Abstract
Context:
Primary care practice.
Objective:
To test whether the principles of complex adaptive systems are applicable to implementation of team-based primary care.
Design:
We used complex adaptive system principles to implement team-based care in a private, five-clinic primary care practice. We compared randomly selected samples of patients with coronary heart disease (CHD) and diabetes before system implementation (March 1, 2009, to February 28, 2010) and after system implementation (December 1, 2011, to March 31, 2013).
Main Outcome Measures:
Rates of patients meeting the composite goals for CHD (blood pressure < 140/90 mmHg, low-density lipoprotein cholesterol level < 100 mg/dL, tobacco-free, and using aspirin unless contraindicated) and diabetes (CHD goal plus hemoglobin A1c concentration < 8%) before and after the intervention. We also measured provider and patient satisfaction with preventive services.
Results:
The proportion of patients with CHD who met the composite goal increased from 40.3% to 59.9% (p < 0.0001) because documented aspirin use increased (65.2%–97.5%, p < 0.0001) and attainment of the cholesterol goal increased (77.0%–83.9%, p = 0.0041). The proportion of diabetic patients meeting the composite goal rose from 24.5% to 45.4% (p < 0.0001) because aspirin use increased (58.6%–97.6%, p < 0.0001). Increased percentages of patients meeting the CHD and diabetes composite goals were not significantly different (p = 0.2319). Provider satisfaction with preventive services delivery increased significantly (p = 0.0017). Patient satisfaction improved but not significantly.
Conclusion:
Principles of complex adaptive systems can be used to implement team-based care systems for patients with CHD and possibly diabetic patients.
INTRODUCTION
Despite the burden that cardiovascular diseases place on Americans1 and clear evidence that team-based health care improves control of cardiovascular risk factors,2–10 many medical practices have not adopted this innovation. A classic trial to reduce cardiac surgical mortality provides clues about the components that make practice improvement interventions successful. Nearly 20 years ago the Northern New England Cardiovascular Disease Study Group showed that surgical outcomes could be improved with a simple 3-component intervention: feedback of outcome data, training in continuous quality improvement techniques, and site visits to other Medical Centers.11 Even though the surgeons were not provided with detailed process improvement instructions, the intervention was associated with a 24% reduction in in-hospital mortality.11 The authors suggested that, along with the 3 prongs of the intervention, giving each care team the autonomy to change their operations as they saw fit led to the rapid decline in mortality.
In his appendix to Crossing the Quality Chasm,12 Plsek13 suggests that, rather than using the principles of mechanical systems to try to improve health care, innovators should employ the principles of complex adaptive systems. The behavior of mechanical systems (eg, automobiles) can always be predicted if the system is described in adequate detail. The same is not true for complex adaptive systems like human social interaction because people are autonomous. Although the behavior of complex adaptive systems cannot be predicted using the rules that apply to mechanical systems, simple rules can suffice. For example, the behavior of flocks of birds, schools of fish, and herds of mammals can be explained with just three rules: avoid collisions, attempt to match velocity, and attempt to stay close to the nearest neighbor.14
Kottke and colleagues15 have hypothesized that only five conditions need to be met to create value in health care. These conditions are: 1) the stakeholders agree on a set of mutual, measurable goals for the health system; 2) the extent to which the goals are being achieved is reported to the public; 3) resources are available to achieve the goals; 4) stakeholder incentives, imperatives, and sanctions are aligned with the agreed-on health system goals; and 5) leaders among all stakeholders endorse and promote the agreed-on health system goals. When these conditions are met, the stakeholders will organize themselves to perform. This observation is consistent with the reported experience of the Northern New England Cardiovascular Disease Study Group.11
The goal we set was to test whether a group practice that comprises 5 privately owned primary care clinics would implement systems of team-based care if we used the principles of complex adaptive systems to design the intervention. We defined success as the satisfaction of 3 objectives. The first objective was that, relative to patients with Type 2 diabetes mellitus, the care system would increase the proportion of patients with coronary heart disease (CHD) who satisfy a composite measure (blood pressure < 140/90 mmHg, low-density lipoprotein [LDL] cholesterol level < 100 mg/dL, no use of tobacco, and taking at least 81 mg/day of aspirin unless contraindicated). The second objective was that the system would be associated with increased satisfaction among both patients and staff. The third objective was that the financial impact of the system would be positive or neutral for the practice. We also collected qualitative data from providers during the implementation period so that we could better understand the process that the clinics experienced as they implemented their systems.
In this article, we report the results of the first two objectives. Regarding the third objective, we were unable to generate a revenue stream that offset the cost of the team-based care system. We are in the process of preparing a detailed report. Finally, the results of the qualitative analysis demonstrate that the task of implementing team-based care is complex. Among other tasks, roles must be defined and individuals must learn how to work in teams; patient registry and clinical data retrieval technology must be developed and implemented; and care processes for previsit planning and between-visit care management must be defined and implemented. Success requires an ongoing effort of creation, revision, retraining, and reinforcement.16
METHODS
The HealthPartners Institute for Education and Research institutional review board approved the study as Protocol 09-132.
Clinical Setting
We conducted the study in a for-profit primary care practice of 46 primary care physicians and advanced care providers who care for small town and rural patients as well as a commuter population in western Wisconsin. The practice is made up of 5 clinics in 3 divisions (1 division has a main practice site and 2 satellite clinics). Each division has its own administrator and Clinical Services Manager. Physicians own and govern the practice. Clinic assistants, primarily certified medical assistants, support the providers during patient visits to increase work flow efficiency. A few months before we began our trial, the practice created a new position of care coordinator in all its divisions to coordinate the care of patients who might benefit from follow-up services. The practice also implemented an electronic medical record system at about the same time. The clinics had already used continuous quality improvement methods to innovate, and in 2013, all 3 divisions achieved National Committee for Quality Assurance Medical Home accreditation.
Patient Management System
We took three concepts into account when we designed the implementation process: 1) health services delivery systems are complex adaptive systems, not mechanical systems13; 2) adoption of any system of care requires adaptation and reinvention17–19; and 3) the long-term survival of any system of care requires that a new process, at a minimum, does not threaten the viability of the overall system. We accepted the long-term financial success of the practice in a highly competitive market as prima facie evidence that the physicians in the group knew the fundamentals of designing care delivery systems; they did not need guidance at that level.
Therefore, rather than provide the clinics with an operational structure that we expected them to implement in parallel with their other care processes, our only firm requests were that they use the study resources to improve their Minnesota HealthScores vascular disease quality scores20 and hire a registered nurse (RN) Care Manager to coordinate the team-care program. Although we paid her salary with grant resources, the RN Care Manager was a clinic employee who reported to one of the Clinical Services Managers and a lead primary care physician; she did not report to the investigators. Otherwise, the clinics could use or modify existing care processes to the extent they wished but could also develop new processes as they believed necessary. Although each of the five clinics shared information and worked to develop common treatment goals, they were free to implement the processes that best fit their existing procedures.
The clinics used the concepts of the medical home21 and the chronic care model22 to develop their patient care systems. The systems’ personnel were composed of the RN Care Manager, information technology staff, and clinic assistant care coordinators. These care coordinators supported providers in the following tasks: developing treatment protocols and processes; verifying the accuracy of patient data; reviewing the lists of patients who were not at goal with the responsible provider; and developing and carrying out care and follow-up plans. The RN Care Manager rotated to a different clinic every month, but care coordinators and providers from all five clinics could contact her by phone and e-mail during the trial. The RN Care Manager also helped the care coordinators refine patient education and counseling techniques, identified resources for patients (eg, smoking cessation options), addressed barriers to care that the patients were facing (eg, transportation, paying for medications), and helped refine and revise clinic systems (eg, previsit planning, after-visit care, between-visit follow-up, and team communications).
For some tasks, the system development teams were able to use existing clinic care and information technology systems; for other tasks, however, they needed to develop new protocols, processes, and capabilities. For example, they needed to develop protocols for hypertension, lipid management, and tobacco use cessation. The clinics also needed to develop previsit planning and postvisit follow-up protocols. All protocols needed to be approved by clinic leaders.
All patients were assigned to provider panels. This allowed the staff to generate quarterly provider-specific lists of patient names and risk factor levels that could be reviewed with each provider to develop treatment and follow-up plans. These plans were then implemented by the care coordinators and the RN Care Manager.
Evaluation Design
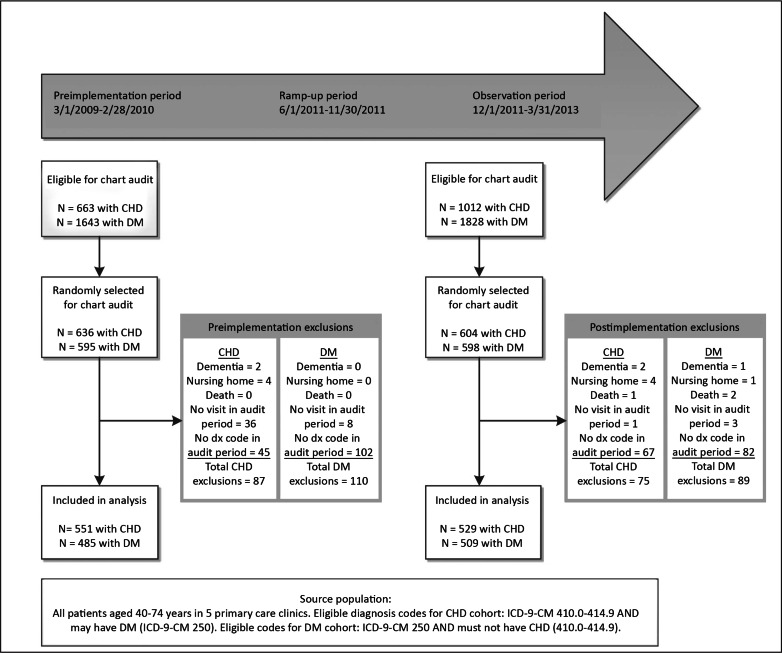
We tested the hypothesis that the patient management system would increase the proportion of patients who met goals for controlling their risk factors. To do so, we reviewed the medical records of independent random samples of patients who received care in the 12 months before the system was implemented and during the 12-month period that started 6 months after each clinic implemented its care system (Figure 1). We excluded the first 6 months of the implementation period from the evaluation because we considered it an early learning period. We compared the differences in the 2 samples of patients with CHD with 2 randomly selected samples of diabetic patients who were treated during the same periods. We selected patients with diabetes as the reference group because, with the exception of hemoglobin A1c concentration, their chronic care management goals are identical. Patients who had both CHD and diabetes were included in our sample of patients with CHD. To ensure that a primary care provider had an opportunity to take corrective action if a patient was not at goal, we required that patients in all 4 samples have 2 or more primary care visits during each evaluation period.
Figure 1.
Trial evaluation design.a
a Dates are presented as month/day/year.
CHD = coronary heart disease; DM = diabetes mellitus; dx = diagnosis; ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
The preimplementation evaluation period was March 1, 2009, to February 28, 2010. Applying prespecified exclusion rules to the 1231 patients identified for the preimplementation sample, we excluded 2 patients because they had a diagnosis of dementia (International Classification of Diseases, Ninth Revision Clinical Modification Codes 290-294), we excluded 4 patients because they resided in a nursing home, we excluded 44 patients because they did not have 2 or more primary care visits in the preimplementation period, and we excluded 145 patients because they did not have CHD or diabetes diagnosis codes. The final preimplementation CHD sample comprised 551 patients, and the final preimplementation diabetes sample comprised 485 patients.
The postimplementation evaluation period was December 1, 2011, to March 31, 2013. The postimplementation period was greater than 1 year because implementation was staggered in the 5 clinics. Applying prespecified exclusion rules to the 1202 patients identified for the postimplementation sample, we excluded 3 patients because of a diagnosis of dementia, 3 patients because they died during the observation period, 5 patients because they resided in a nursing home, 4 patients because they did not have 2 or more primary care visits in the postimplementation period, and 149 because they did not have CHD or diabetes diagnosis codes. The final postimplementation CHD sample comprised 529 patients, and the final postimplementation diabetes sample comprised 509 patients.
Surveys
Providers
To test whether the new system would improve provider satisfaction with the delivery of preventive services, we invited all primary care providers and administrative staff who provided primary care services to complete a survey before implementation. After system implementation, we invited the individuals who had completed the preimplementation survey to complete it again.
Patients
We invited community-living patients who were age 40 years or older, treated by the practice for CHD, and without terminal illness to complete a survey about the care they received and their satisfaction with their clinic. We adapted the survey instrument from a patient satisfaction survey we used in a previous trial.23
We mailed surveys to randomly selected patients with CHD, whom we identified via the clinics’ patient management system, if they met study inclusion criteria and had been seen at least once in primary care during an 18-month preintervention period. An attempt was made to contact patients by telephone if they did not respond to the mailing.
The patients who participated in the preintervention survey were invited to participate in the postintervention survey. The postintervention survey instrument and protocol were the same as those for the preintervention survey.
Clinical Performance Data Sources
We used risk factor data that had been collected as part of routine patient care to evaluate the main trial outcomes. Two trained nurses abstracted the data from the patients’ medical records. Because the clinics had not yet instituted an electronic medical record system at the beginning of the study, the nurses abstracted the preintervention data from paper charts. The clinics implemented an electronic medical record system (Cerner Corp, North Kansas City, MO) in May 2010; thus, we collected postimplementation data from electronic records.
We defined the primary outcomes for patients with CHD and patients with diabetes according to the goals of the Minnesota Community Measurement.20 Patients with CHD had to meet a composite measure comprising the following criteria to be considered at goal: systolic blood pressure under 140 mmHg and diastolic blood pressure below 90 mmHg, LDL cholesterol less than 100 mg/dL, no tobacco use, and taking aspirin unless contraindicated. Patients with diabetes had to meet a composite measure comprising the same criteria plus have a hemoglobin A1c level less than 8%.
To document the reliability of the data extraction process from the electronic records, the 2 nurse abstractors extracted the same data from the records of 50 patients. Kappa statistics for the comparison between the electronically extracted data and the data extracted by the nurses were as follows for systolic blood pressure, diastolic blood pressure, LDL cholesterol, tobacco use, and hemoglobin A1c, respectively: 0.82, 0.82, 0.86, 0.81, and 0.91. Kappa statistics for interrater reliability between the 2 chart auditors were 0.86, 1.00, 0.89, 0.82, and 0.87 for the same 5 data elements, respectively.
Statistical Analysis
We used statistical analysis software (SAS Version 9.3, SAS Institute, Cary NC) to generate all descriptive statistics (means, standard deviations, and proportions) and multivariable analyses. To compare differences between periods and subgroups, we used the Student t-test for continuous data and the χ2 test for categorical data. We used a difference-in-differences analysis to compare differences in blood pressure and LDL cholesterol between the CHD and diabetic pre- and postimplementation samples.
We employed a series of mixed model logistic regressions to compute predicted probabilities of binary outcomes (whether or not at goal for each component of the composite measure) and ordinal outcomes (the composite care score). We used an interaction term for time and condition (CHD, diabetes) to test our hypothesis that the increase in the proportion of patients satisfying the CHD composite measure would be greater than the increase in the proportion of patients satisfying the composite diabetes measure.
For our analysis of the provider survey, we compared individual item responses before and after implementation. For our analysis of the patient survey data, we also compared preimplementation responses with postimplementation responses.
RESULTS
Risk Factor Changes
We identified 23 components that the clinics developed as they implemented their care management systems (see Sidebar: Activities Undertaken by Participating Clinics to Implement Ischemic Vascular Disease Management Systems). Nine were directly related to the delivery of patient care; 5 were related to training and supporting providers and staff; 6 were related to staff education and training and tool development; and 3 were related to information technology needs.
Activities Undertaken by Participating Clinics to Implement Ischemic Vascular Disease Management Systems.
Related to patient care delivery
Develop and/or revise a previsit planning form
Adopt hypertension, hyperlipidemia, and tobacco treatment protocols
Create a rapid medication titration protocol
Develop protocols for proactive between-visit contacts with patients
Create a care coordinator’s patient summary tool that includes treatment goals, medication and medical history, and record of communications with the patient
Create protocols for care coordinator’s team communications regarding blood pressure rechecks and referral to registered nurse Care Manager
Develop an ischemic vascular disease (IVD) report card for patients
Conduct a monthly meeting with a consulting cardiologist to review care plans
Create protocols to provide drug samples, referrals to the free clinic, transportation services, etc
Related to providers and staff
Provide comparison of attainment of IVD goal before and after program implementation
Provide repeated comparisons of diabetes mellitus and IVD goal achievement
Provide monthly, unblinded IVD report cards for all providers
Periodically report project updates to clinic services staff
Review reports and care plans with physicians and clinic services staff at team meetings
Related to staff education and training, and tool development
Develop a frequently asked questions document that answers questions about IVD and addresses the goals, coding, and similar care improvement project topics
Train clinical services staff to use the previsit planning tool, registry, and patient education materials
Conduct training for tobacco use cessation intervention
Provide in-service training for the clinic services staff regarding pathophysiology of IVD and risk factors
Develop tip sheets and quizzes for use by clinical services staff
Develop patient education materials, door posters, tobacco use cessation folders, and similar products
Related to information technology
Create an IVD registry
Update the registry twice weekly
Modify and maintain the electronic health record to ensure data accuracy regarding patient status, provider attribution, aspirin documentation, blood pressure recording, and diagnostic coding
On average, patients in the CHD samples were older than patients in the diabetes samples, and the ratio of men to women was greater in the CHD sample than in the diabetes samples. (Table 1). More than 96% of the patients in each of the samples were white. Although the diagnosis of hypertension was equally prevalent for the patients with CHD and the patients with diabetes, the diagnosis of hyperlipidemia was more prevalent among the patients with CHD. On average, the patients with CHD had more primary care visits and more visits to other services than did the patients with diabetes.
Table 1.
Demographic characteristics and visit frequency of independent samples of patients with coronary heart disease and diabetes before and after implementation of care systems
| Characteristic | Coronary heart disease | Diabetes | CHD vs DM p value | ||||
|---|---|---|---|---|---|---|---|
| Pre (n = 511) | Post (n = 529) | Pre vs post p value | Pre (n = 485) | Post (n = 509) | Pre vs post p value | ||
| Age, years, mean (SD) | 63.6 (7.6) | 64.2 (7.7) | 0.2033 | 59.6 (8.6) | 60.0 (8.7) | 0.4268 | < 0.0001 |
| Age category, % | |||||||
| 40–49 years | 6.2 | 6.4 | 0.2857 | 14.6 | 14.7 | 0.8496 | < 0.0001 |
| 50–59 years | 24.7 | 19.9 | 35.2 | 34.2 | |||
| 60–69 years | 45.8 | 48.2 | 36.9 | 36 | |||
| 70–75 years | 23.3 | 25.5 | 13.2 | 15.1 | |||
| Sex, % | |||||||
| Men | 75.7 | 74.3 | 0.6471 | 52.0 | 52.3 | 0.9245 | < 0.0001 |
| Women | 24.3 | 25.7 | 48.0 | 47.7 | |||
| Medical history, % | |||||||
| Hypertension | 76.0 | 77.3 | 0.6212 | 75.7 | 75.0 | 0.9364 | 0.4835 |
| Dyslipidemia | 82.9 | 87.2 | 0.0530 | 74.0 | 83.7 | 0.0002 | 0.0003 |
| Visit frequency, mean (SD) | |||||||
| Any primary care visit during observation period | 8.5 (6.1) | 7.6 (4.6) | 0.0546 | 7.9 (5.3) | 7.2 (4.6) | 0.3228 | 0.0009 |
| Any visit to other services during observation period | 0.6 (2.6) | 0.3 (1.4) | 0.2607 | 0.5 (1.8) | 0.3 (2.6) | 0.6608 | 0.0118 |
CHD = coronary heart disease; DM = diabetes mellitus; post = postimplementation; pre = preimplementation; SD = standard deviation.
The only significant difference in biometric characteristics between the preimplementation and postimplementation CHD samples was a mean LDL cholesterol level that was nearly 7 mg/dL lower in the postimplementation sample (Table 2). Diastolic blood pressure was the only significantly different biometric parameter between the 2 samples of patients with diabetes. There were no significant biometric differences in differences among the 4 samples.
Table 2.
Biometric characteristics of independent samples of patients with coronary heart disease and diabetes before and after implementation of care systems
| Characteristic | Coronary heart disease | Diabetes | p value: change in CHD vs change in DM | ||||
|---|---|---|---|---|---|---|---|
| Pre (n = 511) | Post (n = 529) | p value | Pre (n = 485) | Post (n = 509) | p value | ||
| Systolic blood pressure (mmHg), mean (SD) | 122.8 (13.8) | 124.1 (13.4) | 0.1658 | 125.5 (13.3) | 126.3 (12.8) | 0.3380 | 0.7109 |
| Diastolic blood pressure (mmHg), mean (SD) | 71.7 (8.9) | 72.5 (9.3) | 0.2526 | 73.2 (9.4) | 74.3 (8.7) | 0.0430 | 0.6094 |
| LDL cholesterol (mg/dL), mean (SD) | 87.7 (35.8) | 80.9 (28.3) | 0.0009 | 93.5 (38.9) | 91.0 (32.9) | 0.2737 | 0.1708 |
| Hemoglobin A1c, mean (SD) | NA | NA | NA | 7.0 (1.1) | 7.1 (1.4) | 0.1226 | NA |
CHD = coronary heart disease; DM = diabetes mellitus; LDL = low-density-lipoprotein; NA = not applicable; post = postimplementation; pre = preimplementation; SD = standard deviation.
The proportion of patients in the CHD postimplementation sample who met the LDL cholesterol goal was significantly higher than the proportion in the preimplementation CHD sample (Table 3). The proportion of patients who met the LDL cholesterol goal was the same for both samples of patients with diabetes. The proportions of patients who were documented to be taking aspirin unless contraindicated were significantly higher in both postimplementation samples. The proportion of patients satisfying the composite score criterion was significantly higher in the postimplementation sample of patients with CHD relative to the preimplementation sample. The same was true for the two samples of patients with diabetes. The difference in LDL before vs after implementation was the only difference between the samples of patients with CHD and the samples of patients with diabetes.
Table 3.
Percentage of patients with coronary heart disease and diabetes whose parameters were at goal before and after program implementation
| Goal parameter | Coronary heart disease | Diabetes | p value: change in CHD vs change in diabetes parameters | ||||
|---|---|---|---|---|---|---|---|
| Pre (n = 511) | Post (n = 529) | p value | Pre (n = 485) | Post (n = 509) | p value | ||
| Blood pressure | 86.6 | 86.8 | 0.9239 | 84.5 | 87.8 | 0.1342 | 0.3129 |
| LDL cholesterol | 77.0 | 83.9 | .0041 | 70.7 | 70.7 | 0.9999 | 0.0323 |
| Aspirin | 65.2 | 97.5 | < 0.0001 | 58.6 | 97.6 | < 0.0001 | 0.3427 |
| Tobacco-free | 79.7 | 81.1 | 0.5562 | 81.2 | 83.3 | 0.3945 | 0.8207 |
| Hemoglobin A1c | NA | NA | NA | 84.7 | 81.3 | 0.1536 | NA |
| Composite score criteriona | 40.3 | 59.9 | < 0.0001 | 24.5 | 45.4 | < 0.0001 | 0.2319 |
Composite score for patients with coronary heart disease comprises blood pressure under 140/90 mmHg, low-density-lipoprotein cholesterol level below 100 mg/dL, daily aspirin therapy unless contraindicated, and tobacco-free status. Composite score criterion for patients with diabetes encompasses the same 4 components plus a hemoglobin A1c concentration below 8%.
CHD = coronary heart disease; LDL = low-density-lipoprotein; NA = not applicable; post = postimplementation; pre = preimplementation.
Survey Results
Providers
Of the 290 providers who were invited to complete the preimplementation survey, 231 (79.8%) responded. We invited the 231 baseline respondents to complete the same survey after implementation, and 205 individuals (88.8%) responded.
The only difference between preimplementation and postimplementation responses was the level of satisfaction with the way preventive services were currently being provided in the respondent’s clinic. The proportion of providers who indicated that they were satisfied or very satisfied increased from 59.5% before implementation to 74.3% after implementation (p = 0.0017).
Patients
A total of 760 patients with a CHD code were randomly selected to be surveyed before implementation of the new system. Of these, 27 were found not to actually have a diagnosis of CHD; 6 were deceased; 95 returned the survey without completing it or refused to complete it when contacted by telephone; 38 were unable to complete the survey; and 139 could not be contacted or did not return the survey. Responses from 455 patients were included in the preimplementation survey analysis.
Four hundred fifty-five eligible patients were invited to take the postimplementation survey. One patient was a duplicate and 3 were ineligible patients; 19 patients refused; 4 no longer received care from the clinics; 3 were unable to complete the survey; 4 were in assisted living or nursing homes; 6 were deceased; and 98 could not be contacted. The postimplementation survey analysis comprised the responses of 320 patients.
The proportion of patients who reported that they were satisfied or very satisfied with the preventive services that they received increased from 79.6% to 92.4%, and the proportion rating the overall health care received as good, very good, or excellent increased from 96.3% to 99.0%. However, neither of these differences, nor any other pre- or postimplementation comparison, was statistically significant.
DISCUSSION
Using the principles of complex adaptive systems, we were able to help five private primary care clinic sites organize themselves to provide team-based care for their patients with CHD. Both LDL cholesterol control and aspirin documentation improved whereas patient satisfaction with their preventive services remained high and provider satisfaction with delivery of preventive services increased. However, the system did not generate sufficient revenue to offset the cost of team-based care.
These facts are evidence that the principles of complex adaptive systems can be used to implement nurse-led team-based care in a private primary care practice. As with the trial conducted by the Northern New England Cardiovascular Disease Study Group,11 the clinicians themselves were able to locally develop and apply the systems and procedures that they needed to succeed. Analyses of large numbers of efforts to diffuse innovations suggest that autonomy to adapt an intervention to fit local conditions is necessary for success.18,19
Despite the fact that the composite scores of patients with CHD were not improved relative to the improvement in composite scores of patients with diabetes, there is other evidence of success: LDL cholesterol levels were significantly lower in the postimplementation sample of patients with CHD, a difference that did not occur between the two samples of patients with diabetes. Documentation of aspirin use also increased, but it did so both among patients with CHD and among patients with diabetes. Documentation of aspirin was responsible for the significant improvement in the composite scores. It is possible that hypertension control did not improve because of a ceiling effect. Even before team-based care, blood pressure control for patients in this practice was outstanding relative to the Healthcare Effectiveness Data and Information Set’s national average and that in other medical groups.24
Our trial has several limitations. Randomizing several clinics to intervention and control groups would have been a stronger study design. However, this was not an option for us. Although there is considerable evidence that a complex adaptive system strategy will succeed in other settings, this is not assured. Migration to an electronic record system and hiring of the RN Care Manager could have confounded the results. In fact, we believe that the RN Care Manager role was crucial to the results because the nurse was the communication and organizing node in the center of physicians, clinical care coordinators, and informatics. She also had time free from patient care that allowed her to work on system development. It is notable that one of the clinics hired the RN Care Manager in a new position of Quality Nurse after funding for the trial ended.
Because the patients with diabetes were treated by the same care teams that treated the patients with CHD, we do not know whether the improvement in aspirin documentation in both groups was caused by contamination by the newly implemented patient management system or whether it was due to another cause. We also believe that most of the change in documentation of aspirin use was simply change in documentation. If we were to consider only our primary hypothesis that the increase in the proportion of patients meeting the composite measure would be greater for patients with CHD than for diabetic patients, we would need to conclude that the study failed. However, we believe that there is still much to be learned from this trial.
CONCLUSION
We believe that the organization of care systems and the improvement in care for patients with CHD documents that the principles of complex adaptive system science and diffusion of innovations can be used to implement team-based care in private primary care practices. As the Northern New England Cardiovascular Disease Study Group demonstrated almost 20 years ago, once the goals of care are agreed on and a few other conditions are met, it is not necessary to supply clinicians with detailed operational protocols and processes. When the conditions are met, clinicians themselves have the skills, training, and professionalism that are required to implement systems that ensure high-quality care for patients who have chronic conditions.
Acknowledgments
National Heart and Lung Institute (National Institutes of Health, Bethesda, MD) grant #R18HL096563 was the sole financial support for this project.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
The Root of Life
The heart is the root of life and causes the versatility of the spiritual faculties. The heart influences the face and fills the pulse with blood.
— The Yellow Emperor’s Classic of Internal Medicine, Bk 3 Sect 9, Huangdi, c 2704 BC-2598 BC, known as the Yellow Emperor, a legendary Chinese sovereign and culture hero
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013 Jan 1;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. DOI: http://dx.doi.org/10.1161/CIR.0b013e31828124ad. Erratum in: Circulation 2013 Jun 11; 127(23):e841. DOI: http://dx.doi.org/10.1161/CIR.0b013e31829ae08c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Becker DM, Raqueño JV, Yook RM, et al. Nurse-mediated cholesterol management compared with enhanced primary care in siblings of individuals with premature coronary disease. Arch Intern Med. 1998 Jul 27;158(14):1533–9. doi: 10.1001/archinte.158.14.1533. DOI: http://dx.doi.org/10.1001/archinte.158.14.1533. [DOI] [PubMed] [Google Scholar]
- 3.Vale MJ, Jelinek MV, Best JD, Santamaria JD. Coaching patients with coronary heart disease to achieve the target cholesterol: a method to bridge the gap between evidence-based medicine and the “real world”—randomized controlled trial. J Clin Epidemiol. 2002 Mar;55(3):245–52. doi: 10.1016/s0895-4356(01)00460-7. DOI: http://dx.doi.org/10.1016/S0895-4356(01)00460-7. [DOI] [PubMed] [Google Scholar]
- 4.Miller NH, Warren D, Myers D. Home-based cardiac rehabilitation and lifestyle modification: the MULTIFIT model. J Cardiovasc Nurs. 1996 Oct;11(1):76–87. doi: 10.1097/00005082-199610000-00009. DOI: http://dx.doi.org/10.1097/00005082-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Artinian NT, Flack JM, Nordstrom CK, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007 Sep-Oct;56(5):312–22. doi: 10.1097/01.NNR.0000289501.45284.6e. DOI: http://dx.doi.org/10.1097/01.NNR.0000289501.45284.6e. [DOI] [PubMed] [Google Scholar]
- 6.DeBusk RF, Miller NH, Superko HR, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994 May 1;120(9):721–9. doi: 10.7326/0003-4819-120-9-199405010-00001. DOI: http://dx.doi.org/10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- 7.Shaw RJ, McDuffie JR, Hendrix CC, et al. Effects of nurse-managed protocols in the outpatient management of adults with chronic conditions: a systematic review and meta-analysis. Ann Intern Med. 2014 Jul 15;161(2):113–21. doi: 10.7326/M13-2567. DOI: http://dx.doi.org/10.7326/M13-2567. [DOI] [PubMed] [Google Scholar]
- 8.Wood DA, Kotseva K, Connolly S, et al. EUROACTION Study Group Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008 Jun 14;371(9629):1999–2012. doi: 10.1016/S0140-6736(08)60868-5. DOI: http://dx.doi.org/10.1016/S0140-6736(08)60868-5. [DOI] [PubMed] [Google Scholar]
- 9.Proia KK, Thota AB, Njie GJ, et al. Community Preventive Services Task Force Team-based care and improved blood pressure control. Am J Prev Med. 2014 Jul;47(1):86–99. doi: 10.1016/j.amepre.2014.03.003. DOI: http://dx.doi.org/10.1016/j.amepre.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Allen JK, Dennison-Himmelfarb CR, Szanton SL, et al. Community Outreach and Cardiovascular Health (COACH) Trial: a randomized, controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers. Circ Cardiovasc Qual Outcomes. 2011 Nov 1;4(6):595–602. doi: 10.1161/CIRCOUTCOMES.111.961573. DOI: http://dx.doi.org/10.1161/CIRCOUTCOMES.111.961573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor GT, Plume SK, Olmstead EM, et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. JAMA. 1996 Mar 20;275(11):841–6. DOI: http://dx.doi.org/10.1001/jama.1996.03530350023029. [PubMed] [Google Scholar]
- 12.Committee on Quality Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001. Mar 1, [Google Scholar]
- 13.Plsek P. Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Vol. 1. Washington, DC: National Academies Press; 2001. Mar, Redesigning health care with insights from the science of complex adaptive systems; pp. 309–22. [Google Scholar]
- 14.Reynolds CW. Flocks, herds and schools: a distributed behavior model. ACM SIGGRAPH Computer Graphics. 1987 Jul;21(4):25–34. DOI: http://dx.doi.org/10.1145/37402.37406. [Google Scholar]
- 15.Kottke TE, Pronk NP, Isham GJ. The simple health system rules that create value. Prev Chronic Dis. 2012;9:E49. DOI: http://dx.doi.org/10.5888/pcd9.110179. [PMC free article] [PubMed] [Google Scholar]
- 16.Huebsch JA, Kottke TE, McGinnis P, et al. A qualitative study of processes used to implement evidence-based care in a primary care practice. Fam Pract. 2015 Oct;32(5):578–83. doi: 10.1093/fampra/cmv045. DOI: http://dx.doi.org/10.1093/fampra/cmv045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis SM, Peterson JC, Helfrich CD, Cunningham-Sabo L. Introduction and conceptual model for utilization of prevention research. Am J Prev Med. 2007 Jul;33(1 Suppl):S1–5. doi: 10.1016/j.amepre.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Rogers EM. Diffusion of innovations. 5th ed. New York, NY: Free Press; 2003. [Google Scholar]
- 19.Tornatzky LG, Eveland JD, Boylan MG, et al. The process of technological innovation: reviewing the literature. Washington DC: National Science Foundation; 1983. [Google Scholar]
- 20.Minnesota HealthScores [Internet] Minneapolis, MN: Minnesota HealthScores; 2014. [cited 2014 May 13]. Available from: www.mnhealthscores.org/?p=our_reports_landing&landing=1. [Google Scholar]
- 21.Patient centered medical home resource center [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2014. [cited 2014 Aug 14]. Available from: https://pcmh.ahrq.gov/ [Google Scholar]
- 22.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002 Oct 16;288(15):1909–14. doi: 10.1001/jama.288.15.1909. DOI: http://dx.doi.org/10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 23.Kottke TE, Solberg LI, Brekke ML, Cabrera A, Marquez M. Will patient satisfaction set the preventive services implementation agenda? . Am J Prev Med. 1997 Jul-Aug;13(4):309–16. [PubMed] [Google Scholar]
- 24.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013 Aug 21;310(7):699–705. doi: 10.1001/jama.2013.108769. DOI: http://dx.doi.org/10.1001/jama.2013.108769. [DOI] [PMC free article] [PubMed] [Google Scholar]