Abstract
Aim:
To obtain information on existing practices in the diagnosis and management of gestational diabetes mellitus (GDM) among physicians/diabetologists/endocrinologists and obstetricians/gynecologists (OB/GYNs) in India.
Methods:
Details regarding diagnostic criteria used, screening methods, management strategies, and the postpartum follow-up of GDM were obtained from physicians/diabetologists/endocrinologists and OB/GYNs across 24 states of India using online/in-person surveys using a structured questionnaire.
Results:
A total of 3841 doctors participated in the survey of whom 68.6% worked in private clinics. Majority of OB/GYNs (84.9%) preferred universal screening for GDM, and screening in the first trimester was performed by 67% of them. Among the OB/GYNs, 600 (36.7%) reported using the nonfasting 2 h criteria for diagnosing GDM whereas 560 (29.4%) of the diabetologists/endocrinologists reported using the same. However, further questioning on the type of blood sample collected and the glucose load used revealed that, in reality, only 208 (12.7%) and 72 (3.8%), respectively, used these criteria properly. The survey also revealed that the International Association of Diabetes and Pregnancy Study Groups criteria was followed properly by 299 (18.3%) of OB/GYNs and 376 (19.7%) of physicians/diabetologists/endocrinologists. Postpartum oral glucose tolerance testing was advised by 56% of diabetologists and 71.6% of OB/GYNs.
Conclusion:
More than half of the physicians/diabetologists/endocrinologists and OB/GYNs in India do not follow any of the recommended guidelines for the diagnosis of GDM. This emphasizes the need for increased awareness about screening and diagnosis of GDM both among physicians/diabetologists/endocrinologists and OB/GYNs in India.
Keywords: Asian Indians, gestational diabetes mellitus, International Association of Diabetes and Pregnancy Study Groups, South Asians, World Health Organization
INTRODUCTION
Diabetes mellitus is one of the most important medical illnesses complicating pregnancy. It has been estimated that 16.8% of live births across the world in 2013 were in women who had some form of hyperglycemia in pregnancy.[1] In India, gestational diabetes mellitus (GDM) has been estimated to affect over 5 million women.[2] GDM poses serious health consequences for mother and the baby both in the short and in the long-term. In addition, this risk starts even at maternal glucose levels below those traditionally considered as diagnostic of GDM.[3] However, treatment of maternal hyperglycemia has been shown to reduce this risk almost to the level seen in women without GDM.[4]
Although most women with GDM usually return to the normoglycemic state shortly after childbirth, they still have 7 times higher risk of developing type 2 diabetes (T2DM) in future.[5] Accurate and timely diagnosis of GDM, therefore, provides a window of opportunity for intervention to reduce the growing burden of T2DM. Prioritizing postpartum care and continued follow-up will help to prevent/delay the onset of T2DM.[6] This is particularly relevant in India, which already suffers from a massive burden of T2DM.[1]
Though the importance of recognizing and managing GDM is now well-accepted, there are no universally accepted criteria for the screening and diagnosis of this condition. Despite several guidelines laid down by various organizations, controversy still exists worldwide on the optimal screening strategies and diagnostic criteria for GDM.[7] Some parts of the world follow risk-based screening whereas others follow universal screening. There is also no consensus on the diagnostic test to be used and the glucose cut-offs to be applied. Use of different criteria makes the accurate estimation of prevalence of GDM difficult[8] and raises the possibility of over- and under-diagnosis of the condition. In addition, in India, care of women with GDM is carried out by a variety of healthcare professionals (HCP). They face unique challenges in their interactions with pregnant women, leading them to favor one diagnostic approach over the other, even though such decisions may not be based on sound scientific evidence.
We, therefore, attempted to understand the perceptions and practices of two important categories of HCPs involved in the care of GDM in India (physicians/diabetologists/endocrinologists and obstetricians/gynecologists [OB/GYNs]), regarding diagnosis, management, and follow-up of GDM. The results from this study will help to gauge the different screening methods and diagnostic criteria employed in India for the diagnosis and management of GDM, and thus understand the gaps and highlight target areas for improvement with regard to provision of care for women with GDM.
Aim
The present study aims to obtain information on existing practices for the diagnosis and management of GDM among physicians/diabetologists/endocrinologists and OB/GYNs from different parts of India.
METHODS
A nationwide survey on the practice patterns with respect to diagnosis and management of GDM was carried out covering physicians/diabetologists/endocrinologists and OB/GYNs from 24 states of India. Data collection involved two methods: Self-completed questionnaires and an online web-based software.
Questionnaires were handed over directly to the doctors to be filled on the spot and returned. The online questionnaire was filled through customized web-based software called “WINGS Survey” created by the Madras Diabetes Research Foundation. The frontend software was developed using Microsoft ASP.NET, and the data collected was stored in the Microsoft SQL server 2000 database.
The questionnaire addressed different screening techniques employed; GDM diagnostic guidelines and diagnostic cut-offs based on blood glucose levels; management and follow-up, pharmacotherapy and postpartum follow-up. Several of the questions allowed multiple responses leading to the reported percentage adding up to more than 100%.
RESULTS
A total of 3841 doctors (2020 physicians/diabetologists/endocrinologists and 1821 OB/GYNs) participated in the survey. The survey covered 24 states of India including the National Capital Territory of Delhi and two union territories, Chandigarh, and Puducherry. Figure 1 shows the state wise percentage distribution of physicians/diabetologists/endocrinologists and OB/GYNs, who participated in the survey.
Figure 1.
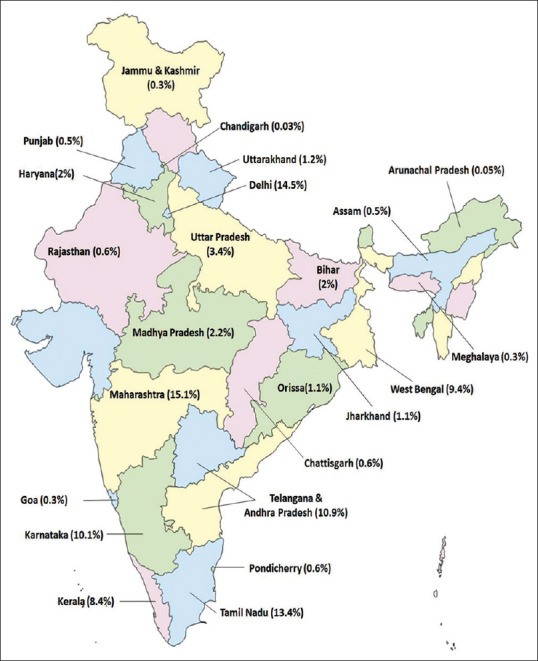
Percentage of respondents in different states of India
Primary institution of practice
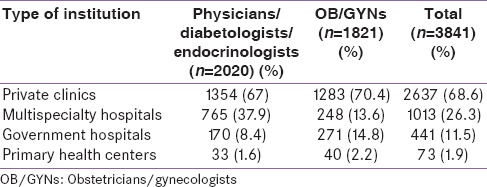
More than half of the doctors who participated in the survey practiced in private clinics and hospitals whereas the rest worked in multispecialty hospitals and government hospitals [Table 1].
Table 1.
Type of institution where the doctors practised
Universal screening versus risk-based screening
The vast majority of the OB/GYNs (84.9%) screened all pregnant women for GDM, i.e., universal screening while 14.5% preferred to do only risk-based screening. The rest (0.6%) reported that they do not screen for GDM in pregnant women [Figure 2].
Figure 2.
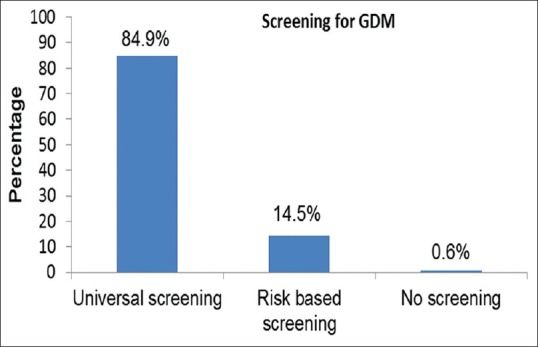
Screening for gestational diabetes mellitus – universal versus risk based screening
Mean week of gestation at which screening was performed
Most of the OB/GYNs performed screening for GDM in the first trimester (18.8% at booking and 49% between 8 and 20 weeks). The screening was performed between 20 and 28 weeks by 40% and after 28 weeks by 2.8%. This question allowed multiple responses, and hence, the percentages reported are more than 100.
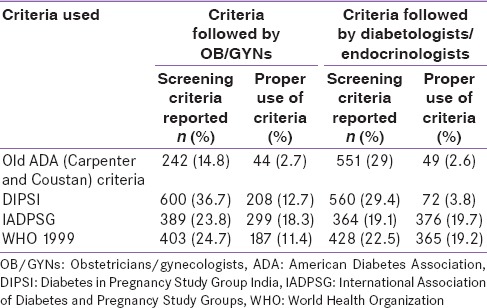
Guidelines used to diagnose gestational diabetes mellitus
Among the 1634 (89.7%) OB/GYNs who responded to this question, 600 (36.7%) reported using the Diabetes in Pregnancy Study Group India (DIPSI) criteria, 403 (24.7%), the World Health Organization (WHO) 1999 criteria, 389 (23.8%), the International Association for Diabetes and Pregnancy Study Groups (IADPSG) criteria, and 242 (14.8%), the American Diabetes Association (ADA)[6] 2-step method (50 g glucose challenge test followed by 100 g 3 h glucose tolerance test with the cut-offs proposed by Carpenter and Coustan[9] or the National Diabetes Data Group).[10]
Among the physicians/diabetologists/endocrinologists, 1903 (94.2%) responded to this question, out of whom 560 (29.4%) reported using the DIPSI criteria, 428 (22.5%) the WHO 1999 criteria, 364 (19.1%), the IADPSG criteria, and 551 (29%) the ADA criteria.
However, as shown in Table 2, responses to subsequent questions on type of blood sample collected, the glucose load used, and the cut-offs as per the criteria revealed that 54.9% OB/GYNs and 54.7% diabetologists/endocrinologists did not correctly follow any of the criteria.
Table 2.
Screening criteria for gestational diabetes mellitus followed by the obstetricians/gynecologists and physicians/diabetologists/endocrinologists
Use of insulin and oral hypoglycemic agents for treatment
When women required pharmacological treatment to manage their GDM, 1019 (50.4%) of diabetologists/endocrinologists said they used insulin for all women with GDM, 758 (37.5%) said they used insulin only for some, and 243 (12.1%) reported using no insulin at all. Among those who preferred using oral hypoglycemic agents, metformin was used by 1087 (53.8%) of diabetologists/endocrinologists, sulfonylureas by 72 (3.6%), and a combination of the two by 247 (12.2%) whereas 591 (29.3%) reported no use of oral hypoglycemic agents (OHAs) and 23 (1.1%) reported using other OHAs such as alpha-glucose inhibitors.
Timing of delivery of women with gestational diabetes mellitus
The majority of OB/GYNs (78.3%) routinely delivered women with GDM before 38 weeks’ gestation whereas 10.9% waited beyond 38 weeks and 10.8% up to 40 weeks.
Postpartum follow-up of women with gestational diabetes mellitus
Fifty-six percent of physicians/diabetologists/endocrinologists and 71.6% OB/GYNs said they advised women with GDM to undergo oral glucose tolerance testing (OGTT) after delivery. OGTT was advised within 6 weeks of delivery by 42.4% of diabetologists/endocrinologists and 44.2% of OB/GYNs, and between 6 and 2 weeks after delivery by 48% of diabetologists/endocrinologists and 49.4% of OB/GYNs.
DISCUSSION
It is evident from our survey that the majority of doctors in India prefer universal screening for gestational diabetes. This is consistent with findings from an online survey conducted by Divakar and Manyonda[8] in 2011 among physicians in India and is in line with the DIPSI guidelines, which favor universal screening as well as with many of the international guidelines, which recommend that all women of high-risk ethnicity be screened for GDM.[6,11] As the prevalence of GDM is almost 11-fold higher in Indian women when compared to their Caucasian counterparts,[12,13,14,15] universal screening is an essential tool in India to ensure that no case of GDM or preexisting diabetes is missed out.
It is heartening to note that the majority of OB/GYNs screen their antenatal patients for diabetes in the first trimester itself. Delaying screening till the second trimester carries the risk of missing preexisting (pregestational) diabetes, especially in a population such as India, where the background prevalence of T2DM is high.[1] It would, however, be ideal if all pregnant women (as opposed to 18.8% in the present survey) were to be screened at the first booking visit itself as recommended by the guidelines.[12]
The multiplicity of available criteria for the diagnosis of GDM, and frequent changes in recommendations made by international organizations, have led to confusion among HCPs as to the best screening test to be used for GDM. This is reflected in the results of our survey where a variety of guidelines were reported to be used by OB/GYNs and physicians/diabetologists/endocrinologists for diagnosing GDM. What is even more worrisome is that the majority of HCPs applied these criteria incorrectly, raising the possibility of over- and under-diagnosis of GDM in India. For example, 36.7% OB/GYNs and 29.4% physicians/diabetologists/endocrinologists said they used the DIPSI criteria, but in reality, only 12.7% and 3.8%, respectively, used the DIPSI criteria. Our results highlight the need for creating greater awareness among HCPs regarding the currently accepted guidelines for the diagnosis of GDM so that the majority of women with GDM are accurately identified and appropriately managed.
Insulin is the first-line pharmacologic therapy for GDM;[16] however, there is some evidence that OHAs such as metformin are safe in pregnancy.[17] Decision-making with respect to the initiation of insulin is often driven by patient preference. Data from our survey shows that more than half of the physicians/diabetologists/endocrinologists preferred to use insulin for women with GDM. When OHA were preferred, 53.8% reported the use of metformin, 3.6% used sulfonylurea alone, and 12.2% used both. It is a matter of some concern that 1.1% of all physicians/diabetologists/endocrinologists reported using “other” OHAs during pregnancy (none of which have been approved for use in this setting).
There is little consensus regarding the preferred method and timing of delivery in women with gestational diabetes, which is usually based on expert opinion. In the absence of any maternal or fetal complications, OB/GYNs routinely deliver at 40 weeks of gestation.[16] However, our survey reports that majority of the OB/GYNs deliver their patients before 38 weeks, presumably to minimize the risk of sudden intra uterine death during the 3rd trimester, which has been shown to occur despite intensive fetal surveillance.
It is critical to check glucose levels postpartum in women with GDM. Nearly, 50% of these women develop T2DM within 5–10 years after delivery.[18] They are also at risk of development of GDM at an earlier stage during subsequent pregnancies. Thus, regular screening for T2DM should be strongly encouraged. Many organizations have issued guidelines for postpartum follow-up of women with GDM. The ADA recommends that women with GDM should undergo screening for T2DM with OGTT, 6 weeks after delivery.[19] Although guidelines for postpartum care are established, data from our survey reports that not all diabetologists/endocrinologists and OB/GYNs advise postpartum OGTT. A possible explanation could be that many physicians do not prioritize these guidelines in practice or may view another health practitioner as responsible for the follow-up. Omitting this important piece of advice will lead to the majority of women with GDM remaining unaware of their glycemic status postdelivery, and thereby running the risk of entering another pregnancy with undiagnosed diabetes, as well as accumulating prolonged duration of unrecognized, uncontrolled hyperglycemia.
CONCLUSION
Both physicians/diabetologists/endocrinologists as well as OB/GYNs have an enormous responsibility for providing proper care and management for women with GDM. This large survey conducted all over India, covering 24 states reveals that more than half of the diabetologists/endocrinologists and OB/GYNs in India do not follow any of the recommended guidelines for the diagnosis of GDM possibly due to lack of awareness about these guidelines. This emphasizes the need for increased awareness about screening and diagnosis of GDM both among physicians and OB/GYNs. It is imperative to also improve adherence to postpartum follow-up testing. Proper educational intervention to address these gaps will help doctors to understand their role in promoting better pregnancy outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The WINGS program has been developed through a partnership between the International Diabetes Federation, the Madras Diabetes Research Foundation in Chennai, India, and the Abbott Fund, the philanthropic foundation of the global healthcare company Abbott. We would also like to place on record our sincere thanks to all the health care professionals for participating in the study. We also wish to thank M/S Sanofi, India, for their help with this survey. This is the fifth publication from the WINGS project (WINGS-5).
REFERENCES
- 1.6th ed. Brussels, Belgium: International Diabetes Federation; 2013. International Diabetes Federation. IDF Diabetes Atlas. [PubMed] [Google Scholar]
- 2.International Diabetes Federation. Policy Briefing. Diabetes in Pregnancy: Protecting Maternal Health. Brussels: IDF. 2011. [Last accessed on 2015 Nov 30]. Available from: http://www.idf.org/diabetes-pregnancy-protecting-maternal-health .
- 3.HAPO Study Cooperative Research Group. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 4.Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86. doi: 10.1056/NEJMoa042973. [DOI] [PubMed] [Google Scholar]
- 5.Kayal A, Anjana RM, Mohan V. Gestational diabetes – An update from India. Diabetes Voice. 2013;58:30–4. [Google Scholar]
- 6.American Diabetes Association. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38(Suppl 1):S8–S16. doi: 10.2337/dc15-S005. [DOI] [PubMed] [Google Scholar]
- 7.Mohan V, Mahalakshmi MM, Bhavadharini B, Maheswari K, Kalaiyarasi G, Anjana RM, et al. Comparison of screening for gestational diabetes mellitus by oral glucose tolerance tests done in the non-fasting (random) and fasting states. Acta Diabetol. 2014;51:1007–13. doi: 10.1007/s00592-014-0660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Divakar H, Manyonda I. Battling with rising prevalence of gestational diabetes mellitus: Screening and diagnosis. Int J Infertil Fetal Med. 2011;2:96–100. [Google Scholar]
- 9.Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144:768–73. doi: 10.1016/0002-9378(82)90349-0. [DOI] [PubMed] [Google Scholar]
- 10.National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes. 1979;28:1039–57. doi: 10.2337/diab.28.12.1039. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence (NICE) Diabetes in Pregnancy: Management of Diabetes and its Complications from Preconception to the Postnatal Period. Clinical Guideline NG3. 2015. [Last accessed on 2015 Oct 24]. Available from: http://www.nice.org.uk/guidance/ng3/resources/diabetes-in-pregnancy-management-of-diabetes-and-its- complications-from-preconception-to-the-postnatal-period- 51038446021 .
- 12.Diabetes in Pregnancy Study Group. Seshiah V, Das AK, Balaji V, Joshi SR, Parikh MN, Gupta S. Gestational diabetes mellitus – guidelines. J Assoc Physicians India. 2006;54:622–8. [PubMed] [Google Scholar]
- 13.Dornhorst A, Paterson CM, Nicholls JS, Wadsworth J, Chiu DC, Elkeles RS, et al. High prevalence of gestational diabetes in women from ethnic minority groups. Diabet Med. 1992;9:820–5. doi: 10.1111/j.1464-5491.1992.tb01900.x. [DOI] [PubMed] [Google Scholar]
- 14.Beischer NA, Oats JN, Henry OA, Sheedy MT, Walstab JE. Incidence and severity of gestational diabetes mellitus according to country of birth in women living in Australia. Diabetes. 1991;40(Suppl 2):35–8. doi: 10.2337/diab.40.2.s35. [DOI] [PubMed] [Google Scholar]
- 15.Metzger BE, Coustan DR. Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee. Diabetes Care. 1998;21(Suppl 2):B161–7. [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists. ACOG practice bulletin. ACOG practice bulletin: Clinical management guidelines for obstetrician – Gynecologists. Obstet Gynecol. 2001;98:525–38. [PubMed] [Google Scholar]
- 17.Perkins JM, Dunn JP, Jagasia SM. Perspectives in gestational diabetes mellitus: A review of screening, diagnosis, and treatment. Clin Diabetes. 2007;25:57–62. [Google Scholar]
- 18.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care. 2002;25:1862–8. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association. Gestational diabetes mellitus. Diabetes Care. 2004;27(Suppl 1):S88–90. doi: 10.2337/diacare.27.2007.s88. [DOI] [PubMed] [Google Scholar]


