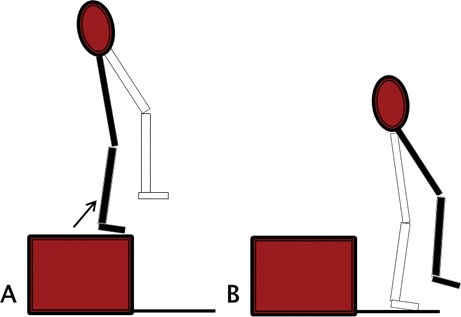
Single-legged drop-jump task. A, Starting position. B, Ending position. Solid black leg represents the uninvolved side; white leg represents the involved side.
Data Processing
Kinematics
All kinematic data were processed using Visual3D Professional (version 4.00.19; C-Motion Inc, Germantown, MD). Kinematic data for the forefoot and hindfoot were calculated using the segment coordinate systems defined by Stebbins et al.25 Euler angles were calculated for the hindfoot relative to the tibia (hindfoot angle) and forefoot relative to the hindfoot (forefoot angle) using the Grood and Suntay sequence.44 Dynamic hindfoot and forefoot angles were calculated for the involved limb referenced to standing neutral position (setting all angles equal to 0 in standing neutral position), and all kinematic data were filtered at 12 Hz using a zero-lag, fourth-order digital Butterworth filter.45 These methods are highly reliable for calculating adult forefoot and hindfoot motion (intraclass correlation coefficient = 0.83–0.97).26
We identified 2 events: the onset of vertical GRF greater than 10 N (IC)14 and vGRFmax. Initial contact has been investigated in various studies.10,13,14,16,22 Although vGRFmax has not been used frequently to compare kinematic data, the large forces seen at this moment could be associated with injury or instability, and other authors14,17 have recognized the potential importance of this time point by comparing peak GRF or time to peak GRF. Forefoot and hindfoot positions in the sagittal and frontal planes were recorded at IC and vGRFmax of each jump landing. Data at each event were averaged across 10 trials for each participant.46 For 2 participants (1 coper, 1 FAI), data-collection errors resulted in fewer than 10 useable trials. Rather than exclude these participants and unbalance participant matching, we used the average of each participant's 7 available trials for analysis.
Additionally, jump height was calculated and averaged across trials. Jump height was defined as the difference between pelvic height at jump initiation and pelvic height at maximal point of the jump trajectory. Because the task was a drop jump, we did not expect large jump heights.
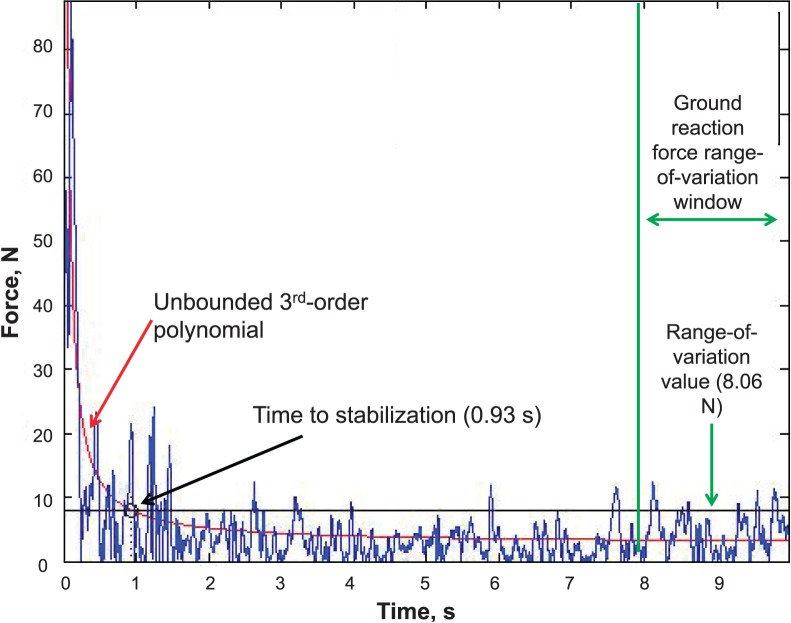
Time to Stabilization
A custom-written MATLAB software program (version R2013b; MathWorks, Natick, MA) calculated TTS using the methods of Ross et al15 with 1 minor adaptation: our trial length was shorter, and thus, we used a GRF range-of-variation window of the last 2 seconds of each trial (seconds 8–10) instead of the originally reported last 5 seconds (seconds 15–20). In brief, we calculated a normalized reference variable using only control-participant trials by taking the smallest absolute GRF ranges during the last 2 seconds of each trial for both the AP and ML components and dividing these components by participant body weight to normalize. We then averaged across all trials for a single participant and across all control participants to identify an overall mean range of variation for the AP and ML components. Three standard deviations of the overall mean were added to the overall mean to create a normalized range-of-variation variable. The resulting range-of-variation variables were 0.0180 and 0.0123 in the AP and ML lateral directions, respectively. For each participant and trial, in both AP and ML directions, an unbounded third-order polynomial was fit to the rectified force data during the 10 seconds postlanding. The range-of-variation value for each participant was calculated using the normalized range-of-variation variable multiplied by participant body weight in Newtons, and TTS was defined as the time point when the unbounded third-order polynomial first crossed the range-of-variation value (Figure 2). Time to stabilization was then averaged across trials for each participant and across participants within each group. Due to data-collection errors, useable TTS data were not available for 7 participants (1 FAI, 4 copers, 2 controls). Therefore, we did not include these 7 participants in the analysis of TTS.
Figure 2. .
Example of calculation of mediolateral time to stabilization of 1 trial of 1 participant.
Statistical Analysis
For our kinematic data, we tested differences among groups at each time point (IC and vGRFmax) among 4 dependent variables: hindfoot sagittal-plane position, hindfoot frontal-plane position, forefoot sagittal-plane position, and forefoot frontal-plane position. Therefore, for each dependent variable, we conducted a test for group differences separately at each time point within a mixed-model analysis of variance (ANOVA) with model effects for group (FAI, coper, control), time (IC, vGRFmax), and the group-by-time interaction. These tests compared model effects to address our specific research questions regarding the effect of group at IC and the effect of group at vGRFmax. We chose to conduct these tests within a mixed-model ANOVA (as opposed to independent 1-way ANOVAs) to account for correlations among data at each time point and within groups, thereby increasing statistical power and decreasing error due to multiple comparisons. At each time point, if the test for group was significant (α ≤ .05), we investigated group differences using mean differences and the Hedges g effect size with 95% confidence intervals (CIs). Effect sizes were interpreted as 0.2 = small, 0.5 = medium, and 0.8 = large. For TTS, separate 1-way ANOVAs tested group differences in the ML and AP directions (α ≤ .05). If they were significant, we calculated 3 pairwise comparisons to investigate group differences; mean differences and Hedges g effect sizes with 95% CIs are also reported.
In addition to the primary analyses, group differences in the CAIT, jump height, failed jump trials, and perceived instability were investigated using 1-way ANOVAs. For all 1-way ANOVAs, α was set at .05, and the Tukey post hoc test was performed for significant differences. All analyses were completed using SPSS (version 20; IBM Corporation, Armonk, NY).
RESULTS
Participant Demographics
Participant demographics are reported in Table 1. Individuals with FAI self-reported 5.81 ± 8.42 episodes of giving way in a typical month. The groups differed on the CAIT (P < .001). Tukey post hoc testing revealed that the FAI group scored lower than the coper and control groups (FAI versus coper: mean difference = −7.22, standard error [SE] = 0.65, 95% CI = −8.78, −5.66; FAI versus control: mean difference = −8.26, SE = 0.65, 95% CI = −9.82, −6.70). Lower CAIT scores indicate increased perceived instability. However, the coper and control groups were not different from each other (control versus coper: mean difference = 1.04, SE = 0.65, 95% CI = −0.52, 2.61).
Single-Legged Drop Jump
Descriptive data for jump-landing kinematics are shown by group in Table 2.
Table 2. .
Kinematics During Single-Legged Drop-Jump Task
| Kinematics |
Group |
F2,66 Value |
P Value |
||||||||
| Functional Ankle Instability |
Coper |
Control |
|||||||||
| Mean |
Standard Error |
95% Confidence Interval |
Mean |
Standard Error |
95% Confidence Interval |
Mean |
Standard Error |
95% Confidence Interval |
|||
| Initial contact | |||||||||||
| Forefoot | |||||||||||
| Sagittal planea | –10.32 | 0.82 | –11.96, −8.68 | –7.94 | 0.82 | –9.58, −6.30 | –10.69 | 0.82 | –12.33, −9.04 | 3.31 | .043c |
| Frontal planeb | –4.58 | 0.52 | –5.62, −3.53 | –5.41 | 0.52 | –6.46, −4.36 | –5.79 | 0.52 | –6.84, −4.74 | 1.40 | .245 |
| Hindfoot | |||||||||||
| Sagittal planea | –10.08d,e | 0.77 | –11.62, −8.54 | –13.26e | 0.77 | –14.80, −11.72 | –13.51d | 0.77 | –15.05, −11.96 | 4.01 | .004c |
| Frontal planeb | 7.81 | 1.08 | 5.66, 9.96 | 6.67 | 1.08 | 4.52, 8.81 | 8.54 | 1.08 | 6.40, 10.69 | 0.77 | .466 |
| Maximum vertical ground reaction forces | |||||||||||
| Forefoot | |||||||||||
| Sagittal planea | 7.07 | 0.62 | 5.83, 8.31 | 6.47 | 0.62 | 5.23, 7.71 | 5.93 | 0.62 | 4.69, 7.17 | 0.84 | .435 |
| Frontal planeb | –2.95 | 0.55 | –4.04, −1.86 | –3.72 | 0.55 | –4.82 −2.63 | –4.38 | 0.55 | –5.47, −3.29 | 1.72 | .188 |
| Hindfoot | |||||||||||
| Sagittal planea | 4.88 | 0.84 | 3.21, 6.56 | 5.22 | 0.84 | 3.55, 6.90 | 4.92 | 0.84 | 3.25, 6.60 | 0.05 | .952 |
| Frontal planeb | –8.42 | 0.74 | –9.90, −6.95 | –8.74 | 0.74 | –10.22, −7.26 | –7.70 | 0.74 | –9.17, −6.22 | 0.52 | .596 |
Positive angle indicates dorsiflexion; negative angle indicates plantar flexion.
Positive angle indicates inversion; negative angle indicates eversion.
Difference among groups.
Difference between control and functional ankle-instability groups.
Difference between coper and functional ankle-instability groups.
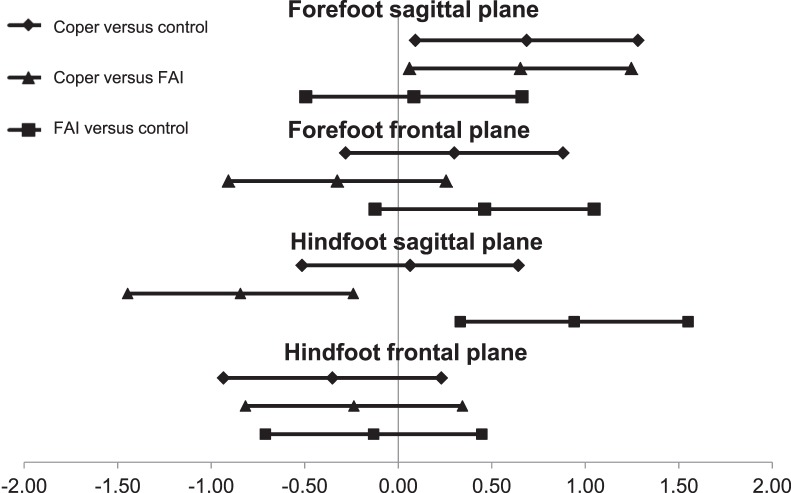
Dorsiflexion and Plantar Flexion
For the forefoot in the sagittal plane (ie, dorsiflexion-plantar flexion), the groups were different at IC (P = .043). A trend toward increased dorsiflexion in the coper group compared with the FAI and control groups was evident, with medium effect sizes (Figure 3; control versus coper mean difference = −2.75°; coper versus FAI mean difference = 2.39°). The control and FAI groups did not differ, as shown by the small effect size (control versus FAI mean difference = −0.36°). Forefoot sagittal-plane motion at vGRFmax was not different (P = .435; Figure 4).
Figure 3. .
Hedges g effect sizes and 95% confidence intervals for kinematic results at initial contact. Confidence intervals not crossing the zero point represent statistically significant effects at P < .05. Abbreviation: FAI, functional ankle instability.
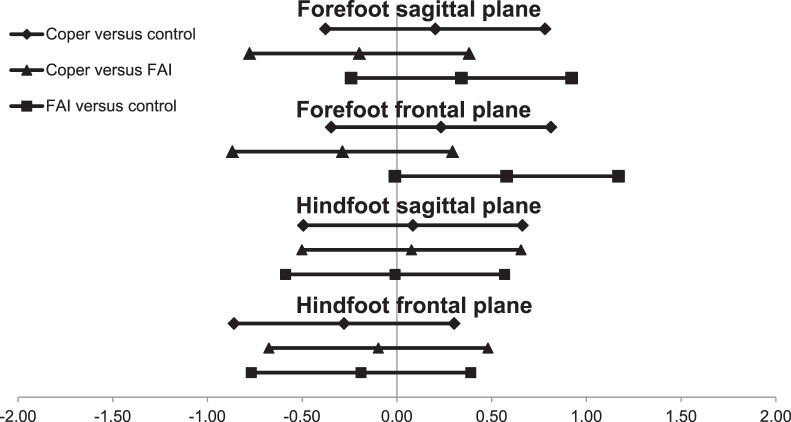
Figure 4. .
Hedges g effect sizes and 95% confidence intervals for kinematic results at vertical ground reaction force maximum. Confidence intervals not crossing the zero point represent statistically significant effects at P < .05. Abbreviation: FAI, functional ankle instability.
For the hindfoot in the sagittal plane, a group difference was observed at IC (P = .004). Specifically, individuals with FAI were more dorsiflexed than the coper or control groups, with strong effect sizes (Figure 3; control versus FAI mean difference = −3.43°; coper versus FAI mean difference = −3.18°). The coper and control groups were not different from each other, as shown by the small effect size (mean difference = −0.25°). We identified no group differences in hindfoot sagittal-plane motion at vGRFmax (P = .952; Figure 4).
Inversion and Eversion
For both the hindfoot and forefoot in the frontal plane (ie, inversion-eversion), no group differences were apparent at IC or vGRFmax (hindfoot IC: P = .466; hindfoot vGRFmax: P = .596; forefoot IC: P = .245; forefoot vGRFmax: P = .188; Table 2; Figures 3 and 4).
Time to Stabilization
The TTS was different among groups (AP TTS: P < .001; ML TTS: P = .040). Post hoc tests indicated that AP TTS was longer in the coper group than in the FAI and control groups (Figures 5 and 6; coper versus control mean difference = 0.54; coper versus FAI mean difference = 0.67 seconds); however, the control and FAI groups were not different from each other (mean difference = 0.13 seconds). Mediolateral TTS was longer in the FAI group than in controls; however, copers were not different from either the FAI or control group (Figures 5 and 6; coper versus control mean difference = −0.26; coper versus FAI mean difference = −0.15; FAI versus control mean difference = −0.42).
Figure 5. .
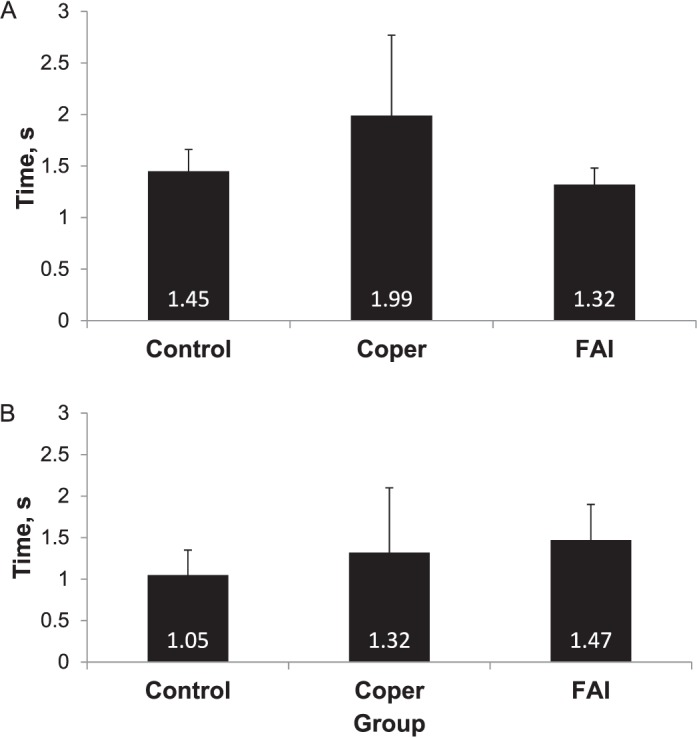
Time to stabilization results in the A, Anteroposterior, and B, Mediolateral directions. Abbreviation: FAI, functional ankle instability.
Figure 6. .
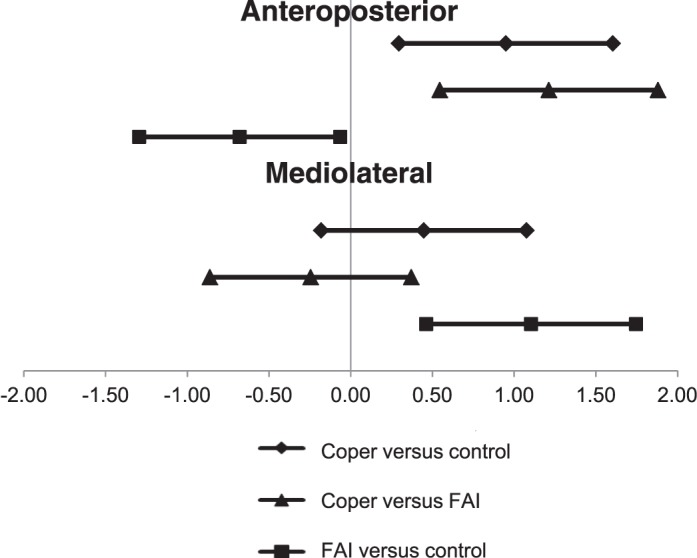
Hedges g effect sizes and 95% confidence intervals for time to stabilization in the anteroposterior and mediolateral directions. Confidence intervals not crossing the zero point represent statistically significant effects at P < .05. Abbreviation: FAI, functional ankle instability.
Jump Height and Perceived Stability
Jump height did not differ between groups (P = .354; FAI: 0.025 ± 0.031 m; coper: 0.013 ± 0.027 m, control: 0.015 ± 0.028 m), indicating that, regardless of group, participants jumped to similar heights. The small magnitude of the average jump demonstrates that participants correctly performed the drop jump. No difference was evident in the number of unsuccessful jump-landing trials between groups for (P = .407; FAI: 1.87 ± 1.42; coper: 1.83 ± 1.72; control: 1.30 ± 1.58). However, perceived instability during the jump-landing task differed between groups (P < .001; FAI: 5.77 ± 1.80; coper: 8.32 ± 1.67; control: 8.35 ± 1.30). Tukey post hoc testing revealed that individuals with FAI perceived greater instability than copers or controls (FAI versus control: mean difference = 2.58, SE = 0.48, 95% CI = 1.43, 3.72; FAI versus coper: mean difference = 2.55, SE = 0.48, 95% CI = 1.39, 3.70). Copers and controls were not different from each other (mean difference = 0.03, SE = 0.48, 95% CI = −1.12, 1.17).
DISCUSSION
We hypothesized that individuals with FAI would have greater plantar flexion at IC and greater inversion at vGRFmax. Although we did find group differences in sagittal-plane motion at IC, in general, the direction of this motion was contrary to our expectations, and no group differences were seen in hindfoot or forefoot inversion. We additionally hypothesized that individuals with FAI would have longer TTS in both the AP and ML directions, and these hypotheses were partially supported. Individuals with FAI had longer ML TTS than controls; however, copers had longer AP TTS than those in the FAI and control groups.
Dorsiflexion and Plantar Flexion
Several groups examined jump-landing kinematics between individuals with FAI and controls10,13,16,18,22,23 and between individuals with FAI and copers.14 To our knowledge, we are the first to include all 3 groups in a single study. We found group differences at IC for both forefoot and hindfoot sagittal-plane motion (dorsiflexion-plantar flexion). Specifically, the FAI group had more hindfoot dorsiflexion than either the coper or control groups. Our results agree with the findings of Caulfield and Garrett,13 who reported increased dorsiflexion in their FAI group compared with controls. They hypothesized that increased dorsiflexion in individuals with FAI may be a protective adaptation that creates a more stable position for the lateral ankle ligaments and the talocrural joint. If increased dorsiflexion is a positive adaptation to increase stability postankle sprain, one might assume that the coper group should also demonstrate this pattern. However, our coper group did not demonstrate increased dorsiflexion. This indicates that increased dorsiflexion is not an adaptation common to all individuals with a history of ankle sprain, but rather, it is specific to individuals who experience instability. Copers in our study maintained dynamic stability without adopting a more dorsiflexed movement pattern.
Contrary to the hypothesis of Caulfield and Garrett,13 we might argue that the increased dorsiflexion noted in individuals with FAI is not a positive adaptation but is perhaps a less stable movement pattern that actually contributes to FAI. One potential explanation for how increased dorsiflexion at IC could contribute to instability is by decreasing the time over which the joint can absorb impact forces. Landing with greater plantar flexion at IC allows a greater range of motion (ROM) for force attenuation. If increased dorsiflexion is indeed a less stable movement pattern, it may have preceded the development of FAI and served as a contributing mechanism. However, given the retrospective nature of our study design, we cannot establish the temporal relationship between instability and increased dorsiflexion.
Although our finding of increased hindfoot dorsiflexion agrees with the work of Caulfield and Garrett,13 several other groups found no difference in ankle dorsiflexion at IC of jump landing between individuals with FAI and controls10,16,22 or between individuals with FAI and copers.14 Although the studies showing no difference had low power, their average sample size (22.5 ± 2.7 per group) was almost identical to ours (n = 23 per group). Thus, it does not appear that an insufficient number of participants was the sole cause for the different results. It could be that slight differences in methods or participant inclusion criteria account for the conflicting results between studies, with the most obvious difference being the use of a single- or multisegment foot model.
We also detected a group difference for forefoot sagittal-plane motion (dorsiflexion-plantar flexion) at IC. Investigating this difference, we found medium effect sizes for the difference between copers and our 2 other groups, indicating that copers had slightly less forefoot plantar flexion at IC than FAI or control participants. Although dorsiflexion and plantar flexion of the hindfoot (primarily at the talocrural joint) may be generally better understood, forefoot motion (primarily at the tarsal-metatarsal joint) can also contribute to overall foot posturing in a more plantar-flexed or dorsiflexed position. If we visualize a ballerina en pointe, we realize that her extreme foot position is not achieved through hindfoot motion alone but rather through the combined motions of the forefoot and the hindfoot. Thinking about forefoot motion in terms of dorsiflexion and plantar flexion may seem novel, yet the only novel aspect is separating its measurement from hindfoot motion. Mean differences between the FAI and coper group (2.39°) and the coper and control group (2.75°) are worth further research. The meaning of this trend is not clear, but given the coper group's self-reported lack of instability, the relatively more dorsiflexed forefoot posturing found in this study may be a positive adaptation. If this is the case, relatively greater amounts of forefoot dorsiflexion and hindfoot dorsiflexion at IC may have opposing effects on stability. Further study is needed before we draw any conclusions as to the clinical relevance of this finding.
Inversion and Eversion
We did not find frontal-plane (ie, inversion-eversion) group differences at IC or vGRFmax for either the hindfoot or forefoot segments. This lack of differences at IC is consistent with other reports using a drop jump-landing task,10,14 although 1 group did find increased inversion in the interval before IC.10 Delahunt et al22 were the only authors to report increased ankle inversion in individuals with FAI specifically at IC; however, rather than a jump-landing task, they used a lateral hop. Differences in the nature of a lateral-hopping task may account for the increased inversion at IC, whereas others10,14 and we found no group differences. To our knowledge, we are the first group to use vGRFmax as a specific time point for kinematic analysis because the large forces seen at this moment could be associated with injury or instability if combined with joint malpositioning. Although there were no group differences at this time point, which occurs rapidly after IC, our kinematic results demonstrate large changes in foot positioning between IC and vGRFmax. One limitation of this study is that the timing of vGRFmax post IC was not recorded; thus, we cannot speculate whether joint kinematics at this time point would be primarily influenced by feedforward or feedback motor-control strategies.
Time to Stabilization
As expected, individuals with FAI took longer to stabilize in the ML direction than did healthy individuals. Our findings are similar to several previous reports15,16,27; however, others21,28,29 have reported no difference. Task and calculation differences may account for the apparently conflicting findings, as demonstrated in the work of Wikstrom et al47 and Liu et al.48 Specifically, Steib et al21,28 used a diagonal-jump task rather than the standard forward jump. Also, all 3 groups that found no ML differences used a calculation originally developed by Ross and Guskiewicz,49 which was later modified15 because the original formula used each participant's static single-legged GRF range-of-variation value as its own reference variable to calculate AP and ML TTS. Thus, a participant with poorer static single-legged balance would have a larger reference variable, which would result in the appearance of a shorter TTS. Because individuals with FAI have been shown to demonstrate static postural-control deficits,50 this could lead to a systematic underestimation of their TTS. This problem and 1 solution are discussed in detail by Ross et al,15 and we recommend that all future researchers use the modified methods.
Perhaps more interesting than the increased ML TTS we report is the addition of a coper group for comparison. As shown in Figure 5B, the coper group was not different than either the FAI or control groups. This finding makes it difficult to interpret whether the deficits found in the FAI group are meaningful, given that copers who report no instability have a ML TTS that is similar to that of FAI participants. Future authors should investigate whether training that improves TTS, such as that reported by Ross and Guskiewicz,27 also increases patient-reported stability or whether there is no correlation between TTS improvements and changes in perceived instability.
It is interesting that copers demonstrated a longer AP TTS than either FAI or control individuals. Copers' increased time in AP sway may be a compensatory technique, allowing greater freedom in the AP plane while quickly controlling ML sway to limit the potential of ML forces to create a destabilizing inversion moment. Future researchers should investigate the responses of copers and individuals with FAI to expected and unexpected perturbations to see if indeed copers use control strategies that allow greater AP sway while controlling ML sway. To our knowledge, only Steib et al21,28 have included a coper group when making TTS comparisons. They found a slightly shorter AP TTS in copers compared with controls in 1 study28 and a slightly longer AP TTS in copers and FAI compared with controls in another study.21 Unfortunately, they did not discuss these apparently conflicting findings, perhaps because the primary aim of both studies was to investigate fatigue-related changes rather than prefatigue group differences. Although the method of standardizing jump height was minimally different in the 2 studies, all other methods appear identical and do not lead to an easy explanation. It should be noted that they used a slightly different outcome measure, but Wikstrom et al30 also compared the dynamic stability of the 3 groups of interest in this study: FAI, copers, and controls. They reported the MLSI and APSI, which capture a similar (but not identical) concept as TTS.51 They found a higher APSI in copers and FAI compared with controls and higher MLSI in copers than in controls and FAI, with no other pairwise comparisons reaching significance. Because of differences in the measure, no direct comparisons can be made. However, their results reinforce our finding that copers may use different postural-control mechanisms than individuals with FAI.
We found no difference between FAI and control participants in AP TTS, yet multiple other authors16,27,29 have reported longer AP TTS in FAI participants than in controls. We believe a slight difference in the jump-landing task may explain these differences. Our study used a forward drop jump, whereas most previous investigators have used a forward jump to 50% of maximal vertical-jump height, starting 70 cm from the force plate.15,16,29 Thus, previous research had a much larger AP motion component than our drop jump. Both the current and previous jump-landing tasks may capture unique control strategies individuals use when they encounter the demands of jump landings under various conditions.
Perceived Stability
Additionally, we tracked participants' perceived stability during task completion, with the primary purposes of assessing whether our task sufficiently challenged dynamic stability in our participants and identifying which group of individuals would feel most challenged by the same task. Previous investigators41,52 used a simple binary question (eg, “Did you feel unstable while completing this task?”) to assess perceived stability during task completion. However, we felt that perceived stability most likely exists in a continuum. Thus, we asked our participants to report stability on a scale of 0 (very unstable) to 10 (very stable). Our FAI group reported feeling less stable (mean = 5.8) than both copers and controls (mean = 8.3 and 8.4, respectively). This provides evidence that the task itself was sufficient to challenge stability, especially in FAI participants.
Clinical Application
Because copers displayed more AP TTS variability than individuals with FAI, clinicians aiming to decrease ankle instability should include rehabilitation and injury-prevention exercises that target flexible motor patterns, potentially by incorporating both expected and unexpected perturbations during functional tasks. Additionally, as FAI and coper individuals tend to differ in the amount and location (forefoot versus hindfoot) of dorsiflexion, interventions that restore normal ROM within the entire foot and ankle complex may also be beneficial, as well as functional training that encourages use of the full ROM. Finally, as alterations in kinematics and TTS seem to manifest in the sagittal plane (rather than the frontal plane, as has long been hypothesized), clinicians should place renewed focus on dorsiflexion and plantar-flexion motions.
Limitations
Our participants completed the jump-landing task barefoot because the multiple anatomical markers attached to each foot prevented them from wearing normal athletic shoes. Several participants (from all groups) complained that the jump landing was uncomfortable because of the lack of cushioning a shoe would normally provide. No participant was unable to complete the task due to this discomfort. However, it might have modified landing strategy compared with a shod landing. Despite this limitation, we believe our group comparisons are valid because participants in all groups were tested under the same barefoot condition.
Additionally, we chose to use a drop jump from a 40-cm box based on previous research on jump-landing kinematics in the FAI population.10 Yet during the testing, we noticed that using a single box height can create unequal task difficulty for a very short versus a very tall individual. Because our participants were matched for height, we do not think this limitation affected our group comparisons. However, we recommend that future researchers normalize box height to a percentage of participant height to create a more equal task among participants.
Lastly, data-collection errors limited the total number of participants included in our TTS analysis. However, even after excluding participants without useable data, our groups still numbered 22, 19, and 21 for FAI, copers, and controls, respectively. These final sample sizes are comparable with the previous literature.15,16,29
CONCLUSIONS
Individuals with FAI, ankle-sprain copers, and healthy controls display differences in both joint kinematics and kinetics. Group differences were found in hindfoot and forefoot dorsiflexion, ML TTS, and AP TTS. The exact mechanism by which copers maintain dynamic stability is still not clear, but the current research shows that, during drop-jump landings, copers displayed differences in sagittal-plane control: less plantar flexion at IC and increased AP sway during stabilization. Future authors should continue to investigate how sagittal-plane alterations may increase or decrease dynamic stability, using a similar 3-group model.
REFERENCES
- 1.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine—trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22–27. doi: 10.1249/01.mss.0000241637.52231.18. [DOI] [PubMed] [Google Scholar]
- 3.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 4.Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 5.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braun BL. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8(2):143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- 7.Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 8.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 9.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 10.Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res. 2006;24(10):1991–2000. doi: 10.1002/jor.20235. [DOI] [PubMed] [Google Scholar]
- 11.Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970–1976. doi: 10.1177/0363546506290989. [DOI] [PubMed] [Google Scholar]
- 12.Monaghan K, Delahunt E, Caulfield B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin Biomech (Bristol, Avon) 2006;21(2):168–174. doi: 10.1016/j.clinbiomech.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Caulfield BM, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23(1):64–68. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 14.Brown C, Padua D, Marshall SW, Guskiewicz K. Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech (Bristol, Avon) 2008;23(6):822–831. doi: 10.1016/j.clinbiomech.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 15.Ross SE, Guskiewicz KM, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 16.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–355. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caulfield B, Garrett M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin Biomech (Bristol, Avon) 2004;19(6):617–621. doi: 10.1016/j.clinbiomech.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 18.de Noronha M, Refshauge KM, Crosbie J, Kilbreath SL. Relationship between functional ankle instability and postural control. J Orthop Sports Phys Ther. 2008;38(12):782–789. doi: 10.2519/jospt.2008.2766. [DOI] [PubMed] [Google Scholar]
- 19.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 20.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steib S, Hentschke C, Welsch G, Pfeifer K, Zech A. Effects of fatiguing treadmill running on sensorimotor control in athletes with and without functional ankle instability. Clin Biomech (Bristol, Avon) 2013;28(7):790–795. doi: 10.1016/j.clinbiomech.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17(6):641–648. doi: 10.1111/j.1600-0838.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 23.Gribble P, Robinson R. Differences in spatiotemporal landing variables during a dynamic stability task in subjects with CAI. Scand J Med Sci Sports. 2010;20(1):e63–e71. doi: 10.1111/j.1600-0838.2009.00899.x. [DOI] [PubMed] [Google Scholar]
- 24.Carson MC, Harrington ME, Thompson N, O'Connor JJ, Theologis TN. Kinematic analysis of a multi-segment foot model for research and clinical applications: a repeatability analysis. J Biomech. 2001;34(10):1299–1307. doi: 10.1016/s0021-9290(01)00101-4. [DOI] [PubMed] [Google Scholar]
- 25.Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T. Repeatability of a model for measuring multi-segment foot kinematics in children. Gait Posture. 2006;23(4):401–410. doi: 10.1016/j.gaitpost.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Wright CJ, Arnold BA, Coffey TG, Pidcoe PE. Repeatability of the modified oxford foot model during gait in healthy adults. Gait Posture. 2011;33(1):108–112. doi: 10.1016/j.gaitpost.2010.10.084. [DOI] [PubMed] [Google Scholar]
- 27.Ross SE, Guskiewicz KM. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16(4):323–328. doi: 10.1097/00042752-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Steib S, Zech A, Hentschke C, Pfeifer K. Fatigue-induced alterations of static and dynamic postural control in athletes with a history of ankle sprain. J Athl Train. 2013;48(2):203–208. doi: 10.4085/1062-6050-48.1.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown C, Ross SE, Mynarks R, Guskiewicz KM. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 2004;13(2):122–134. [Google Scholar]
- 30.Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Dynamic postural control but not mechanical stability differs among those with and without chronic ankle instability. Scand J Med Sci Sports. 2010;20(1):e137–e144. doi: 10.1111/j.1600-0838.2009.00929.x. [DOI] [PubMed] [Google Scholar]
- 31.Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Borsa PA. Dynamic postural stability deficits in subjects with self-reported ankle instability. Med Sci Sports Exerc. 2007;39(3):397–402. doi: 10.1249/mss.0b013e31802d3460. [DOI] [PubMed] [Google Scholar]
- 32.Brown CN, Bowser B, Orellana A. Dynamic postural stability in females with chronic ankle instability. Med Sci Sports Exerc. 2010;42(12):2258–2263. doi: 10.1249/MSS.0b013e3181e40108. [DOI] [PubMed] [Google Scholar]
- 33.Hertel J, Kaminski TW. Second international ankle symposium summary statement. J Orthop Sports Phys Ther. 2005;35(5):A2–A6. [PubMed] [Google Scholar]
- 34.Wikstrom EA, Brown CN. Minimum reporting standards for copers in chronic ankle instability research. Sports Med. 2014;44(2):251–268. doi: 10.1007/s40279-013-0111-4. [DOI] [PubMed] [Google Scholar]
- 35.Brown C, Bowser B, Simpson KJ. Movement variability during single leg jump landings in individuals with and without chronic ankle instability. Clin Biomech (Bristol, Avon) 2012;27(1):52–63. doi: 10.1016/j.clinbiomech.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 36.Konradsen L, Voigt M. Inversion injury biomechanics in functional ankle instability: a cadaver study of simulated gait. Scand J Med Sci Sports. 2002;12(6):329–336. doi: 10.1034/j.1600-0838.2002.00108.x. [DOI] [PubMed] [Google Scholar]
- 37.Wright CJ, Arnold BL, Ross SE, Ketchum JM, Ericksen JJ, Pidcoe PE. Clinical examination results in individuals with functional ankle instability and ankle-sprain copers. J Athl Train. 2013;48(5):581–589. doi: 10.4085/1062-6050-48.3.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wright CJ, Arnold BL, Ross SE, Pidcoe PE. Individuals with functional ankle instability, but not copers, have increased forefoot inversion during walking gait. Athl Train Sport Health. 2013;5(5):201–209. [Google Scholar]
- 39.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 40.Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014;49(1):121–127. doi: 10.4085/1062-6050-49.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Self-assessed disability and functional performance in individuals with and without ankle instability: a case control study. J Orthop Sports Phys Ther. 2009;39(6):458–467. doi: 10.2519/jospt.2009.2989. [DOI] [PubMed] [Google Scholar]
- 42.Wikstrom EA, Fournier KA, McKeon PO. Postural control differs between those with and without chronic ankle instability. Gait Posture. 2010;32(1):82–86. doi: 10.1016/j.gaitpost.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Docherty CL, Arnold BL. Force sense deficits in functionally unstable ankles. J Orthop Res. 2008;26(11):1489–1493. doi: 10.1002/jor.20682. [DOI] [PubMed] [Google Scholar]
- 44.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 45.Yu B, Gabriel D, Noble L, Kai-Nan A. Estimate of the optimum cutoff frequency for the Butterworth low-pass digital filter. J Appl Biomech. 1999;15(3):318–329. [Google Scholar]
- 46.Monaghan K, Delahunt E, Caulfield B. Increasing the number of gait trial recordings maximises intra-rater reliability of the CODA motion analysis system. Gait Posture. 2007;25(2):303–315. doi: 10.1016/j.gaitpost.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 47.Wikstrom EA, Tillman MD, Borsa PA. Detection of dynamic stability deficits in subjects with functional ankle instability. Med Sci Sports Exerc. 2005;37(2):169–175. doi: 10.1249/01.mss.0000149887.84238.6c. [DOI] [PubMed] [Google Scholar]
- 48.Liu K, Glutting J, Wikstrom E, Gustavsen G, Royer T, Kaminski TW. Examining the diagnostic accuracy of dynamic postural stability measures in differentiating among ankle instability status. Clin Biomech (Bristol, Avon) 2013;28(2):211–217. doi: 10.1016/j.clinbiomech.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 49.Ross SE, Guskiewicz KM. Time to stabilization: a method for analyzing dynamic postural stability. Athl Ther Today. 2003;8(3):37–39. [Google Scholar]
- 50.Arnold BL, de la Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41(5):1048–1062. doi: 10.1249/MSS.0b013e318192d044. [DOI] [PubMed] [Google Scholar]
- 51.Wikstrom EA, Tillman MD, Smith AN, Borsa PA. A new force-plate technology measure of dynamic postural stability: the dynamic postural stability index. J Athl Train. 2005;40(4):305–309. [PMC free article] [PubMed] [Google Scholar]
- 52.Caffrey E, Docherty CL, Schrader J, Klossner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39(11):799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]