Abstract
We often see painful ankle joint destruction with painful hindfoot valgus deformity in rheumatoid arthritis. Our policy in such cases has been to first correct the hindfoot deformity in the subtalar joint with fusion, but then ankle joint pain has been observed. Two women with rheumatoid arthritis underwent correction and fusion surgery for hindfoot valgus deformity. They had been using wheelchairs because of severe pain in the ankle joint and hindfoot despite extensive medical treatment. After surgery, both patients complained of no pain in the hindfoot. Furthermore, dramatic pain reduction in the ankle joint was also observed especially in a case without ankle joint instability. Consequently, the patients could walk without any support. Correction of valgus hindfoot deformity contributes to centralizing the weight-bearing line in the ankle joint, leading to ankle joint pain relief. It appears possible to preserve the ankle joint without additional ankle surgery even in rheumatoid arthritis cases, if ankle is stable.
Keywords: Rheumatoid arthritis, ankle joint pain, painful valgus hindfoot deformity, correction of subtalar joint with fusion, displacement of weight-bearing line
Introduction
If patients suffer from destructive changes of the ankle joint and valgus hindfoot simultaneously, there is no clear surgical guideline for such a situation. In previous reports, simultaneous arthrodesis surgery of both the ankle joint and the subtalar joint using an intramedullary nail and plate was recommended1,2 in severe ankle and hindfoot deformity. However, it is often difficult to determine which joint (ankle joint or subtalar joint) is predominantly responsible for the patient’s pain. Furthermore, fusion through the tibia and calcaneus provides no hindfoot mobility. If possible, joint preservation is desirable to maintain mobility. Then, in such cases, our policy has been to first correct the valgus hindfoot deformity in the subtalar joint and then fuse, and changes in the ankle joint pain have been observed.
Methods
Patient demographics
Case 1
A 63-year-old woman with a 10-year history of rheumatoid arthritis (RA) (functional class III, radiographic stage IV) had been treated with 10-mg methotrexate (MTX)/week for 10 years. Prednisolone was also used at 5 mg/day. The patient had severe pain in the ankle joint and the subtalar joint (with tenderness at ankle joint, sinus tarsi, and medial opening of tarsal canal) for several months. Consequently, she required a wheelchair for the preceding month. The radiographic degree of ankle joint destruction was assessed using the method described by Larsen et al.3 The affected ankle was classified as grade 4 (complete loss of joint space).
Case 2
A 60-year-old woman with a 7-year history of RA (functional class III, radiographic stage IV) had been treated with 8-mg MTX/week for 7 years. Tocilizumab at 8 mg/kg was introduced in the 4-week intervals between the regular treatments. Furthermore, she also received prednisolone at 9 mg/day. She had severe pain in the ankle joint and subtalar joint (with tenderness at ankle joint, sinus tarsi, and medial opening of tarsal canal) for several months. Consequently, she required a wheelchair for the preceding month. The radiographic degree of the affected ankle destruction was grade 4.
Surgical procedure and postoperative procedure
Surgery was carried out using the lateral approach. The subtalar joint including the sinus tarsi was identified, followed by synovectomy and decortication. After that, varus correction was added with fusion using k-wires, screws, and staples. In the bony defect, autograft and/or allograft bone was transplanted. In case 1, a calcaneal osteotomy was also performed. After surgery, the ankle was immobilized in a below-knee cast for 2 months with non-weight bearing. After 2 months, the patients were allowed to start partial weight-bearing, and after an additional 2 weeks, full weight-bearing was allowed.
Clinical evaluation
To evaluate the pain, a visual analog scale (VAS) was used, and to evaluate general clinical outcomes, the American Orthopedics Foot and Ankle Society (AOFAS) ankle–hindfoot score4 was evaluated pre- and postoperatively (case 1: 17 months, case 2: 8 months after surgery).
Radiological evaluation
X-ray radiographs of the anterior–posterior and lateral views of the ankle joint were made. A subtalar view was also taken to check the tibio-calcaneal (TC) angle. After surgery, varus/valgus stress views of the ankle joint were also taken to detect the reason for the difference in ankle joint pain between case 1 and case 2.
Results
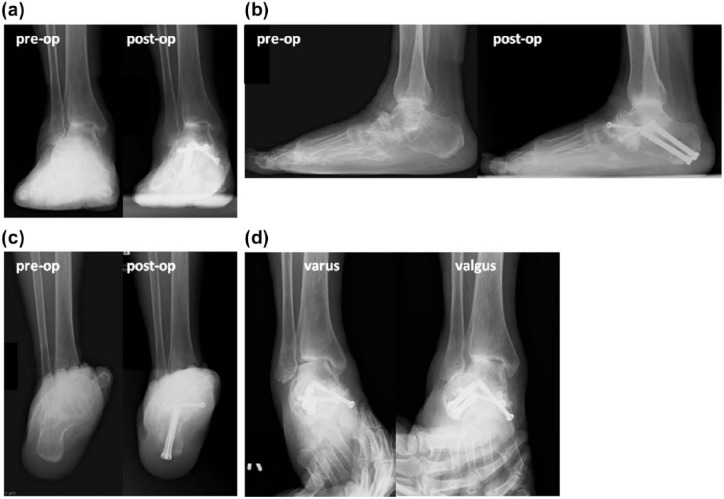
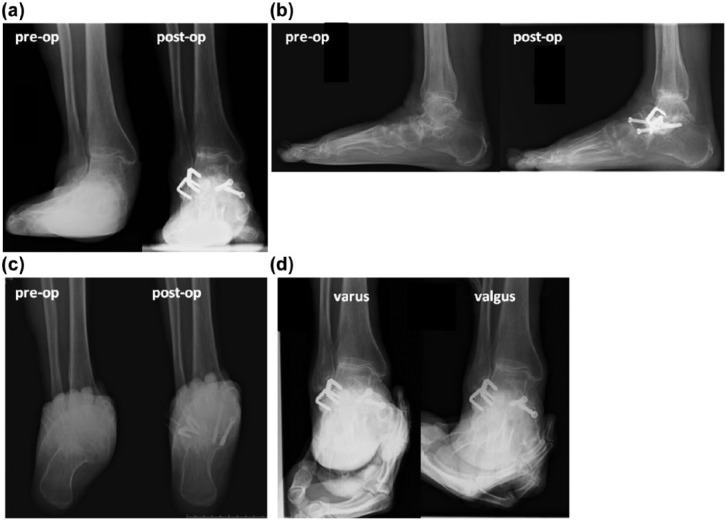
Both patients complained of no subtalar pain; furthermore, dramatic pain relief in the ankle joint was also observed (VAS, case 1: 90–15 mm, case 2: 90–5 mm). Both patients could walk without any support. However, some limitations in daily living or recreational activities remained with dysfunction and pain of other joints. The AOFAS ankle–hindfoot score was also improved (case 1: 7 (pain: 0, functional: 7) to 59 (pain: 30, functional: 29); case 2: 7 (pain: 0, functional: 7) to 77 (pain: 30, functional: 47)). Radiological findings showed complete bony fusion in both cases (Figures 1 and 2), and the TC angle showed clear improvement in hindfoot valgus deformity (case 1: 17° preoperatively to 7° postoperatively, case 2: 24° preoperatively to 6° postoperatively) (Figures 1(c) and 2(c)). Valgus tilt of the talus against the joint surface of the tibia was decreased, especially in case 2 (Figure 2(a)). In addition, in the varus/valgus stress views, case 1 showed instability in the ankle joint, while case 2 showed no instability (Figures 1(d) and 2(d)).
Figure 1.
Preoperative and follow-up weight-bearing radiographs. (a) Anteroposterior view, (b) lateral view, and (c) subtalar joint view are shown. The left panel shows the preoperative findings, and the right panel shows the postoperative findings (17 months). Calcaneal pitch and the longitudinal internal arch are increased, and the TC angle (calcaneal offset) is decreased postoperatively. (d) Varus and valgus stress radiographs in the anteroposterior view. There is instability in the ankle joint and the tibio-fibular ligament.
TC: tibio-calcaneal.
Figure 2.
Preoperative and follow-up weight-bearing radiographs. (a) Anteroposterior view, (b) lateral view, and (c) subtalar joint view are shown. The left panel shows the preoperative findings, and the right panel shows the postoperative findings (8 months). The longitudinal internal arch is increased, and the TC angle (calcaneal offset) is decreased postoperatively. The supinated foot deformity is also improved. (d) Varus and valgus stress radiographs in the anteroposterior view. There is no instability in the ankle joint.
Discussion
For the treatment of end-stage osteoarthritis (OA), low tibial osteotomy (LTO) is widely performed as a novel procedure.5,6 In this procedure, corrective osteotomy is performed at the distal tibia to correct the displacement of weight-bearing line. Then, it is plausible to understand that correction even in hindfoot could also improve the displacement of weight-bearing line passing the ankle joint. Thus, first, we selected hindfoot correction to preserve the ankle joint mobility, and then ankle pain has been observed. Instability of the ankle joint is also an important factor for ankle pain. Radiological evaluation revealed some varus/valgus instability in case 1, while there was no varus/valgus instability in case 2. This may also be one of the possible reasons that case 1 continued to have a small amount of pain in the ankle joint, while case 2 had none.
Although this study had a very small number of cases, it appears possible to preserve the ankle joint without additional ankle surgery even in RA cases, if ankle joint is stable. Continuous observation and possible tight control of RA by medical treatment are, of course, required, because RA is a degenerative and inflammatory disease. However, it is proper to suggest that all clinicians involved in RA treatment, rheumatologists, orthopedic surgeons, and nurses should keep in mind the importance of correction of hindfoot deformity.
Acknowledgments
We greatly thank Dr Masato Matsushita, Dr Shiro Ohshima, and Dr Yukihiko Saeki for their medical treatment against RA and supporting us. We also greatly thank medical assistants in the hospital for supporting us.
Footnotes
Declaration of conflicting interests: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Research ethics and patient consent: This research was approved by the Institutional Ethical Review Board at the National Hospital Organization, Osaka Minami Medical Center (approval number: 23-10), and written informed consent was obtained from the patients.
References
- 1. Niinimäki TT, Klemola TM, Leppilahti JI. Tibiotalocalcaneal arthrodesis with a compressive retrograde intramedullary nail. A report of 34 consecutive patients. Foot Ankle Int 2007; 28: 431–434. [DOI] [PubMed] [Google Scholar]
- 2. Myerson MS, Alvarez RG, Lam PW. Tibiocalcaneal arthrodesis for the management of severe ankle and hindfoot deformities. Foot Ankle Int 2000; 21: 643–650. [DOI] [PubMed] [Google Scholar]
- 3. Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn 1977; 18: 481–491. [DOI] [PubMed] [Google Scholar]
- 4. Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994; 15: 349–353. [DOI] [PubMed] [Google Scholar]
- 5. Takakura Y, Tanaka Y, Kumai T, et al. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br 1995; 77: 50–54. [PubMed] [Google Scholar]
- 6. Tanaka Y, Takakura Y, Hayashi K, et al. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Br 2006; 88: 909–913. [DOI] [PubMed] [Google Scholar]