Abstract
Aims
The purpose of this study was to determine the efficacy and stability of the biodegradable fixation system for treatment of mandible fractures in pediatric patients by measuring the bite force.
Methods
Sixty pediatric patients with mandibular fractures (36 males, 24 females) were included in this study. The 2.5-mm resorbable plates were adapted along Champy's line of ideal osteosynthesis and secured with four 2.5 mm diameter monocortical resorbable screws, 8 mm in length. All patients were followed for 10 months. Clinical parameters, such as soft tissue infection, nonunion, malunion, implant exposure, malocclusion, nerve injury, and bite force for stability, were prospectively assessed.
Results
Adequate fixation and primary bone healing was achieved in 100% of the cases. Six minor complications (10%) were observed: 2 soft tissue infections (3%), 1 plate dehiscence (2%), 1 malocclusion (2%), and 2 paresthesia (3%).
Conclusion
2.5-mm resorbable plating system along Champy's line of ideal osteosynthesis is a good treatment modality for mandible fractures in pediatric patients.
Keywords: Maxillomandibular fixation, Hydrolysis, Polylactic acid (PLA), Polyglycolic acid (PGA)
1. Introduction
Successful treatment of mandible fractures signifies an anatomic bony union with restoration of normal occlusion and function. Mandibular fractures may be either treated conservatively or with open reduction and internal fixation. The principles of management of mandibular fractures differ in children. While in adults, absolute reduction and fixation of fractures is indicated, minimal manipulation of facial skeleton is mandated in children. The goal of fracture management is to restore the underlying bony architecture to preinjury position, in a stable fashion, as noninvasively as possible, with minimal residual esthetic and functional impairment.
Most fractures are treated conservatively by splints with circummandibular wires and maxillomandibular fixation; but in unstable fractures, internal fixation using miniplates is required. Titanium plates have been the gold standard for internal fixation of mandible fractures.1 Resorbable plating systems have been used for midface, craniofacial, and pediatric fracture cases. The purpose of this study was to determine the efficacy and stability of the biodegradable fixation system in the treatment of pediatric mandible fractures by measuring the bite force.
2. Methodology
Sixty children with mandible fractures, who reported to our outpatient department over a period of one and half years, were included in the study, irrespective of age, sex, caste, religion, socioeconomic status, and nature of injury. Inclusion criteria include normal healthy individuals with no debilitating systemic and bony diseases, and single, noncomminuted mandibular fractures (symphysis, parasymphysis, body, angle) where open reduction was indicated (Fig. 1). An informed consent was obtained from their parents prior to their enrollment in the study. Exclusion criteria include infected fracture site, undergoing steroid therapy, pathological fracture, and concomitant condylar, coronoid fractures, and midface fractures.
Fig. 1.

Intraoral view of fracture and deranged occlusion.
Pediatric patients having mixed and permanent dentition in the age range of 8–15 years were included in the study. Preoperative detailed history was recorded. Careful examination of the soft tissues and underlying facial skeleton excluded any other associated injuries. Radiographs (Fig. 2) and routine blood investigations were advised and parents were informed of the treatment plan. Prophylactic antibiotic coverage and analgesics were prescribed. Mean duration between injury and surgery was 2 days.
Fig. 2.
Preoperative O.P.G.
Nasotracheal intubation was done and all fractures were treated under general anesthesia. Fractures were treated either intraorally with vestibular/mucosal incision or extraorally through existing traumatic scar. Extraction of teeth in the line of fracture was performed if the tooth was fractured, periodontally involved, nonrestorable, grossly carious, or interfering with reduction of fracture, or occlusion. Either a splint was made after impression or interdental eyelet wiring was done prior to surgery.
Ideal occlusion was achieved using maxillomandibular fixation, and fractures were reduced. 2.5-mm INION – CPS plating kit was used for plating (Fig. 3 and 4). A four-hole resorbable plate was adapted along Champy's line of ideal osteosynthesis after being immersed in a sterile water bath at 55 °C for 15 s, and was secured with four 8 mm length, 2.5 mm diameter monocortical screws, using a drill–tap–screw sequence (Fig. 5). Care was taken to place the screws lateral to roots and superior to neurovascular bundle, with a minimum of two screws in the proximal and distal segments of the fracture. Interforaminal fracture involving symphysis and parasymphysis was fixed with 2 four-hole resorbable plates. The area was irrigated and closed with resorbable sutures. All patients received a postoperative course of intravenous antibiotics and chlorhexidine oral rinse upon discharge. A short-term postoperative IMF for 2 weeks was done. Patients were followed for bite force, temporo-mandibular joint function, esthetics, and complications if any.
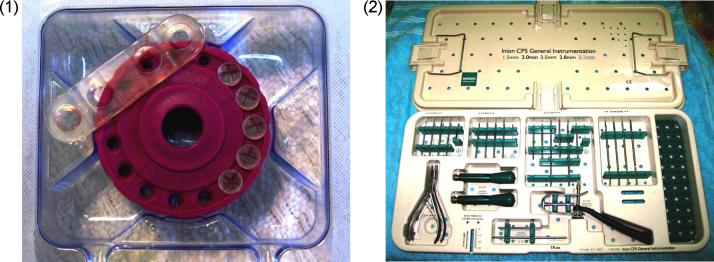
Figs. 3 and 4.
INION – CPS plating kit containing plates and screws.
Fig. 5.
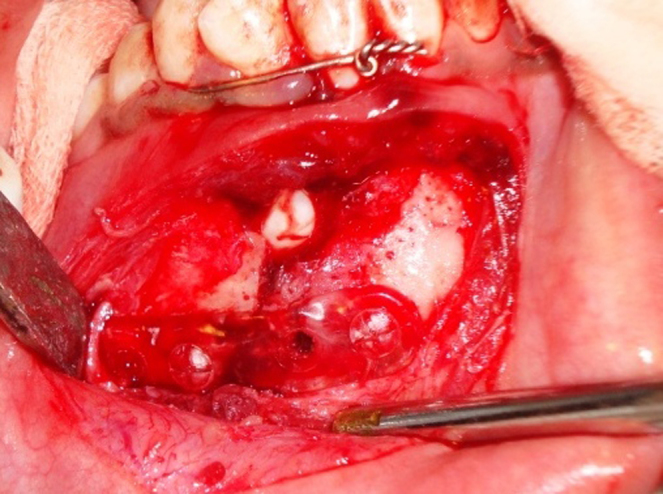
Intraoperative view of reduction and plate fixation.
2.1. Bite force recording
Bite force recordings were made using indigenous Bite Force Recorder, designed at Research Design and Standard Organization, Lucknow. The recorder consists of four strain gauges mounted on steel bar forming a wheatstone bridge. Load changes in steel bar produces measurable voltage changes across the strain gauges, which were converted into the kilogram force (kp). Bite forces were recorded at the bilateral molar region and incisor region.
3. Results
In the present study, 60% were male and 40% were females. 55% of the mandibular fractures were in body, 25% at angle, and 20% in the parasymphyseal region. Biodegradable fixation system provided satisfactory stability to enable bone healing during the initial phase, as bone healing was achieved in all fractures (100%) with satisfactory alignment of fracture segments, reproducible preinjury occlusion, normal temporomandibular joint function, and satisfactory esthetics, as determined clinically and radiographically (Fig. 6, Fig. 7).
Fig. 6.
Postoperative OPG showing healing of fracture.
Fig. 7.

Postoperative Occlusion.
Bite force analysis showed an increased stability and masticatory function at incisor and molar regions at all monthly follow-ups. (Table 1, Table 2). Table 3 demonstrates the complications observed.
Table 1.
Bite force assessment in incisor region.
| Bite force (mean ± SD) | Change in bite force (mean ± SD) | ‘t’ value | ‘p’ value | |
|---|---|---|---|---|
| 2 weeks | 3.58 ± 1.281 | – | – | – |
| 3 months | 5.25 ± 1.624 | 1.670 ± 0.786 | 8.886 | <0.0001 |
| 6 months | 6.71 ± 1.795 | 3.13 ± 1.144 | 11.449 | <0.0001 |
Significant increase in bite force at 3 months and 6 months, from 2nd week onwards.
Table 2.
Analysis of bite force in molar region.
| Bite force (mean ± SD) | Change in bite force (mean ± SD) | ‘t’ value | ‘p’ value | |
|---|---|---|---|---|
| 2 weeks | 6.11 ± 1.846 | – | – | – |
| 3 months | 11.385 ± 1.934 | 7.245 ± 2.038 | 14.880 | <0.0001 |
| 6 months | 17.14 ± 2.443 | 12.030 ± 3.076 | 18.373 | <0.0001 |
Table 3.
Complications.
| Complications | Numbers (%) |
|---|---|
| Soft tissue infection | 2 (3%) |
| Nerve injury (paresthesia) | 2 (3%) with body fracture for 4 weeks, resolved at further follow-up |
| Implant exposure | 1 (2%) at 3rd week follow-up |
| Malunion, nonunion | 0 |
| Malocclusion | 1 (2%) |
| Total | 6 (10%) |
4. Discussion
Pediatric fractures are rare and estimated to occur in 5% of all maxillofacial trauma.2 Approximately 40% of all pediatric fractures involve mandible.3 The basic treatment principles differ from the adult population because of the mixed dentition, unerupted teeth, and the ongoing growth.4 Hence, these patients present with their own unique treatment requirements. Treatment of mandible fractures with titanium plates5 and lag screws6 has been applied to improve osteosynthesis at mandibular fracture sites for decades. There are reported disadvantages, such as osteoporosis,7 implant migration,8 release of metal ions,9 extrusion,10 stress shielding,11 artifacts on radiographic examinations,12 restrictions on growth in children,13, 14 and thermal sensitivity.15 Other disadvantages of titanium plating include palpability, thermal sensitivity, image interference, transcranial migration in pediatric cases,16 growth inhibition when placed across growth sutures, and the need for secondary hardware removal surgery.17 The reported removal rates of nonresorbable plates are as 12–18%, with infection as the major cause in 50–60% of cases.18, 19
In 1966, Kullkarni first applied bioresorbable materials for the fixation of maxillofacial bones.20 These plates were made of polymers consisting of varying compositions of polylactic acid (PLA) and polyglycolic acid (PGA). Many problems had been encountered,21 such as foreign body reactions and persistence of the material in the body for periods longer than desired. Development of polymer technology and regulation of PLA/PGA ratios make it completely biocompatible, with adequate biomechanical resistance and elimination from body without causing any foreign body reaction. The INION resorbable plates and screws consist of an amorphous injection-molded copolymer of l-lactide/d-lactide/trimethylene carbonate. These plates resorb slowly, maintaining 70% of their strength at 9–14 weeks, and losing their strength steadily thereafter. There is a 42% bulk resorption at 40 weeks and then complete resorption by 2–4 years. The mechanism of plate and screw resorption is hydrolysis of the long polymer chains into shorter water-soluble fragments and then metabolism via Krebs cycle and excretion as CO2 and water. This product retains more than 100 MPa of its strength after 6 months and converts into carbon dioxide and water by the process of bulk hydrolysis and absorbs completely in approximately 36–60 months.22 The absorption happens in two phases: hydrolysis and fragmental metabolization.23 Hydrolysis occurs when body fluids enter the implant and chemically react with the polymer and break the polymer chains. Fragmental metabolization occurs as the polymer continues to fragment until single lactic acid molecules are finally metabolized in the liver into carbon dioxide and water.24
The mechanical strength of bioresorbable plates is weaker than that of metal plates. Through advances in bioengineering and technology, contemporary resorbable plate systems have almost achieved similar strength levels compared to metal plates.
Kallela observed good stability after mandibular advancement and fixation with polylactide biodegradable screws.25 Enislidis successfully used new biodegradable copolymer osteosynthesis system for fixation of zygomatic fractures26, 27 as absorbable mesh plates for orbital floor28 and craniosynostosis29 due to its easy shaping and application. Turvey used self-reinforced biodegradable bone plates and screws in orthognathic surgery.30, 31 Self-reinforced poly(l-/dl-)lactic acid copolymer does not require heating before adaptation to bony contours. Even high load-bearing areas, such as the human mandible, can be treated with biodegradable devices under certain circumstances due to their new biomechanical properties. Ylikontiola successfully used them for fixation of anterior mandibular fractures.32
Ricalde studied the effect of heating on bioresorbable plates.33 Ferretti34 conducted a prospective trial of poly-l-lactic/PGA copolymer plates and screws for internal fixation of mandibular fractures in 29 patients and observed a 22.5% complication rate, range 13.7–43%. He concluded that PLLA/PGA copolymer plate and screw fixation of mandibular fractures, although technically more challenging and costly, is a viable alternative to traditional metal devices. Yang et al.35 treated 10 patients (6 men, 4 women) with isolated displaced mandibular angle fracture using single or dual resorbable plates. They found resorbable plates suitable for the fixation of isolated mandibular angle fractures. Recently, An et al.36 fixed pediatric mandibular 42 fractures and concluded that the biodegradable fixation devices were safe and efficient. Although osteolysis follows biodegradable fixation of pediatric mandibular fractures, it has no adverse effect on fracture healing.
At present, the most important problem with resorbable plating systems is their high cost. However, their advantages, such as low infection rates and minimization of the need for secondary operations, make them an attractive option. With newer and cost-effective systems, we believe that they will be preferred more frequently among other options.
5. Conclusion
Based on our study, we conclude that the bioresorbable plate system provides reliable stability for osteosynthesis of mandibular fractures without major complications. Case selection is the key and it should only be used as a load-sharing plate in a semirigid technique after anatomic reduction. However, a long-term follow-up and more cases are needed to confirm these results.
Conflicts of interest
The authors have none to declare.
References
- 1.Champy M., Loddé J.H., Must D., Jaeger J.H., Muster D. Mandibular osteosynthesis by miniature screwed plates via buccal approach. J Maxillofac Surg. 1978;6:14–21. doi: 10.1016/s0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 2.Rowe N.L. J Oral Surg. 1968;26:505–507. [PubMed] [Google Scholar]
- 3.McCoy F.J., Chandler R.A., Crow M.L. Plast Reconstr Surg. 1966;37:209–312. doi: 10.1097/00006534-196603000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Krueger E. Fractures of the facial bones in children. In: Krueger E., Schilli W., editors. Vol. 2. Quintessence; Chicago: 1986. pp. 259–292. (Oral Maxillofac Trauma). [Google Scholar]
- 5.Singh R.K., Chand S., Pal U.S., Das Sanjib K., Sinha V.P. Matrix miniplate versus locking miniplate in the management of displaced mandibular angle fractures. Natl J Maxillofac Surg. 2013;4:22–25. doi: 10.4103/0975-5950.127656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar V., Mehrotra D., Mohammad S. Anchor lag screw vs conventional lag screw in mandibular fractures: a series of 30 cases. J Oral Biol Craniofac Res. 2013;3(1):15–19. doi: 10.1016/j.jobcr.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bessho K., Iizuka T., Murakami K. A bioabsorbable poly-l-lactide miniplate and screw system for osteosynthesis in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1997;55(9):941–945. doi: 10.1016/s0278-2391(97)90065-3. [DOI] [PubMed] [Google Scholar]
- 8.Wall G., Dahlberg G., Rosenquist B. Postoperative migration of the osteotomy segment stabilized by titanium miniplate osteosynthesis following Le Fort I osteotomy: an X-ray stereometric study. Int J Adult Orthodon Orthognath Surg. 1998;13(2):119–129. [PubMed] [Google Scholar]
- 9.Bessho K., Fuiimura K., Iizuka T. Experimental long-term study of titanium ions eluted from pure titanium miniplates. J Biomed Mater Res. 1995;29(7):901–904. doi: 10.1002/jbm.820290716. [DOI] [PubMed] [Google Scholar]
- 10.Islamoglu K., Coskunfirat O.K., Tetik G., Ozgentas H.E. Complications and removal rates of miniplates and screws used for maxillofacial fractures. Ann Plast Surg. 2002;48(3):265–268. doi: 10.1097/00000637-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Kennady M.C., Tucker M.R., Lester G.E., Buckley M.J. Stress shielding effect of rigid internal fixation plates on mandibular bone grafts. A photon absorption densitometry and quantitative computerized tomographic evaluation. Int J Oral Maxillofac Surg. 1989;18(5):307–310. doi: 10.1016/s0901-5027(89)80101-8. [DOI] [PubMed] [Google Scholar]
- 12.Fiala T.G., Novelline R.A., Yaremchuk M.J. Comparison of CT imaging artifacts from craniomaxillofacial internal fixation devices. Plast Reconstr Surg. 1993;92(7):1227–1232. [PubMed] [Google Scholar]
- 13.Wiltfang J., Merten H.A., Schultze-Mosgau S., Schrell U., Wenzel D., Kessler P. Biodegradable miniplates (LactoSorb): long-term results in infant minipigs and clinical results. J Craniofac Surg. 2000;11(3):239–243. doi: 10.1097/00001665-200011030-00006. [DOI] [PubMed] [Google Scholar]
- 14.Yerit K.C., Haninich S., Enislidis G. Biodegradable fixation of mandibular fractures in children: stability and early results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):17–24. doi: 10.1016/j.tripleo.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Suuronen R., Pohjonen T., Vasenius J., Vainionpaa S. Comparison of absorbable self-reinforced multilayer poly-l-lactide and metallic plates for the fixation of mandibular body osteotomies: an experimental study in sheep. J Oral Maxillofac Surg. 1992;50(3):255–262. doi: 10.1016/0278-2391(92)90322-q. [DOI] [PubMed] [Google Scholar]
- 16.Cohen S.R., Holmes R.E., Amis P., Fitchner H., Shusterman E.M. Tacks: a new technique for craniofacial fixation. J Craniofac Surg. 2001;12:596–602. doi: 10.1097/00001665-200111000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt B.L., Perrott D.H., Mahan D., Kearns G. The removal of plates and screws after Lefort I osteotomy. J Oral Maxillofac Surg. 1998;56:184–188. doi: 10.1016/s0278-2391(98)90865-5. [DOI] [PubMed] [Google Scholar]
- 18.Nagase D.Y., Courtemanche D.J., Peters D.A. Plate removal in traumatic facial fractures: 13-year practice review. Ann Plast Surg. 2005;55(6):608–611. doi: 10.1097/01.sap.0000189666.13860.c0. [DOI] [PubMed] [Google Scholar]
- 19.Francel T.J., Brent C.B., Ringleman P.R., Manson P.N. The fate of plates and screws after facial fracture reconstruction. Plast Reconstr Surg. 1992;90(4):568–573. doi: 10.1097/00006534-199210000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Kulkarni R.K., Pani K.C., Neumann C., Leonard F. Polylactic acid for surgical implants. Arch Surg. 1966;93(5):839–843. doi: 10.1001/archsurg.1966.01330050143023. [DOI] [PubMed] [Google Scholar]
- 21.Eppley B.L. Use of resorbable plates and screws in pediatric facial fractures. J Oral Maxillofac Surg. 2005;63:385–439. doi: 10.1016/j.joms.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 22.Eppley B.L., Sadove A.M., Havlik RJ: Resorbable plate fixation in pediatric craniofacial surgery. Plast Reconstr Surg. 1997;100(1):1–13. doi: 10.1097/00006534-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Mizuhashi H., Suga K., Uchiyama T., Oda Y. Changes in mechanical properties of poly-l-lactic acid mini-plates under functional loading simulating sagittal split ramus osteotomy. Int J Oral Maxillofac Surg. 2008;37:162–169. doi: 10.1016/j.ijom.2007.09.178. [DOI] [PubMed] [Google Scholar]
- 24.Vaananen P., Nurmi J.T., Nuutinen J.P., Jakonen S., Happonen S., Jank S. Fixation properties of a biodegradable “free form” osteosynthesis plate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:477–482. doi: 10.1016/j.tripleo.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Kallela I., Laine P., Suuronen R., Iizuka T., Pirinen S., Lindqvist C. Skeletal stability following mandibular advancement and rigid fixation with polylactide biodegradable screws. Int J Oral Maxillofac Surg. 1998;27:3–8. doi: 10.1016/s0901-5027(98)80086-6. [DOI] [PubMed] [Google Scholar]
- 26.Enislidis G., Pichorner S., Lambert F. Fixation of zygomatic fractures with a new biodegradable copolymer osteosynthesis system. Preliminary results. Int J Oral Maxillofac Surg. 1998;27:352–355. doi: 10.1016/s0901-5027(98)80063-5. [DOI] [PubMed] [Google Scholar]
- 27.Enislidis G., Yerit K., Wer G., Hnke R.K., Schragl S., Ewers R. Self-reinforced biodegradable plates and screws for fixation of zygomatic fractures. J Cranio-Maxillofac Surg. 2005;33:95–102. doi: 10.1016/j.jcms.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 28.Hollier L.H., Rogers N., Berzin E., Stal S. Resorbable mesh in the treatment of orbital floor fractures. J Craniofac Surg. 2001;12(3):242–246. doi: 10.1097/00001665-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Surpure S.J., Smith K.S., Sullivan S.M., Francel P.C. The use of a resorbable plating system for treatment of craniosynostosis. J Oral Maxillofac Surg. 2000;59:1271–1275. doi: 10.1053/joms.2001.27497. [DOI] [PubMed] [Google Scholar]
- 30.Turvey T.A., Bell R.B., Tejera T.J., Proffit W.R. The use of self reinforced biodegradable bone plates and screws in orthognathic surgery. J Oral Maxillofac Surg. 2002;60:59–65. doi: 10.1053/joms.2002.28274. [DOI] [PubMed] [Google Scholar]
- 31.Eppley B.L., Sadove A.M. Effects of resorbable fixation on craniofacial skeletal growth: modifications in plate size. J Craniofac Surg. 1994;5(2):110–114. doi: 10.1097/00001665-199405000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Ylikontiola L., Sundqvuist K., Sandor G.K., Törmälä P., Ashammakhi N. Self-reinforced bioresorbable poly-l/dl-lactide [SRP(L/DL)LA] 70/30 miniplates and miniscrews are reliable for fixation of anterior mandibular fractures: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(31):2–7. doi: 10.1016/j.tripleo.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 33.Ricalde P., Caccamese J., Norby C., Posnick J.C., Hartman M.J., von Fraunhofer J.A. Strength analysis of 6 resorbable implant systems does heating affect the stress strain curve. J Oral Maxillofac Surg. 2009;66:2493–2497. doi: 10.1016/j.joms.2008.06.096. [DOI] [PubMed] [Google Scholar]
- 34.Ferretti C. A prospective trial of poly-l-lactic/polyglycolic acid co-polymer plates and screws for internal fixation of mandibular fractures. Int J Oral Maxillofac Surg. 2008;37:242–248. doi: 10.1016/j.ijom.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 35.Yang R.T., Lv K., Zhou H.H., Li Z., Li Z.B. Resorbable plates for the fixation of isolated mandibular angle fracture. J Craniofac Surg. 2015;26(2):447–448. doi: 10.1097/SCS.0000000000001349. [DOI] [PubMed] [Google Scholar]
- 36.An J., Jia P., Zhang Y., Gong X., Han X., He Y. Application of biodegradable plates for treating pediatric mandibular fractures. J Cranio-Maxillofac Surg. 2015;43(4):515–520. doi: 10.1016/j.jcms.2015.03.002. [DOI] [PubMed] [Google Scholar]