Abstract
Objectives:
Trauma is the greatest cause of morbidity and mortality in paediatric/adolescent populations worldwide. This study aimed to describe trauma mechanisms, patterns and outcomes among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital (SQUH) in Muscat, Oman.
Methods:
This retrospective single-centre study involved all children ≤12 years old with blunt torso trauma admitted for paediatric surgical care at SQUH between January 2009 and December 2013. Medical records were analysed to collect demographic and clinical data.
Results:
A total of 70 children were admitted with blunt torso trauma during the study period, including 39 (55.7%) male patients. The mean age was 5.19 ± 2.66 years. Of the cohort, 35 children (50.0%) received their injuries after having been hit by cars as pedestrians, while 19 (27.1%) were injured by falls, 12 (17.1%) during car accidents as passengers and four (5.7%) by falling heavy objects. According to computed tomography scans, thoracic injuries were most common (65.7%), followed by abdominal injuries (42.9%). The most commonly involved solid organs were the liver (15.7%) and spleen (11.4%). The majority of the patients were managed conservatively (92.9%) with a good outcome (74.3%). The mortality rate was 7.1%. Most deaths were due to multisystem involvement.
Conclusion:
Among children with blunt torso trauma admitted to SQUH, the main mechanism of injury was motor vehicle accidents. As a result, parental education and enforcement of infant car seat/child seat belt laws are recommended. Conservative management was the most successful approach.
Keywords: Pediatrics, Trauma, Blunt Injury, Thoracic Injury, Abdominal Injury, Oman
Advances in Knowledge
- In this study, school-aged children were most often the victims of blunt torso trauma. Furthermore, trauma injuries were rarely isolated and most deaths were due to multisystem involvement.
Application to Patient Care
- As the findings of this study indicated that most cases of paediatric blunt trauma to the torso involved multiple systems, careful patient evaluation is of paramount importance to rule out intra-abdominal injuries.
- Nonoperative management was the most successful approach for cases of paediatric blunt torso trauma in the current study. As such, this approach is recommended, particularly when treating children with solid organ injuries.
Trauma is the single greatest cause of morbidity and mortality in paediatric or adolescent populations and an estimated one in four children require medical care due to unintentional trauma every year.1,2 Trauma can either be blunt or penetrating and different principles of management exist accordingly. Blunt trauma is more prevalent and usually involves multiple systems in children due to their small size.3 Isolated skeletal or head injuries are managed by the concerned specialties, while blunt trauma that involves other areas is known as blunt torso trauma. The torso is generally considered a single unit as thoracic and abdominal injuries tend to occur simultaenously.4 For this reason, children with this type of trauma require more vigilant assessment and the involvement of multidisciplinary teams in the management of their injuries.
In Oman, trauma is one of the most common causes of death in patients below 18 years of age.5 Since 2009, children with blunt torso trauma have been referred to the Sultan Qaboos University Hospital (SQUH), a tertiary care hospital in Muscat and one of the main trauma referral centres in Oman. Although SQUH meets many of the standards of a level I paediatric trauma centre, it is considered a level III paediatric trauma centre because the hospitalisation rate for children with trauma is less than 100 admissions per year.6 To the best of the authors’ knowledge, no study to date has yet documented the patterns, management practices and outcomes of paediatric blunt torso trauma cases in Oman. In order to improve the care of such patients, the current study therefore aimed to provide a detailed description of trauma mechanisms, patterns and outcomes among children hospitalised for the management of blunt torso trauma at SQUH.
Methods
This retrospective single-centre study was conducted at SQUH between January 2009 and December 2013. Medical records were obtained for all children ≤12 years old with thoracic, abdominal or combined injuries due to trauma who were admitted to SQUH for paediatric surgical care during the study period. Data were collected by two independent researchers using the hospital’s computerised database and records from the emergency, paediatric and surgical wards.
Demographic and clinical data were collected, including gender, age, mechanism of injury, associated injuries, Glasgow Coma Scale scores and clinical condition at presentation to the Emergency Department (ED). Diagnostic modalities used, radiological findings and management approaches were also recorded. Furthermore, admission to and duration of stay at the Paediatric Intensive Care Unit (PICU), utilisation of inotropic support (if needed), overall duration of hospital stay, intraoperative findings, transfers to other hospitals (if needed) and patient outcomes, including rates of complications, mortality and residual morbidity at discharge, were also noted. Radiological findings were validated by a senior radiologist at SQUH. Data were analysed using the Statistical Package for the Social Sciences (SPSS), Version 16 (IBM Corp., Chicago, Illinois, USA).
This study was approved by the Medical Research & Ethics Committee of the College of Medicine & Health Sciences, Sultan Qaboos University (MREC #903).
Results
Over the four-year study period, 7,417 paediatric patients were brought to the ED with a history of all-cause trauma, including 15 patients who were dead on arrival (incidence: 20/10,000 individuals) and 125 patients who were subsequently admitted (incidence: 650/10,000 individuals). Of those admitted, a total of 70 children (56.0%) presented with blunt torso trauma, including 39 males (55.7%) and 31 females (44.3%). These patients ranged in age from 0–12 years old, with a mean age of 5.19 ± 2.66 years. School-aged children (6–12 years old) were most commonly involved (n = 31; 44.3%). In terms of mechanism of injury, the majority were pedestrians who had been hit by cars (n = 35; 50.0%). Children also received blunt trauma injuries due to falls (n = 19; 27.1%), motor vehicle accidents in which the children were passengers (n = 12; 17.1%) and from falling heavy objects (n = 4; 5.7%) [Table 1].
Table 1:
Mechanism of trauma by age group among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 70)
| Mechanism of trauma | Age in years | Total | |||
|---|---|---|---|---|---|
| <1 | 1–3 | 4–5 | 6–12 | ||
| Pedestrian hit by car in MCV | 2 | 6 | 9 | 18 | 35 |
| Fall | 2 | 5 | 7 | 5 | 19 |
| Passenger in MVC | 2 | 2 | 1 | 7 | 12 |
| Fall of a heavy object | 0 | 2 | 1 | 1 | 4 |
| Total | 6 | 15 | 18 | 31 | 70 |
MVC = motor vehicle collision.
Chest and pelvic X-rays were the primary diagnostic modality; chest X-rays were normal for 53 patients (75.7%) while pelvic X-rays were normal for 70 patients (100.0%). Pneumothorax was evident on the chest X-rays of 15 patients (21.4%) and lung contusions were seen on the chest X-rays of two patients. Underlying thoracic injuries in 31 patients (44.3%) were not observed on chest X-rays; however, the injuries were subsequently observed on helical chest computed tomography (CT) scans. Most of the patients in the current study who were haemodynamically normal or responded to resuscitation were evaluated by intravenous contrast CTs of the head, chest, abdomen and pelvis. A total of 65 patients (92.9%) underwent abdominal CT scans with intravenous contrast; these detected 34 injuries in 29 patients. All cases of rib fracture were missed on initial chest X-rays (n = 5; 10.9%). Of the 37 cases with lung contusions, most were missed via X-ray (n = 35; 94.6%). Similarly, none of the pelvic fractures observed via CT scans (n = 14) were picked up by the pelvis X-rays. More than 50% of the abdominal CT scans were negative for intra-abdominal injuries.
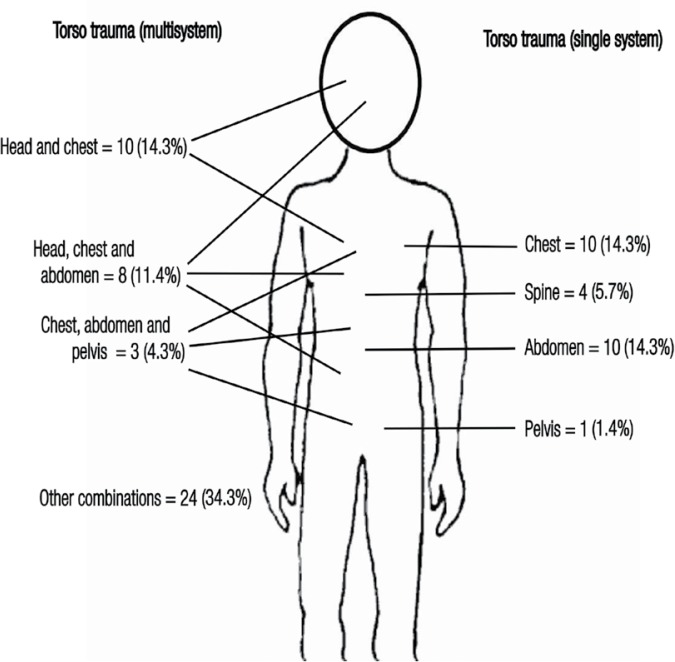
According to CT scans, single system thoracic injuries (n = 10; 14.3%) or multisystem thoracic injuries (n = 36; 51.4%) were most common (n = 46; 65.7%), followed by abdominal injuries (n = 30; 42.9%). Of the thoracic injuries, the most common injuries were lung contusions (n = 37; 80.4%), followed by pneumothorax (n = 18; 39.1%), haemothorax (n = 6; 13.0%) and rib fractures (n = 5; 10.9%) [Table 2]. Among those with abdominal trauma, 10 patients (33.3%) had single system abdominal injuries while 20 (66.7%) had multisystem injuries [Figure 1]. Two patients, one hit by a car causing a perforation of the small bowel with a mesenteric tear and extensive liver damage and the other patient with a duodenal blow-out due to a fall, had hollow viscous injuries which were managed by exploratory laparotomy; another two patients had multisystem involvement which developed into haemodynamic instability. Intra-abdominal injuries were noted in 29 patients (44.6%) via CT scan, with one patient taken to the operating theatre without initial imaging. The most commonly involved solid organs were the liver (n = 11; 15.7%)—in isolation (n = 8; 72.7%) or in combination with other organs (n = 3; 27.3%)—and the spleen (n = 8; 11.4%). Seven patients had a minimal amount of free fluid in the absence of any solid or hollow viscus injury. The majority of the children with single or multiple solid organ injuries were managed successfully through a conservative approach (88.9%) [Table 3].
Table 2:
Thoracic injuries among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 46)
| Type of injury | Single system | Multisystem | Total |
|---|---|---|---|
| Lung contusions | 7 | 16 | 23 |
| Lung contusions and pneumothorax | 1 | 7 | 8 |
| Pneumothorax | 0 | 4 | 4 |
| Haemopneumothorax | 1 | 2 | 3 |
| Lung contusions and rib fractures | 0 | 3 | 3 |
| Lung contusions, pneumothorax and haemothorax | 1 | 2 | 3 |
| Rib fractures | 0 | 2 | 2 |
| Total | 10 | 36 | 46 |
Figure 1:
Patterns of blunt torso trauma among children admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 70). All injuries were diagnosed via computed tomography.
Table 3:
Intra-abdominal injuries among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 30)
| Type of injury | Total | Grade | Management | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Operative (successful) | NOM (successful) | ||
| Solid organ injuries | 18 | - | - | - | - | - | - | - |
| Liver alone | 8 | 5 | - | 1 | 2 | - | 1 (0) | 7 (7) |
| Spleen alone | 6 | 2 | - | 2 | 1 | 1 | 1 (0) | 5 (5) |
| Liver and spleen | 2 | 1* | - | - | 2† | 1‡ | - | 2 (2) |
| Renal | 2 | - | - | 1 | - | 1 | - | 2 (2) |
| Other IAIs | 12 | - | - | - | - | - | - | - |
| Adrenal with retroperitoneal haematoma | 2 | 1 | - | 1 | - | - | - | 2 (1) |
| Bowel | 1 | - | - | - | - | - | 1 (1) | - |
| Liver and bowel | 1 | - | - | - | 1‡ | - | 1 (0) | - |
| Suspected IAI | 1 | - | - | - | - | - | 1 (0) | - |
| Free abdominal fluid without obvious solid organ injury | 7 | - | - | - | - | - | - | 7 (7) |
IAI = intra-abdominal injury; NOM = nonoperative management.
Spleen injury grade only.
Spleen and liver injury grades for two different patients, respectively.
Liver injury grade only.
All of the patients were managed according to advanced trauma life support protocols. Five patients (7.1%) required surgical interventions while the rest of the patients were managed conservatively (92.9%). A total of 15 patients (32.6%) with thoracic injuries required chest intubation in the ED due to X-ray evidence of pneumothorax. Three additional cases of pneumothorax required chest intubation due to helical chest CT findings. In total, 62 patients (88.6%) were haemodynamically stable at presentation. Of the eight patients (11.4%) who were not, seven (87.5%) responded to resuscitation while the remaining patient underwent an exploratory laparotomy without an initial abdominal CT scan; the surgical exploration revealed a splenic injury which required a splenectomy. Unfortunately, the patient died five days after the operation while in the PICU. Four patients (6.2%) required an exploratory laparotomy after an abdominal CT scan. One patient died intra-operatively and the other three patients were moved to the PICU. Two of these patients died while in the PICU; the remaining patient, who had an isolated small bowel injury, survived. Another patient who had extensive retroperitoneal haematoma and was on expectant management died in the PICU. The mortality rate was therefore 7.1% (n = 5). Most of the patients who died had multisystem injuries [Table 4].
Table 4:
Fatalities among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 70)
| Age in years/gender | Mechanism of injury | Haemodynamic status at presentation | Type of injuries | Management | |||
|---|---|---|---|---|---|---|---|
| Head | Chest | Abdomen | Other | ||||
| 2/F | Pedestrian hit by car | Unstable | Severe | - | Liver and bowel | Retroperitoneal haematoma | Laparotomy |
| 5/F | Pedestrian hit by car | Unstable | Severe | Haemopneumothorax and rib fracture | Liver | - | Laparotomy |
| 6/M | Pedestrian hit by car | Unstable | Severe | Lung contusion, pneumothorax and haemothorax | Adrenal | Retroperitoneal haematoma and pelvic fracture | Expectant |
| 6/M | Pedestrian hit by car | Unstable | Severe | - | Spleen | Retroperitoneal haematoma and pelvic fracture | Laparotomy and splenectomy |
| 7/M | Pedestrian hit by car | Unstable | Severe | - | Suspected injury | - | Laparotomy* |
F = female; M = male.
Negative.
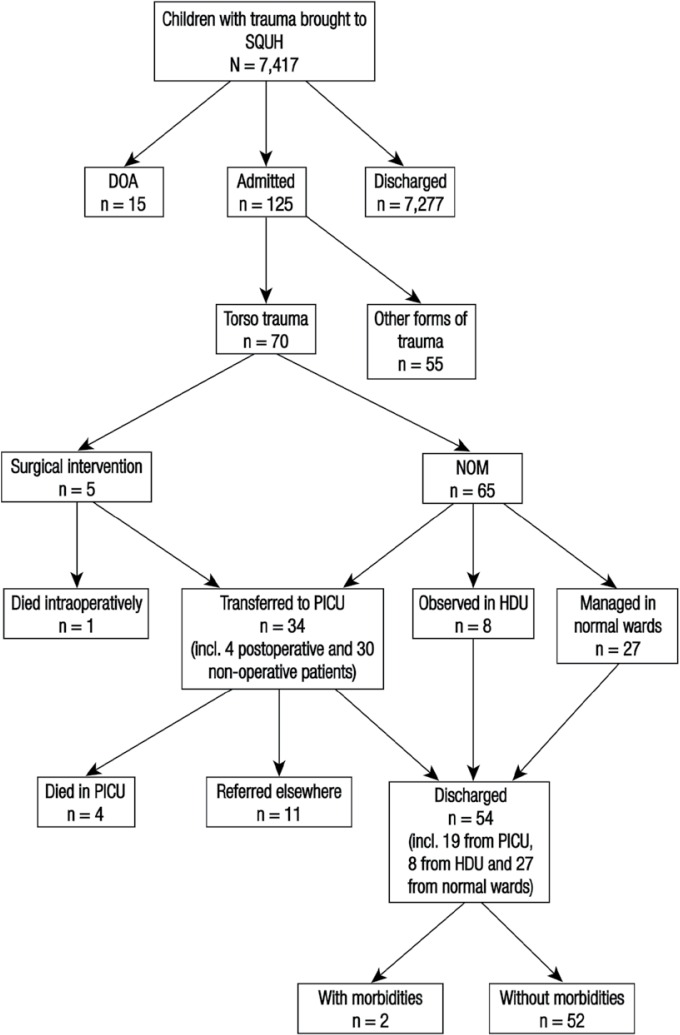
In total, 35 patients (50.0%) were managed in wards—eight (22.9%) in a high dependency unit and 27 (77.1%) in normal wards—while 34 (48.6%) required observation in the PICU. Of those transferred to the PICU, four (11.8%) were moved post-surgery while 30 (88.2%) were transferred directly after CT evaluation. In the PICU, 21 patients (61.8%) required invasive ventilation (range of duration: <24 hours–29 days). All of the patients admitted to the PICU required blood transfusions (1–13 units of 10 mL/kg of packed red blood cells) and 15 patients (44.1%) required inotropic support (range of duration: <1 hour–10 days). Of the surviving patients, 52 patients (74.3%) were discharged without any residual morbidities, two patients (2.9%) were discharged with neurological complications and 11 patients (32.4%) were referred to other hospitals for further management [Figure 2]. The two patients who were discharged with severe head injuries developed permanent disabilities.
Figure 2:
Flowchart showing management approaches and treatment outcomes among children with blunt torso trauma admitted to the Sultan Qaboos University Hospital, Muscat, Oman (N = 70).
SQUH = Sultan Qaboos University Hospital; DOA = dead on arrival; NOM = nonoperative management; PICU = paediatric intensive care unit; HDU = high-dependency unit; incl. = including.
Discussion
Factors which determine the types and patterns of paediatric injury include the age and gender of the patient group and the cause of trauma. In the current study, the age group most commonly involved was 6–12-year-olds and children were most often injured as a result of being hit by a vehicle as a pedestrian. These findings could possibly be due to the fact that children of this age group are often allowed to play in the streets unattended. In contrast, toddlers (<1-year-olds) and preschool-aged children (1–3-year-olds) were collectively more likely to be injured in a fall or by having a heavy object fall upon them. As a result, parental education and strict enforcement of infant car seat and child seat belt laws are recommended as strategies to reduce the number of paediatric trauma patients in Oman. Regarding gender, slightly more male children presented with torso trauma than females in the current study. This is consistent with findings from other research—being male has been documented as a risk factor for trauma in many studies, with differences between males and females in involvement in trauma appearing from the first year of life.7,8 In children under 15 years of age, the mortality rate due to trauma is reportedly 24% higher in boys than girls.7,8 Differences in behaviour between genders may be one reason for such findings, as well as higher activity levels, greater freedom to play alone and increased involvement in risky sports among males.
Most of the patients in the current study who were haemodynamically stable were evaluated by CTs of the head, chest, abdomen and pelvis. Although CT scans are considered the primary diagnostic modality for the evaluation of haemodynamically stable children with torso trauma, there are concerns of cost and the potential for radiation-associated malignancies.9 Recently, a clinical decision rule (CDR) has been suggested to identify children who are at very low risk of intra-abdominal injuries and hence would not require abdominal CTs; however, although cost-effective, the validity of this CDR still requires further research.9,10 In the current study, the CT scan rate appears high; however, this may be because all children with torso trauma detected on CT scans were included in the study cohort. Hence, the exact CT scan rate for children presenting with torso trauma at SQUH is unknown. Nevertheless, CT scans were effective in the detection of additional injuries, including underlying lung injuries such as lung contusions and rib fractures. Similarly, none of the pelvic fractures were picked up by the pelvis X-rays.
The major concern in children with torso trauma is diagnosing potential intra-abdominal injuries. In the current study, all of the patients who underwent an abdominal CT did so with intravenous contrast. Oral contrast CTs are not used to screen paediatric trauma patients at SQUH as they are time-consuming and may be unsuccessful if the patient is scared or nauseous. Delayed emptying can also increase the risk of aspiration and may mask the imaging of the liver and spleen. Moreover, Ellison et al. recently showed that routine use of oral contrast is unnecessary and delays performance of CT scans and angiographic studies, if indicated.11 In the current study, more than half of the abdominal CT scans were negative for intra-abdominal injuries. However, CT scans can nonetheless play an important role in the management of patients with torso trauma as they can exclude potential intra-abdominal or pelvic sources of blood loss.12
The thorax was the most commonly involved region in combination with other regions in the current study. This is consistent with the findings of Peres et al., who described thoracic involvement in 50% of children with polytrauma.13 Although lung contusions were the most common injury, the majority of these were not observed via chest X-ray; furthermore, very few cases of associated rib fractures were found among the children in the current study. Karadaş et al. reported a similarly low rib fracture incidence in children under 19 years of age (11.1%).14 These findings imply that lung parenchymal injuries can occur in the absence of associated rib fractures, perhaps due to the greater pliability of the rib cage in children; furthermore, such injuries can be missed on initial chest X-rays.14,15
An interesting finding on the CT scans of some of the patients in the current study was the presence of more than a trace amount of free fluid in the absence of solid organ injuries. The presence of this fluid indicates a mesenteric tear or hollow viscous injury, both of which require surgical intervention; however, there is a lack of consensus on the correct approach to be taken in such cases.16 Hollow viscous injuries pose a significant diagnostic challenge and management options include performing another CT scan with oral contrast or a diagnostic laparoscopy.12,17,18 The reported incidence of hollow viscous injuries among children with polytrauma varies from 1–23% and may involve any part of the gastrointestinal tract.17 Only two patients were found to have such injuries in the current study. Hollow viscous injuries involving other organs like the stomach, large bowel or rectum were not found in the study. Abdominal exploration was performed for five patients due to either hollow viscous injuries or haemodynamic instability.
In the current study, all thoracic injuries were managed conservatively or by chest intubation, with the intention to intervene in case of haemodynamic instability or the development of peritonitis. Ismail et al. reported that the most common intervention for children with blunt thoracic trauma was chest intubation.19 In the present study, none of the patients required thoracotomies. Currently, the management of solid organ injuries in stable children with blunt trauma is primarily nonoperative.20 In the current study, the vast majority of the children with single or multiple solid organ injuries were managed successfully through a conservative approach. Failed nonoperative management is concerning because it carries a higher mortality rate than operative management (∼5%).21 Potential reasons for the high success rate of conservative management in the present study could include the availability of support, blood and blood products received by the patients in the PICU. However, another major contributor to the success rate may have been the absence of high-risk factors such as bicycle-related injuries, isolated pancreatic injuries and grade five solid organ injuries.21
The current study had a number of limitations. Firstly, only children aged up to 12 years old were included in the study, although most paediatric trauma series have an upper age limit of 15–19 years old; for this reason, differences in trauma patterns may exist.8,13,14,17 Secondly, the current study was retrospective and focused only on hospitalised patients admitted to a single trauma centre; as such, the findings may not represent the exact CT scan rate at SQUH or the true number of paediatric blunt torso trauma cases occurring in Oman during the study period. Thirdly, the current study did not describe the precise management algorithms utilised by the ED physicians, if any. The results of this study should hence be interpreted in light of the above limitations.
Conclusion
The main mechanism of torso trauma injury among children admitted to SQUH involved motor vehicle accidents. In order to reduce the number of paediatric trauma patients, parental education and strict enforcement of infant car seat and child seat belt laws is recommended. The majority of patients were managed conservatively with a good outcome. The optimal approach in treating paediatric trauma patients therefore seems to be conservative management. Mortality, although low, stemmed from multisystem involvement.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Seid T, Ramaiah R, Grabinsky A. Pre-hospital care of pediatric patients with trauma. Int J Crit Illn Inj Sci. 2012;2:114–20. doi: 10.4103/2229-5151.100887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danesco ER, Miller TR, Spicer RS. Incidence and costs of 1987–1994 childhood injuries: Demographic breakdowns. Pediatrics. 2000;105:E27. doi: 10.1542/peds.105.2.e27. [DOI] [PubMed] [Google Scholar]
- 3.Inaba AS, Seward PN. An approach to pediatric trauma; Unique anatomic and pathophysiologic aspects of the pediatric patient. Emerg Med Clin North Am. 1991;9:523–48. [PubMed] [Google Scholar]
- 4.Trunkey DD. Torso trauma. Curr Probl Surg. 1987;24:209–65. doi: 10.1016/0011-3840(87)90016-5. [DOI] [PubMed] [Google Scholar]
- 5.Hill AG, Muyeed AZ, al-Lawati JA, editors. The mortality and health transitions in Oman: Patterns and processes. From: www.2unicef.org/spanish/evaldatabase/files/2000_Oman_health_transition_rec_347399pdf Accessed: Feb 2016.
- 6.Missouri Department of Health & Senior Services 19 CSR 30-40.440: Standards for pediatric trauma center designation. From: health.mo.gov/living/healthcondiseases/chronic/tcdsystem/pdf/pediatric_trauma_designation_7-21-10.pdf Accessed: Feb 2016.
- 7.World Health Organization, Unicef World report on child injury prevention. From: www.unicef.org/eapro/World_report.pdf Accessed: Feb 2016. [PubMed]
- 8.Fabricant PD, Robles A, Downey-Zayas T, Do HT, Marx RG, Widmann RF, et al. Development and validation of a pediatric sports activity rating scale: The Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS) Am J Sports Med. 2013;41:2421–9. doi: 10.1177/0363546513496548. [DOI] [PubMed] [Google Scholar]
- 9.Streck CJ, Jr, Jewett BM, Wahlquist AH, Gutierrez PS, Russell WS. Evaluation for intra-abdominal injury in children after blunt torso trauma: Can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg. 2012;73:371–6. doi: 10.1097/TA.0b013e31825840ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishijima DK, Yang Z, Clark JA, Kuppermann N, Holmes JF, Melnikow J. A cost-effectiveness analysis comparing a clinical decision rule versus usual care to risk stratify children for intraabdominal injury after blunt torso trauma. Acad Emerg Med. 2013;20:1131–8. doi: 10.1111/acem.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ellison AM, Quayle KS, Bonsu B, Garcia M, Blumberg S, Rogers A, et al. Use of oral contrast for abdominal computed tomography in children with blunt torso trauma. Ann Emerg Med. 2015;66:107–14. doi: 10.1016/j.annemergmed.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 12.Sivit CJ. Abdominal trauma imaging: Imaging choices and appropriateness. Pediatr Radiol. 2009;39:S158–60. doi: 10.1007/s00247-008-1127-z. [DOI] [PubMed] [Google Scholar]
- 13.Peres A, Chaves M, Vieira M, Santos E, Cruz J, Feijó S, et al. [Polytraumatism in childhood: It can be more than it seems] Acta Med Port. 2010;23:511–14. [PubMed] [Google Scholar]
- 14.Karadaş S, Gönüllü H, Çobanoğlu U, Selvi F, Dursun R, Güner S. Comparison of pediatric and adult patients with thoracic trauma in emergency department. J Exp Clin Med. 2013;30:323–6. doi: 10.5835/jecm.omu.30.04.008. [DOI] [Google Scholar]
- 15.Tovar JA. The lung and pediatric trauma. Semin Pediatr Surg. 2008;17:53–9. doi: 10.1053/j.sempedsurg.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Banz VM, Butt MU, Zimmermann H, Jeger V, Exadaktylos AK. Free abdominal fluid without obvious solid organ injury upon CT imaging: An actual problem or simply over-diagnosing? J Trauma Manag Outcomes. 2009;3:10. doi: 10.1186/1752-2897-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chirdan LB, Uba AF, Chirdan OO. Gastrointestinal injuries following blunt abdominal trauma in children. Niger J Clin Pract. 2008;3:250–3. [PubMed] [Google Scholar]
- 18.Adelgais KM, Kuppermann N, Kooistra J, Garcia M, Monroe DJ, Mahajan P, et al. Accuracy of the abdominal examination for identifying children with blunt intra-abdominal injuries. J Pediatr. 2014;165:1230–5. doi: 10.1016/j.jpeds.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 19.Ismail MF, al-Refaie RI. Chest trauma in children, single center experience. Arch Bronconeumol. 2012;48:362–6. doi: 10.1016/j.arbres.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 20.Gaines BA. Intra-abdominal solid organ injury in children: Diagnosis and treatment. J Trauma. 2009;67:S135–9. doi: 10.1097/TA.0b013e3181adc17a. [DOI] [PubMed] [Google Scholar]
- 21.Holmes JH, 4th, Wiebe DJ, Tataria M, Mattix KD, Mooney DP, Scaife ER, et al. The failure of nonoperative management in pediatric solid organ injury: A multi-institutional experience. J Trauma. 2005;59:1309–13. doi: 10.1097/01.ta.0000197366.38404.79. [DOI] [PubMed] [Google Scholar]