Sir,
We present the case of an 8-year-old child in Ethiopia with a large coronary artery fistula connecting the left anterior descending artery to the right ventricle, who was treated by a combined surgical and percutaneous approach.
First described in 1865,[1] coronary artery fistulae connect the coronary vessel to a chamber of the heart, the pulmonary artery, or the coronary sinus. Coronary artery fistulae are relatively rare, representing 0.2–0.4% of all congenital heart defects[2] and can be asymptomatic and close spontaneously, or they can manifest as myocardial ischemia, arrhythmia, or heart failure. In the case of large and/or symptomatic fistulae, surgical closure is indicated; however, in young patients, large uncorrected fistulae can be difficult to visualize. The majority of fistulae can be closed using percutaneous procedures; although, invasive surgery is sometimes required to achieve full closure.
An 8-year-old child was admitted to a cardiology center with biventricular heart failure. Echocardiography revealed a fistula from the left anterior descending coronary artery opening into the right ventricle through three outlets [Figure 1]. The right cardiac chambers were severely dilated.
Figure 1.
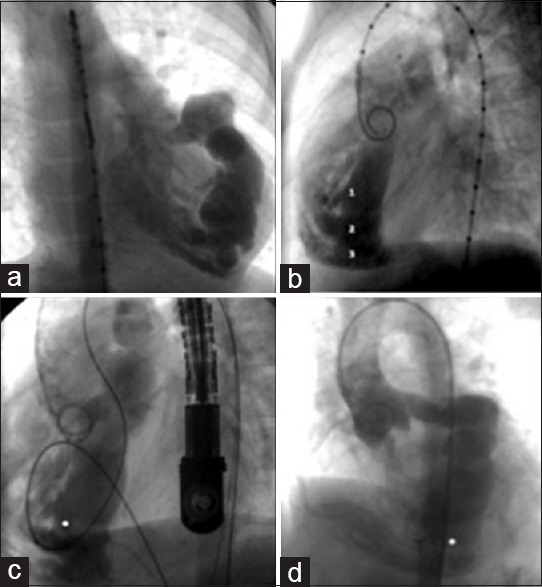
Catheter intervention. (a and b) Aortogram 39° showing a grossly dilated left anterior descending coronary artery. Large communication is visible between the coronary artery and the right ventricle via three orifices (labeled 1, 2, and 3 in panel B). (c) Aortogram, lateral projection. A balloon (the white dot) was used to estimate the size of the orifice. The transesophageal echocardiogram probe is visible at the right. (d) Aortogram, left anterior oblique projection. The white dot indicates the ADO device that was placed in the lower orifice
In November 2010, catheterization and coronary angiography were performed, revealing significant dilation of the left anterior descending artery and a large fistula from the middle third of the artery, with three large orifices emptying into the right ventricular chamber.
Percutaneous closure is the current treatment of choice for coronary artery fistulae and the medical team elected to initially place a patent ductus arteriosus closure device (Amplatzer duct occluder, [ADO]) into the largest orifice. Using angiography, the team located the three fistulous orifices that emptied into the right ventricle through the middle and lower third of the interventricular septum; the largest orifice was 4–6 mm wide. Following the creation of an arteriovenous loop, a size 10/8-mm ADO occlusion device was inserted transvenously using a 7F long sheath catheter; the placement and stability of the device were confirmed using transesophageal echocardiography [Figure 2].
Figure 2.
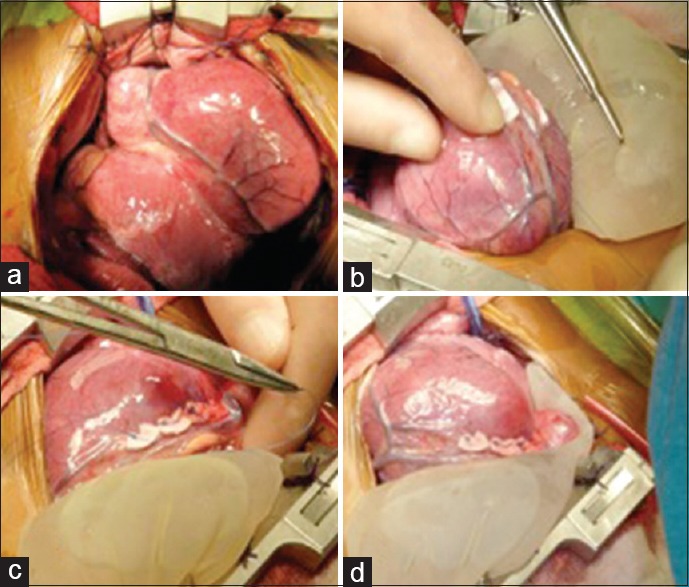
The surgical intervention. (a) The left pericardium was retracted using several sutures. (b) The area surrounding the left anterior descending artery was stabilized using a surgical glove filled with sterile serum placed under the heart. (c) Using data obtained from the transesophageal echocardiograph, the orifices were located. The cardiologist guided the surgeon, who then began to suture below the left anterior descending artery. The sutures were backed with Teflon patches. (d) The procedure was completed after six sutures were placed under the artery
After the placement of this first device, the child was discharged under medical treatment. Three years later, the patient's New York Heart Association (NYHA) cardiac functional Class was II–III. Following a risk-benefit analysis, the team elected to attempt surgical closure of the remaining orifices. The closure was performed without cardiopulmonary bypass and was guided by transesophageal echocardiography, with sutures placed below the left anterior descending artery to close the fistulous trajectories [Video 1].
The patient showed clear clinical improvement and was discharged 10 days after surgery. In a follow-up assessment 3 years after surgical closure, the patient's NYHA functional class improved to Class I, and echocardiography showed only a small residual fistula.
In summary, we report the treatment of a coronary artery fistula in an 8-year-old child in Ethiopia using a two-step approach. In many patients, coronary artery fistulae can be treated using either a percutaneous or invasive surgical approach. In clinical settings in which the appropriate technology is not available, a combination of both treatments can be vital for achieving successful treatment.
Video Available on: www.annalspc.com
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Krause W. Ueber den Ursprung einer accessorischen A. coronaria cordis aus der A. pulmonalis. Z Rat Med. 1865;24:225–9. [Google Scholar]
- 2.Urrutia SC, Falaschi G, Ott DA, Cooley DA. Surgical management of 56 patients with congenital coronary artery fistulas. Ann Thorac Surg. 1983;35:300–7. doi: 10.1016/s0003-4975(10)61563-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


