Abstract
Objectives
Mood disorders are prevalent in hospitalized patients. However, risk factors for early diagnosis have not been studied exclusively in surgical patients. Our study aimed to investigate the prevalence and determinants of depression and anxiety symptoms in surgical patients.
Methods
We included 392 surgical patients in this prospective cross-sectional study, which took place between June 2011 and June 2012. The Hospital Anxiety and Depression Scale (HADS) was used to screen for symptoms of depression and anxiety at weekly interviews. Regression analysis was performed to identify risk factors for early (the day after admission) and late (one week or more) in-hospital psychiatry symptoms.
Results
Depression and anxiety symptoms increased from the time of admission toward longer hospital stay. Scores obtained in the second and third weeks of admission were associated with the need for surgery while HADS in the third week was associated with lack of familial support and being under the poverty line (p < 0.050). Regression model analysis showed that early depression was associated with female gender, and early anxiety was inversely affected by female gender and protected by higher education level. A history of mood disorder was a risk factor. Later anxiety was also associated with longer hospital stay.
Conclusions
Depression and anxiety symptoms are a major concern in surgical patients especially in females and those with a history of mood disorders or lower educational level. Patients with a longer hospital stay, in particular, those with underlying diseases, postoperative complications, lack of familial support, and the need for reoperation were also at increased risk.
Keywords: Hospital Anxiety and Depression Scale, Surgery, Prevalence, Depression, Anxiety
Introduction
Depression and anxiety are common in hospitalized patients especially those waiting for surgery1-3 and with chronic or hard-to-treat conditions.4-10 Psychological disorders are not only related to a poor adjustment to hospitalization distress,11 but is associated with adverse events and unsatisfactory outcomes.3,12,13 Although the mechanism of action in psychological disorders and its relation to adverse outcomes in hospitalized patients has been explained to some extent,14,15 screening strategies to identify patients at higher risk for hospitality-related mood disorders are not robust. Moreover, risk factors for depressive and anxiety disorders in inpatient settings have not been exclusively determined.1,7,9,12,13,15
Risk stratification in hospitalized patients for mood disorders could help in identifying those with a higher probability to develop poor outcomes.16 This is of particular importance when considering that depression and anxiety disorders have been associated with readmission,2 higher morbidity17 and mortality,4 and even post-discharge psychiatric diagnosis.18 The Hospital Anxiety and Depression Scale (HADS) has been used extensively as a screening instrument for mood disorders and its appropriateness for the general population and applicability in an inpatient setting has been well documented.8,18-21
On this basis, our study sought to use the HADS to screen patients admitted to a surgical ward of a tertiary care center to determine the prevalence and risk factors for developing depression and anxiety symptoms in such a setting.
Methods
Patients admitted to the surgical ward of Shariati Hospital, affiliated with the Tehran University of Medical Sciences in Tehran, Iran, were enrolled consecutively in this prospective observational cross-sectional study, which took place between June 2011 and June 2012.
The institutional review board of Shariati Hospital approved the study protocol, which was in accordance with the tenets of the Declaration of Helsinki. The ethics committee of Tehran University of Medical Sciences granted ethical approval.
Patients aged ≥ 18 years who were conscious and cooperative and gave their informed consent were enrolled in the study. Patients with a diagnosis of current psychiatric disorder, who were taking antidepressive, anxiolytic, or antipsychotic medications, or had an altered mental status were excluded from the study.
A trained nurse used the HADS to evaluate patients’ mood symptoms at the first inpatient visit. This was either 12 hours after admission for electively scheduled surgeries or 12–24 hours after the surgery for patients undergoing emergency surgery. The questionnaire was repeated weekly until the patient was discharged. Demographics and other clinical and surgical characteristics of patients were also recorded.
HADS is a self-reported 14-item questionnaire composed of two seven-item anxiety (HADS-A) and depression (HADS-D) subscales that are rated on a Likert-type scale from zero (the least) to four (the most severe). The total score is obtained from the sum of the 14 items. For each subscale, the score is the sum of the corresponding seven scores ranging between zero and 21.21 We used a validated Persian translation of HADS in this study.22 HADS scores in each construct were divided to normal (0–7), doubtful (8–10), and definite (11–21) cases.21 To produce a binary regression model, patients with HADS scores ≥ 11 (definite cases) were compared to those with normal scores. Patients with scores in the doubtful range were not included in regression analysis.
Data were analyzed using SPSS Statistics (SPSS Inc., Chicago, US) version 16. In univariate analysis, chi-square test for categorical and independent t-test for continuous variables was used. Repeated measure analysis of variance (ANOVA) was used to determine changing pattern of HADS scores with hospital stay. A binary logistic regression analysis was also performed for early psychiatric symptoms (within 24 hours of admission) including factors with a p-value < 0.200 in the univariate analysis. HADS scores in the second week of hospital stay and beyond were not entered in regression analysis because a significant number of patients were discharged by the second week and the subsequent low expected frequency of variables for inclusion in a regression model. Data are presented as n (%) or mean ± standard deviation (SD), and odds ratio (OR) and 95% CI are provided when appropriate. A p-value < 0.050 was considered statistically significant.
Results
A total of 392 patients were enrolled in this study with a mean age of 35.1±12.9 years. The female:male ratio was 194:198 (female 49.5%, male 50.5%). Table 1 summarizes patient’s demographic, clinical, and surgical characteristics. The majority of our study population had an intermediate socioeconomic status, supportive familial relationships, and religious belief.
Table 1. Demographics and patient’s characteristics (n = 392).
| Demographics | n (%) |
|---|---|
| Age | 35.1±12.9 |
| Gender | |
| Male | 198 (50.5) |
| Female | 194 (49.5) |
| Marital status | |
| Single | 118 (30.1) |
| Married | 274 (69.9) |
| Insurance coverage | 373 (95.2) |
| Residential setting | |
| Urban | 270 (68.9) |
| Rural | 122 (31.1) |
| Education | |
| Preliminary | 19 (4.8) |
| Intermediate | 284 (72.5) |
| College | 89 (22.7) |
| Below poverty line | 52 (13.3) |
| Familial support | 367 (93.6) |
| Religious belief | 320 (81.6) |
| Strongly religious | 50 (12.8) |
| Disease-induced malformation | 13 (3.3) |
| Smoking | 49 (12.5) |
| Alcohol | 8 (2.0) |
| Illegal drug use | 7 (1.8) |
| History of mood disorder | 9 (2.3) |
| Surgery type | |
| Hepatobiliary procedure | 61 (15.6) |
| Thyroid mass | 73 (18.6) |
| Trauma surgery | 18 (4.6) |
| Abdominal wall hernia repair | 31 (7.9) |
| Breast mass | 13 (3.3) |
| Benign anorectal disease | 48 (12.2) |
| Gastrointestinal tumor resection | 22 (5.6) |
| Laparotomy due to acute abdomen | 59 (15.1) |
| Other surgeries | 24 (6.1) |
| Non-operative management | 67 (17.1) |
| Reoperation | 10 (2.6) |
| Postoperative complications | 49 (12.5) |
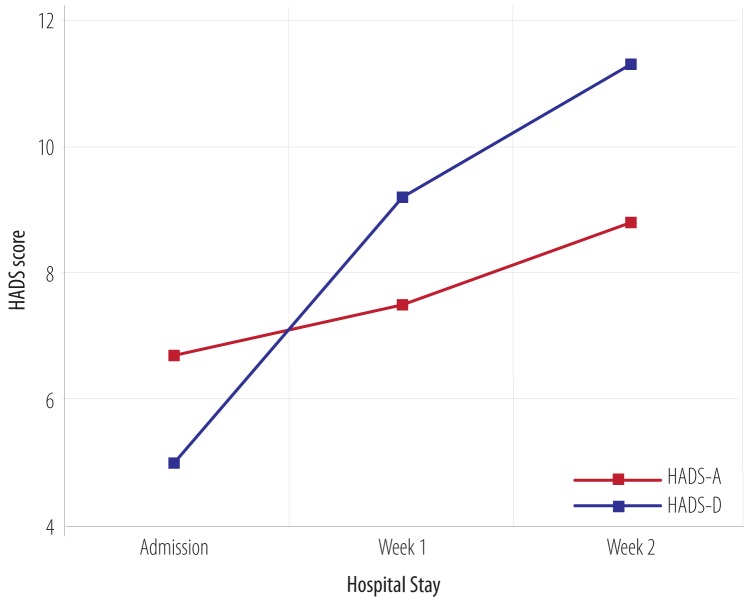
The prevalence of depressive and anxiety symptoms according to HADS definition are presented in Table 2. Definite and doubtful depression became more prevalent as the length of hospital stay increased. Although doubtful anxiety scores increased in the second week, the prevalence of definite cases decreased. Repeated measure ANOVA revealed that HADS-D score at the time of admission was 5.0±3.7, 9.2±2.5 in the first week and 11.3±1.7 in the second week (p = 0.009). Furthermore, HADS-A score was 6.7±4.0 at the time of admission, which increased significantly (p = 0.027) to 7.5±3.1 in the first week and to 8.8±3.5 in the second week [Figure 1].
Table 2. HADS subscales according to admission week, n (%).
| Score | HADS1-D1 | HADS2-D2 | HADS1-A3 | HADS2-A4 |
|---|---|---|---|---|
| Normal | 304 (77.6) | 6 (21.4) | 250 (63.8) | 13 (46.4) |
| Doubtful | 49 (12.5) | 13 (46.4) | 79 (20.2) | 13 (46.4) |
| Definite | 39 (10.0) | 9 (32.1) | 63 (16.1) | 2 (7.1) |
1HADS depression subscale at the time of admission; 2HADS depression subscale in the second week; 3HADS anxiety subscale at the time of admission; 4HADS anxiety subscale in the second week.
Figure 1.
Hospital anxiety and depression scale (HADS) scores over the course of hospital stay.
Univariate analysis was performed to identify two-sided p-values < 0.200 for HADS subscales and their predictors to include in the regression model and to determine the relationship of HADS subscales in the third week with other determinants. The analysis revealed that HADS3-D was associated with a lack of familial support and being under the poverty line (p < 0.050). HADS3-A did not demonstrate a significant relationship with any variable (p > 0.050).
Regression analysis was also carried to include predictors with a significant two-sided association of < 0.200 with HADS subscales at the time of admission and in the second week [Table 3]. Both HADS1-D and HADS1-A were associated with female gender (p = 0.040 and p = 0.002, respectively). Regarding HADS1-A, a higher education level was protective (p = 0.060) while a history of mood disorder was a risk factor (p = 0.005). HADS2-A was also associated with a longer hospital stay (p = 0.039).
Table 3. Binary logistic regression analysis according to each subscale of HADS in each week of hospitalization and associated predictors in the univariate analysis.
| Feature | Subscale | |||
|---|---|---|---|---|
| HADS1-D1 | HADS2-D2 | HADS1-A3 | HADS2-A4 | |
| Female | 2.1 (1.0–4.2) * | N/A | 2.5 (1.4–4.4) * | 1.7 (0.0–1.0) |
| Academic education | N/A | N/A | 0.6 (0.3–1) * | N/A |
| Urban living | 1.1 (0.6–2.2) | N/A | 1.4 (0.8–2.7) | N/A |
| History of mood disorder | 5.4 (0.9–33.5) | N/A | 10.7 (2.0–56.5) * | N/A |
| Serious diseases | 1 (1.0–1.1) | N/A | N/A | N/A |
| Morbidity | 0.0 (-) | N/A | N/A | N/A |
| Familial support | 0.4 (0.1–1.3) | N/A | N/A | N/A |
| Complication | 1.0 (0.4–2.8) | N/A | N/A | N/A |
| Reoperation | 0.0 (-) | N/A | N/A | N/A |
| Underlying diseases | N/A | 0.6 (0.2–2.0) | 0.9 (0.6–1.3) | N/A |
| Employed | N/A | 1.3 (0.8–1.9) | N/A | N/A |
| Alcohol | N/A | 0.0 (-) | N/A | N/A |
| Admission length | N/A | N/A | N/A | 1.1 (1.0–1.2) * |
| Need to surgery | N/A | N/A | N/A | 0.6 (0.0–1.0) |
| Reoperation | N/A | 0.0 (-) | N/A | N/A |
Data displayed as OR (95% CI). *p < 0.050. 1HADS depression subscale at the time of admission; 2HADS depression subscale in the second week; 3HADS anxiety subscale at the time of admission; 4HADS anxiety subscale in the second week. N/A: Not Applicable (p > 0.200 in univariate analysis).
Discussion
Our study was carried out in an inpatient setting to screen patients admitted to the surgical ward for symptoms of depression and anxiety. One of the unique features of our study was its exclusive discrimination between levels of HADS scores in relation to the predicting variables. Other studies have rarely distinguished between mood components and have discussed psychiatric symptoms as mood disorders.
Our findings suggest that factors including a lack of familial support, type of diseases, need for reoperation, postoperative complications, previous history of mood disorders, and unsatisfactory outcomes may play an important role in the development of mood symptoms among surgical inpatients with varying significance. A study investigating psychiatric morbidity among patients admitted for abdominal aortic surgery showed that preoperative and surgical factors were more predictive of psychiatric symptoms.1 This study, in accordance with our findings, pointed out that a high prevalence of depression and anxiety symptoms in surgical patients (58.8%) does not reflect reactivation of previous mood disorders (2.3%) but contributes to surgery-related psychiatric symptoms.
Our study showed that depression increases in surgical patients with longer hospital stay with doubtful depression scores four times more prevalent in the second week (46.4%) than at the time of admission (12.5%). Definite depression scores increased three-fold. Definite anxiety scores decreased by 50% over hospital stay while doubtful anxiety scores nearly doubled. Additionally, the prevalence of mood disorders recorded at the time of admission was 32.7% for doubtful scores compared to 26.1% for definite scores. This was much higher when compared to the prevalence of psychiatric disorders in a similar study (58.8% vs. 32%).1 In a large administrative study by Daratha et al,2 in a hospital setting, only 2.3% of adult patients who had been hospitalized for any medical conditions were diagnosed with co-occurred mood disorders. In contrast, a study by Rentsch et al,23 looking at hospitalized patients in an internal medicine department identified 26.9% of patients with depressive disorders and 11.3% with major depression based on Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria and 34.9% with depressive disorder and 18.4% with major depression according to Patient Health Questionnaire (PHQ-9) criteria.
As this study highlights and with extensive variations observed between existing studies, the diagnostic instrument used plays a major role in the reported prevalence of mood disorders among populations. However, virtually all the studies have emphasized that mood disorders in non-psychiatric patients should be attended with more seriousness.2,13,15,23,24 These mood disorders in their severe form can predispose the admitted patients to higher morbidity and mortality more than three times than general population.24,25
Depression at the time of admission was significantly associated with longer hospital stay, a previous history of mood disorders, the need for surgery or reoperation, underlying diseases, surgical complication, and lack of familial support. Indeed, these predictors are either a stressor to newly admitted patients or a supporting factor that if present would help the patients to adopt their conditions. Admission-time anxiety symptoms were significantly associated with female gender, lower educational level, and previous history of mood disorders in univariate analysis. Anxiety in the second week was also related to the need for a surgical procedure for the admission-related condition. Later depression also correlated with lack of familial support and being under the poverty line. Liberzon et al,1 identified risk factors for post-traumatic stress disorders or depressive symptoms in patients with an aortic aneurysm or occlusive diseases as younger age, having increased preoperative blood pressure and being intubated at the end of the surgery. However, in contrast to our finding that a longer hospital stay was associated with depression, their study did not confirm a longer hospital stay to be a risk factor.1
The regression model revealed that female gender is a risk factor for HADS1-D and HADS1-A. In contrast, a higher education level was protective for anxiety in the admission time while a history of mood disorders was a risk factor. Longer hospital stay also predicted more anxiety in the second week. Liberzon et al,1 also performed regression analysis showing that demographics, pre-surgical and surgical variables can predict postoperative psychiatric morbidity. However, postoperative complications, length of hospital stay, or longer intensive care unit admission did not relate to such symptoms.
Another study using HADS investigated factors associated with suicidal thoughts among hospitalized patients. The study revealed that admission to the infectious disease department and oncology and hematology units present a higher probability of suicidal ideation (7.9%, 7.8%, and 7.2%, respectively).26 Their results also revealed that suicidal ideation was associated with depression (OR 8.3), younger age (18–35 years old; OR 2.5), alcohol abuse (OR 2.3), and smoking (OR 1.8). A similar study conducted in a general hospital concluded that female gender, retired or in a disabled job-condition, low income and bad family relationships, and presence of chronic somatic illness were risk factors for depression among hospitalized patients. Depression had a high comorbidity with organic mental and anxiety disorders.27
A systematic review has recently questioned the ability of HADS to differentiate between the constructs of anxiety and depression and suggested that it should be used to measure the general aspects of distress.28 Moreover, it has been stated that HADS could not be used for diagnostic purposes. However, our study did not primarily aim to compare mood entities but to determine predictors of depression and anxiety in patients hospitalized for surgery. Future randomized clinical trials should focus on treating patients with depression and mood disorders in hospital settings to explore the cost-effectiveness of such therapeutic approach as well as preventing coincidence of psychiatric and somatic disorders.
Conclusion
Depression and anxiety symptoms are of major concern to admitted surgical patients especially in females and those with a history of mood disorders or lower educational level. Patients with longer hospital stay are also at increased risk notably with underlying diseases, postoperative complications, lack of familial support, and need for reoperation.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
The authors declared no conflicts of interest. No funding was received for this study.
Refereneces
- 1.Liberzon I, Abelson JL, Amdur RL, King AP, Cardneau JD, Henke P, et al. Increased psychiatric morbidity after abdominal aortic surgery: risk factors for stress-related disorders. J Vasc Surg 2006. May;43(5):929-934. 10.1016/j.jvs.2006.01.026 [DOI] [PubMed] [Google Scholar]
- 2.Daratha KB, Barbosa-Leiker C, H Burley M, Short R, Layton ME, McPherson S, et al. Co-occurring mood disorders among hospitalized patients and risk for subsequent medical hospitalization. Gen Hosp Psychiatry 2012. Sep-Oct;34(5):500-505. 10.1016/j.genhosppsych.2012.05.001 [DOI] [PubMed] [Google Scholar]
- 3.Burg MM, Benedetto MC, Rosenberg R, Soufer R. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med 2003. Jan-Feb;65(1):111-118. 10.1097/01.PSY.0000038940.33335.09 [DOI] [PubMed] [Google Scholar]
- 4.Fan VS, Ramsey SD, Giardino ND, Make BJ, Emery CF, Diaz PT, et al. National Emphysema Treatment Trial (NETT) Research Group Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med 2007. Nov;167(21):2345-2353. 10.1001/archinte.167.21.2345 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Disability Assessment Schedule II. World Health Organization, 2006. [Google Scholar]
- 6.World Health Organization and World Organization of Family Doctors. Integrating Mental Health into Primary Care: A Global Perspective Geneva: World Health Organization, 2008. [Google Scholar]
- 7.Pignay-Demaria V, Lespérance F, Demaria RG, Frasure-Smith N, Perrault LP. Depression and anxiety and outcomes of coronary artery bypass surgery. Ann Thorac Surg 2003. Jan;75(1):314-321. 10.1016/S0003-4975(02)04391-6 [DOI] [PubMed] [Google Scholar]
- 8.Elliott PC, Murphy BM, Oster KA, Le Grande MR, Higgins RO, Worcester MU. Changes in mood states after coronary artery bypass graft surgery. Eur J Cardiovasc Nurs 2010. Sep;9(3):188-194. 10.1016/j.ejcnurse.2009.11.010 [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen PB, Widows MR, Hann DM, Andrykowski MA, Kronish LE, Fields KK. Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosom Med 1998. May-Jun;60(3):366-371. 10.1097/00006842-199805000-00026 [DOI] [PubMed] [Google Scholar]
- 10.Douki ZE, Esmaeili MR, Vaezzadeh N, Mohammadpour RA, Azimi H, Sabbaghi R, et al. Maternal child abuse and its association with maternal anxiety in the socio-cultural context of iran. Oman Med J 2013. Nov;28(6):404-409. 10.5001/omj.2013.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tully PJ, Baker RA. Depression, anxiety, and cardiac morbidity outcomes after coronary artery bypass surgery: a contemporary and practical review. J Geriatr Cardiol 2012. Jun;9(2):197-208. 10.3724/SP.J.1263.2011.12221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koivula M, Tarkka MT, Tarkka M, Laippala P, Paunonen-Ilmonen M. Fear and anxiety in patients at different time-points in the coronary artery bypass process. Int J Nurs Stud 2002. Nov;39(8):811-822. 10.1016/S0020-7489(02)00022-6 [DOI] [PubMed] [Google Scholar]
- 13.Stundner O, Kirksey M, Chiu YL, Mazumdar M, Poultsides L, Gerner P, et al. Demographics and perioperative outcome in patients with depression and anxiety undergoing total joint arthroplasty: a population-based study. Psychosomatics 2013. Mar-Apr;54(2):149-157. 10.1016/j.psym.2012.08.009 [DOI] [PubMed] [Google Scholar]
- 14.Shapira-Lichter I, Beilin B, Ofek K, Bessler H, Gruberger M, Shavit Y, et al. Cytokines and cholinergic signals co-modulate surgical stress-induced changes in mood and memory. Brain Behav Immun 2008. Mar;22(3):388-398. 10.1016/j.bbi.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 15.Capo-Ramos DE, Gao Y, Lubin JH, Check DP, Goldin LR, Pesatori AC, et al. Mood disorders and risk of lung cancer in the EAGLE case-control study and in the U.S. Veterans Affairs inpatient cohort. PLoS One 2012;7(8):e42945. 10.1371/journal.pone.0042945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Székely A, Balog P, Benkö E, Breuer T, Székely J, Kertai MD, et al. Anxiety predicts mortality and morbidity after coronary artery and valve surgery–a 4-year follow-up study. Psychosom Med 2007. Sep-Oct;69(7):625-631. 10.1097/PSY.0b013e31814b8c0f [DOI] [PubMed] [Google Scholar]
- 17.Gasse C, Laursen TM, Baune BT. Major depression and first-time hospitalization with ischemic heart disease, cardiac procedures and mortality in the general population: a retrospective Danish population-based cohort study. Eur J Prev Cardiol 2014. May;21(5):532-540. 10.1177/2047487312467874 [DOI] [PubMed] [Google Scholar]
- 18.Gerson S, Mistry R, Bastani R, Blow F, Gould R, Llorente M, et al. Symptoms of depression and anxiety (MHI) following acute medical/surgical hospitalization and post-discharge psychiatric diagnoses (DSM) in 839 geriatric US veterans. Int J Geriatr Psychiatry 2004. Dec;19(12):1155-1167. 10.1002/gps.1217 [DOI] [PubMed] [Google Scholar]
- 19.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002. Feb;52(2):69-77. 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 20.Kathol RG, Wenzel RP. Natural history of symptoms of depression and anxiety during inpatient treatment on general medicine wards. J Gen Intern Med 1992. May-Jun;7(3):287-293. 10.1007/BF02598085 [DOI] [PubMed] [Google Scholar]
- 21.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983. Jun;67(6):361-370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 22.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health Qual Life Outcomes 2003;1:14. 10.1186/1477-7525-1-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rentsch D, Dumont P, Borgacci S, Carballeira Y, deTonnac N, Archinard M, et al. Prevalence and treatment of depression in a hospital department of internal medicine. Gen Hosp Psychiatry 2007. Jan-Feb;29(1):25-31. 10.1016/j.genhosppsych.2006.08.008 [DOI] [PubMed] [Google Scholar]
- 24.Sokal J, Messias E, Dickerson FB, Kreyenbuhl J, Brown CH, Goldberg RW, et al. Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. J Nerv Ment Dis 2004. Jun;192(6):421-427. 10.1097/01.nmd.0000130135.78017.96 [DOI] [PubMed] [Google Scholar]
- 25.Kartha A, Anthony D, Manasseh CS, Greenwald JL, Chetty VK, Burgess JF, et al. Depression is a risk factor for rehospitalization in medical inpatients. Prim Care Companion J Clin Psychiatry 2007;9(4):256-262. 10.4088/PCC.v09n0401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Botega NJ, de Azevedo RC, Mauro ML, Mitsuushi GN, Fanger PC, Lima DD, et al. Factors associated with suicide ideation among medically and surgically hospitalized patients. Gen Hosp Psychiatry 2010. Jul-Aug;32(4):396-400. 10.1016/j.genhosppsych.2010.02.004 [DOI] [PubMed] [Google Scholar]
- 27.Pakriev S, Kovalev J, Mozhaev M. Prevalence of depression in a general hospital in Izhevsk, Russia. Nord J Psychiatry 2009. Nov;63(6):469-474. 10.3109/08039480903062950 [DOI] [PubMed] [Google Scholar]
- 28.Cosco TD, Doyle F, Ward M, McGee H. Latent structure of the Hospital Anxiety And Depression Scale: a 10-year systematic review. J Psychosom Res 2012. Mar;72(3):180-184. 10.1016/j.jpsychores.2011.06.008 [DOI] [PubMed] [Google Scholar]