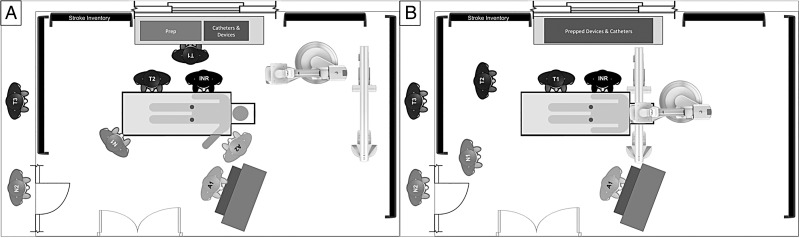
Figure 2.
INR: neurointerventionalist, T1: technician-1, T2: technician-2, T3: technician-3, N1: nurse-1, N2: nurse-2, A1: anesthesiologist/certified registered nurse anesthetist (CRNA)-1, A2: anesthesiologist/CRNA-2. During the patient preparation stage (A), T1 sets up the procedure trays and prepares the devices and catheters. T2 prepares the patient and helps the attending technician, who punctures the right femoral artery and typically places an 8 Fr sheath. The patient's left arm is extended out on an arm board for simultaneous access to anesthesia for placement of lines and administration of drugs. If there is no radial arterial access by the time the right femoral sheath is placed, the INR punctures the left femoral artery and places a 4 Fr sheath for invasive blood pressure monitoring. Even though it is possible to obtain arterial tracing via the 8 Fr right femoral sheath, placement of the 4 Fr sheath allows removal of the larger right femoral sheath at the end of the procedure. The patient is transferred to the intensive care unit with the 4 Fr sheath in place for pressure monitoring. The nurse takes a report, prepares the continuous flush lines, assists the anesthesiologist, and charts all times. The A-plane detector is stationed in such a way as to allow easy positioning over the groin in case fluoroscopy is required. For the interventional stage (B), T2 scrubs up and functions as the float. One anesthesiologist (A1) stays to cover the case, assisted by the nurse. This setup with stocked anesthesia cart is duplicated in an immediately adjacent second interventional biplane room. During working hours an additional technician (T3) and nurse (N2) are available. If two simultaneous emergent cases occur after hours, the technicians split and the backup nurse (N2) is called in.