Abstract
Study Design Retrospective radiographic study.
Objective To investigate changes and correlations of cervical sagittal alignment including T1 slope before and after occipitocervical corrective surgery. We also investigated the relevance for preoperative planning.
Methods We conducted a retrospective radiographic analysis of 27 patients who underwent surgery for occipitocervical deformity. There were 7 men and 20 women with a mean age of 56.0 years. Mean follow-up was 68.0 months (range 24 to 120). The radiographic parameters measured before surgery and at final follow-up included McGregor slope, T1 slope, occipito (O)–C2 angle, O–C7 angle, and C2–C7 angle. Pearson correlation coefficient was used to examine the correlation between the radiographic parameters.
Results There was a stronger positive correlation between the T1 slope and the O–C7 angle both preoperatively and postoperatively (r = 0.72 and r = 0.83, respectively) than between the T1 slope and the C2–C7 angle (r = 0.60 and r = 0.76, respectively). The O–C2 angle and C2–C7 angle had inverse correlations to each other both pre- and postoperatively (r = − 0.50 and −0.45). McGregor slope and T1 slope did not significantly change postoperatively at final follow-up. Increase in O–C2 angle after surgery (mean change, 10.7 degrees) inversely correlated with decrease in postoperative C2–C7 angle (mean change, 12.2 degrees). As result of these complementary changes, O–C7 angle did not statistically change.
Conclusions Our results suggest that the O–C7 angle is regulated by T1 slope and the corresponding O–C7 angle is divided into the O–C2 and C2–C7 angles, which have inverse correlation to each other and then maintain McGregor slope (horizontal gaze).
Keywords: cervical alignment, sagittal alignment, occipitocervical fusion, deformity
Introduction
Careful consideration of the sagittal parameters of the spine and pelvis is essential for the treatment of the spine, particularly the thoracolumbar spine.1 2 3 Although malalignment of the thoracolumbar spine is associated with poor long-term clinical outcomes and postoperative health-related quality of life, the clinical impact of cervical alignment has not been sufficiently investigated.3 4 5 6 Prior studies indicated that the significance of sagittal parameters such as the negative impact of kyphotic deformity in cervical laminoplasty or the positive sagittal malalignment following posterior cervical fusion correlated with the severity of disability.7 8 The occipito (O)–C2 angle reportedly accounts for 77% of cervical lordosis, and a correlation between the alignment of the upper and lower cervical spine has been already reported.9 10 Although there are studies on the relationship between the atlantoaxial angle and subaxial cervical lordosis after atlantoaxial fixation,11 12 13 14 there are few studies on the occipitocervical angle in cervical sagittal alignment.15 16 Furthermore, although several reports indicated the correlation between the T1 slope and thoracolumbar sagittal alignment,17 18 19 only few studies reported the correlation of the T1 slope and cervical sagittal alignment.9 The purpose of this study was to examine the potential impact of the occipitocervical fusion on subaxial sagittal alignment and to clarify the correlations of these sagittal parameters. We also investigated the relevance for preoperative planning.
Materials and Methods
A total of 33 consecutive patients who underwent posterior O–C3 fixation for the treatment of occipitocervical deformity between 2002 and 2011 were retrospectively investigated. Six patients did not fulfill at least one of the necessary parameters and were excluded, and thus 27 patients were included in the present study. The surgical procedures consisted of a posterior approach, and we used a screw and loop rod system with posterior wiring.
The McGregor slope, T1 slope, O–C2 angle, O–C7 angle, and C2–C7 angle were measured preoperatively and at the final follow-up on lateral cervical X-ray in the sitting position. The McGregor slope and T1 slope are defined as the angle of the McGregor line and T1 superior end plate against a horizontal line, respectively.20 The O–C2 angle and O–C7 angle consist of the angles of the C2 inferior end plate and C7 inferior end plate against the McGregor line, respectively. The C2–C7 angle was measured using the Cobb method between the inferior end plate of C2 and that of C7. Considering the role of the occipitocervical angle in cervical alignment, it is essential to include the craniocervical junction in the assessment of cervical sagittal alignment. Thus we used the McGregor slope to assess cranial position. To minimize the effect of change in the thoracolumbar alignment, we evaluated the X-rays of patients while sitting, which can provide direct information of the occipitocervical fixation for cervical alignment.
The severity of myelopathy was assessed using the Japanese Orthopaedic Association (JOA) score. Two patients could not be evaluated, one because of cerebral infarction after surgery and one because of mental retardation.
The Ethics Committee of the Gunma Spine Center approved the study protocol, and informed consent was obtained from the study participant or the person authorized to give consent.
The Statistical Package for the Social Sciences (SPSS version 21.0, SPSS Inc., Chicago, Illinois, United States) software was used for all statistical analysis. The correlations between the parameters were analyzed with the Pearson correlation coefficient. The relationship between the postoperative cervical lordosis and radiographic parameters was calculated using forward stepwise multivariate linear regression analysis. Statistical analyses were two-sided, and a p value of ≤0.05 was considered statistically significant.
Results
There were 7 men and 20 women. The average age at surgery was 56.0 years (range 14 to 83). The mean follow-up period was 68.0 months (range 24 to 120). Twenty-four patients had rheumatoid arthritis, 1 had os odontoideum, 1 had Klippel-Feil syndrome, and 1 had spondylosis. Myelopathy was observed in 21 patients. Pre- and postoperative JOA scores of the patients with myelopathy are listed in Table 1. The mean preoperative JOA score was 11.7, and it significantly improved to 13.6 postoperatively. The recovery rate of JOA score was 45%. With regard to surgical procedure, 23 patients underwent C1 posterior arch resection. Pedicle screws were used at C2 in 2 patients and at C3 in 21 patients. Sublaminar wiring was used at C1 in 1 patient, at C2 in 26 patients, and at C3 in 12 patients. Five patients received subaxial cervical laminoplasty. Postoperative screw breakage was observed in 1 case, and postoperative instability (olisthesis ≥ 3 mm) was observed in 2 cases. Deterioration of the subaxial cervical kyphotic deformity was observed in 1 case, and de novo kyphotic deformity was observed in 2 cases. One patient with rheumatoid arthritis required revision surgery at 28 months after primary surgery because of deterioration and C5–C6 instability.
Table 1. Pre- and postoperative parameters values and JOA scores.
| Min | Max | Mean | SD | p Value | |
|---|---|---|---|---|---|
| McGregor slope pre | −20 | 9 | −4.0 | 6.7 | 0.07 |
| McGregor slope post | −11 | 9 | −2.0 | 5.8 | |
| T1 slope pre | 17 | 47 | 30.9 | 7.8 | 0.40 |
| T1 slope post | 12 | 64 | 32.5 | 12.4 | |
| O–C2 angle pre | −13 | 25 | 4.7 | 10.7 | 0.0001 |
| O–C2 angle post | −4 | 38 | 15.4 | 10.7 | |
| C2–C7 angle pre | 4 | 50 | 21.8 | 13.8 | 0.002 |
| C2–C7 angle post | −17 | 42 | 9.6 | 15.2 | |
| O–C7 angle pre | 4 | 45 | 26.4 | 12.6 | 0.46 |
| O–C7 angle post | 4 | 60 | 25.0 | 14.1 | |
| JOA score pre | 7.0 | 16.0 | 11.7 | 2.9 | 0.0001 |
| JOA score post | 8.5 | 17.0 | 13.6 | 2.7 |
Note: Wilcoxon signed rank test.
Abbreviations: JOA, Japanese Orthopaedic Association; Min, minimum; Max, maximum; O, occipito; pre, preoperative value; post, postoperative value; SD, standard deviation.
The measured values of the radiographic parameters are listed in Table 1. The McGregor slope did not significantly change after surgery (p = 0.07), despite a statistically significant increase in the O–C2 angle (mean change 10.7 degrees, p < 0.001) for correction of occipitocervical kyphosis. In contrast to the increase in the O–C2 angle, the C2–C7 angle significantly decreased (mean change 12.2 degrees, p = 0.002). As a result of these changes, the O–C7 angle and T1 slope did not significantly change postoperatively (p = 0.46 and 0.40, respectively). Correlations between the radiographic parameters are summarized in Table 2 and Fig. 1. The pre- and postoperative McGregor slopes were significantly correlated (r = 0.63), and a similar correlation was observed for T1 slope (r = 0.62). A previous study indicated correlation between the T1 slope and C2–C7 angle and between the C2–C7 angle and O–C2 angle.9 But in this study, the correlation coefficients between the T1 slope and the O–C7 angle both preoperatively and postoperatively (r = 0.72 and r = 0.83, respectively) were higher than between the T1 slope and the C2–C7 angle (r = 0.60 and r = 0.76, respectively). We observed an inverse correlation between the O–C2 and C2–C7 angles pre- and postoperatively (r = − 0.50 and r = − 0.45, respectively). The JOA score and its recovery rate did not correlate with the radiographic cervical sagittal parameters.
Table 2. Pearson correlation coefficient between the parameters.
| McGregor slope pre | T1 slope pre | O–C2 pre | O–C7 pre | C2–C7 pre | McGregor slope post | T1 slope post | O–C2 post | O–C7 post | C2–C7 post | |
|---|---|---|---|---|---|---|---|---|---|---|
| McGregor slope pre | – | −0.16 | −0.39a | −0.68b | −0.31 | 0.63b | −0.06 | −0.42a | −0.38 | −0.06 |
| T1 slope pre | – | 0.08 | 0.72b | 0.60b | −0.31 | 0.62b | 0.26 | 0.68b | 0.45a | |
| O–C2 pre | – | 0.30 | −0.50c | −0.38 | 0.15 | 0.35 | 0.28 | 0.01 | ||
| O–C7 pre | – | 0.67b | −0.55c | 0.42a | 0.60b | 0.72b | 0.25 | |||
| C2–C7 pre | – | −0.20 | 0.27 | 0.27 | 0.44a | 0.22 | ||||
| McGregor slope post | – | 0.10 | −0.40a | −0.28 | 0.02 | |||||
| T1 slope post | – | 0.01 | 0.83b | 0.76b | ||||||
| O–C2 post | – | 0.27 | −0.45a | |||||||
| O–C7 post | – | 0.74b |
Abbreviations: pre, preoperative value; O, occipito; post, postoperative value.
p < 0.05.
p < 0.001.
p < 0.01.
Fig. 1.
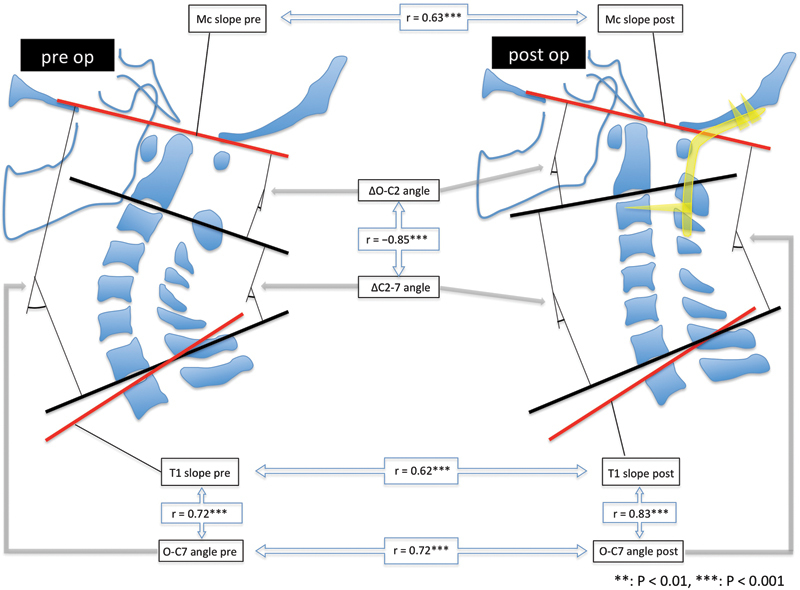
Correlations between the cervical parameters. Abbreviations: Δ, change between preoperative and postoperative values; Mc, McGregor; pre, preoperative values; post, postoperative values.
Table 3 shows the correlation coefficient between the pre- and postoperative parameters. There was an inverse correlation between the mean pre- versus postoperative change (Δ) in O–C2, the angle created by correction surgery, and ΔC2–C7, the reciprocal change of the correction angle (Fig. 2). The ΔO–C7 angle, which is the sum of these two changes, was correlated with the ΔT1 slope (r = 0.76).
Table 3. Pearson correlation coefficient between the pre- and postoperative change of parameters.
| ΔMcGregor slope | ΔT1 slope | ΔO–C2 | ΔO–C7 | ΔC2–C7 | |
|---|---|---|---|---|---|
| ΔMcGregor slope | – | 0.38 | 0.05 | −0.05 | −0.06 |
| ΔT1 slope | – | −0.28 | 0.76a | 0.61a | |
| ΔO–C2 | – | −0.34 | −0.85a | ||
| ΔO–C7 | – | 0.78a |
Abbreviations: Δ, change between pre- and postoperative values; O, occipito.
p < 0.001.
Fig. 2.
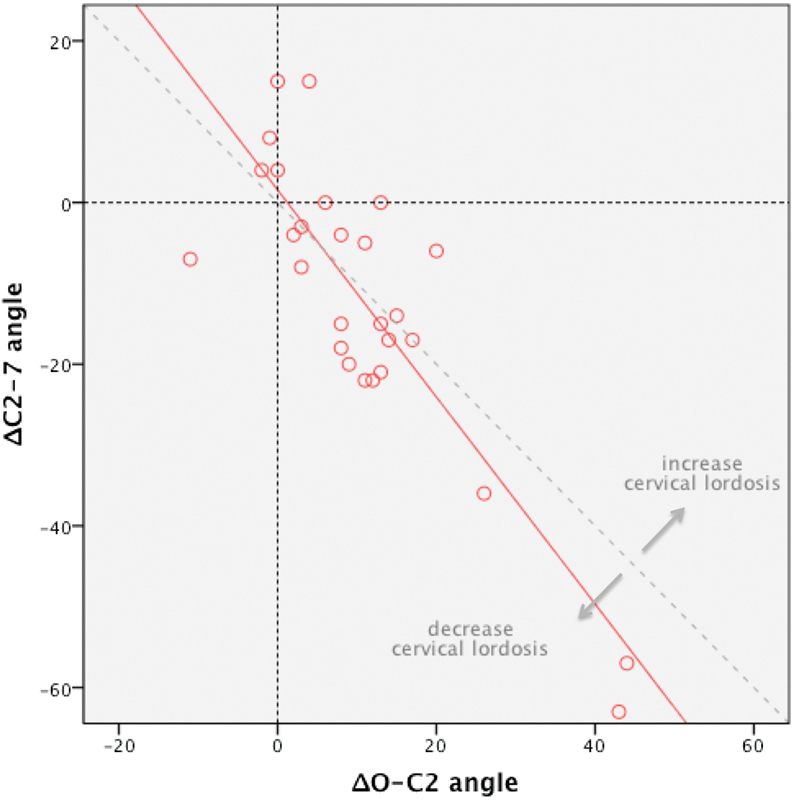
Correlation between ΔO–C2 angle and ΔC2–C7 angle. Abbreviations: Δ, change between preoperative and postoperative values; O, occipito.
We conducted a multiple linear regression model for postoperative cervical lordosis to predict the postoperative cervical subaxial kyphotic deformity. We used preoperative parameters and postoperative O–C2 angle for the analysis and excluded the McGregor and T1 slopes and the C2–C7 angle from this analysis to avoid multicollinearity with the O–C7 angle. The predicted C2–C7 angle model was 4.085 + 0.988 · O–C7 pre −1.340 · O–C2 post (p < 0.001). The formula had a strong correlation (r = 0.79) with the postoperative C2–C7 angle (Fig. 3).
Fig. 3.
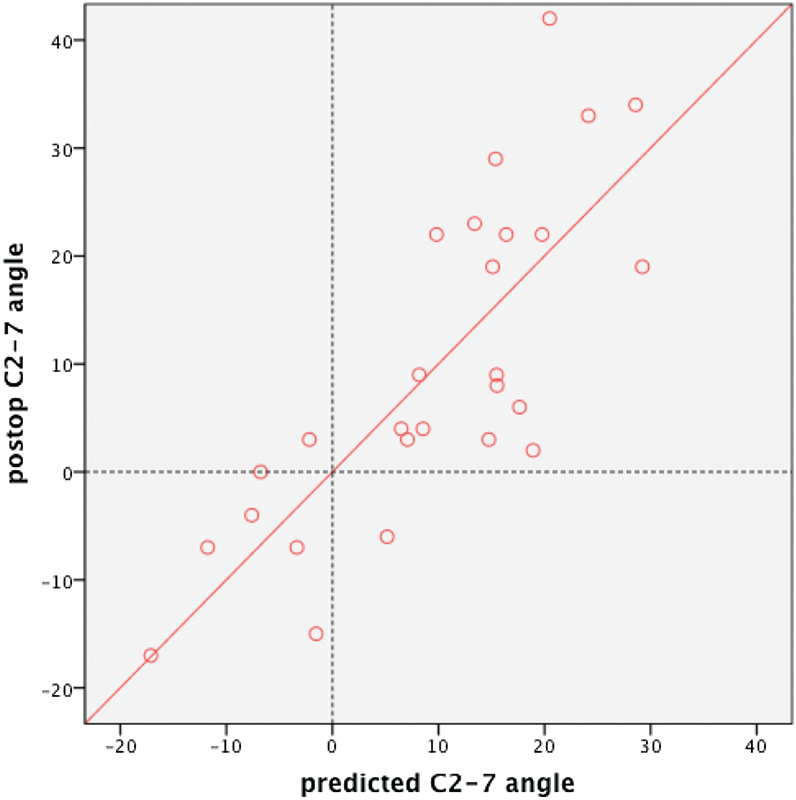
Correlation between postoperative C2–C7 angle and predicted C2–7 angle.
Discussion
In this study, we found that the correlation coefficient between the T1 slope and the O–C7 angle (O–C2 angle plus C2–C7 angle) is higher than that with the C2–C7 angle alone both pre- and postoperatively. Correlations between the T1 slope and C2–C7 lordosis and between the O–C2 angle and C2–C7 lordosis were mentioned in previous studies.6 9 These results suggest that the subaxial cervical spine compensated for the deformity of the upper cervical spine preoperatively, and the entire cervical spine was realigned against the T1 slope, which represents thoracolumbar spine alignment, to maintain the McGregor slope (horizontal gaze). After surgery, increases of the occipitocervical angle led to decreases of the subaxial cervical lordosis to maintain whole cervical lordosis against the T1 slope. In this study, we used the McGregor slope as a parameter of skull alignment, which can be measured in a normal lateral cervical X-ray.20 The McGregor line is the most reproducible and reliable method for measuring the occipitocervical angle among the lines of the skull base, including the McGregor, Chamberlain, and McRae lines.21 22 The McGregor slope was expected to maintain its angle even after occipitocervical surgery for horizontal gaze.20
In addition, we found that the majority of the correction angles of the upper cervical spine were absorbed by reciprocal change of the subaxial cervical spine at the final follow-up (Fig. 2). Preoperatively, C2–C7 created hyperlordosis if there was O–C2 kyphotic deformity to maintain the horizontal gaze. After occipitocervical corrective surgery, subaxial lordosis decreased to absorb the increase of occipitocervical lordosis, and the horizontal gaze was maintained. This result indicates that an excessive lordosis at the craniocervical junction by correction surgery can lead to kyphotic changes of the subaxial cervical spine, which was also noted in a previous study.16 However, that study included both occipito-atlanto-axial fusion and atlantoaxial fusion; thus, in some cases, the correction angle could be absorbed not only by the subaxial spine but also by the atlanto-occipital junction. Therefore, to the best of our knowledge, this study is the first to show the direct impact of occipitocervical correction on subaxial cervical alignments. The postoperative C2–C7 angle absorbed most of the upper cervical correction angle because the O–C7 angle was postoperatively maintained. Fig. 2 shows the correlation between the ΔO–C2 and ΔC2–C7 angles. The correction angle of the upper cervical deformity was absorbed by a decrease of the subaxial lordosis, even if the correction angle was ≥20 degrees. Fig. 2 shows that some patients had increased or decreased cervical lordosis. The greatest cause of large increases of cervical lordosis was the increase of T1 slope, which is suggestive of a thoracolumbar kyphotic deformity such as a compression fracture. The greatest cause of decreases of cervical lordosis was postoperative subaxial kyphotic deformity. Figs. 4, 5, 6, and 7 show representative cases of this study.
Fig. 4.
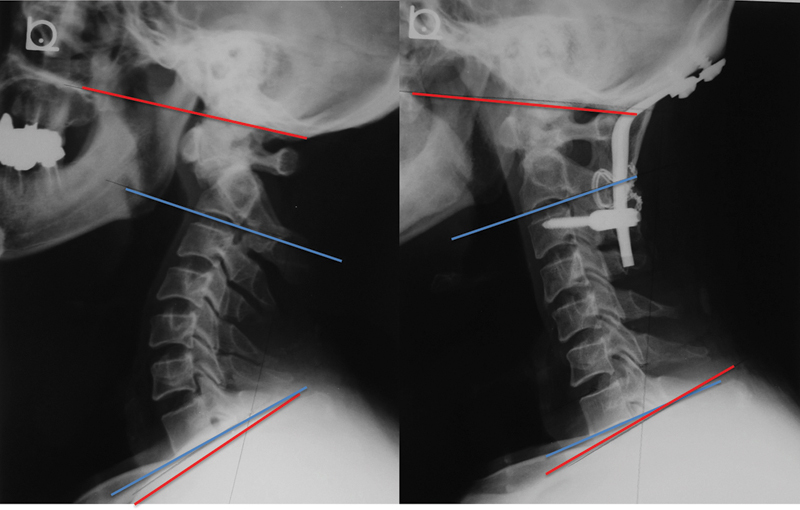
Case 1. A 54-year-old man with os odontoideum. Preoperative (left) and 3 years postoperative (right) X-rays. Occipitocervical kyphosis was corrected and lordosis gained at 3 years postoperatively. Conversely, subaxial lordosis decreased, and the McGregor and T1 slopes were maintained.
Fig. 5.
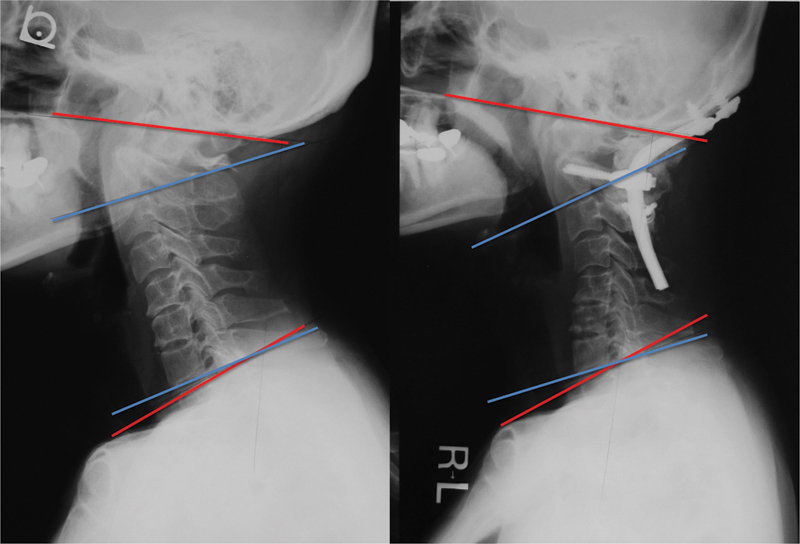
Case 2. A 55-year-old woman with rheumatoid arthritis. Preoperative (left) and 5 years postoperative (right) X-rays. Occipito–C2 lordosis increased after correction surgery, and the subaxial cervical spine presented kyphotic changes 5 years postoperatively. The McGregor slope and T1 slope were maintained.
Fig. 6.
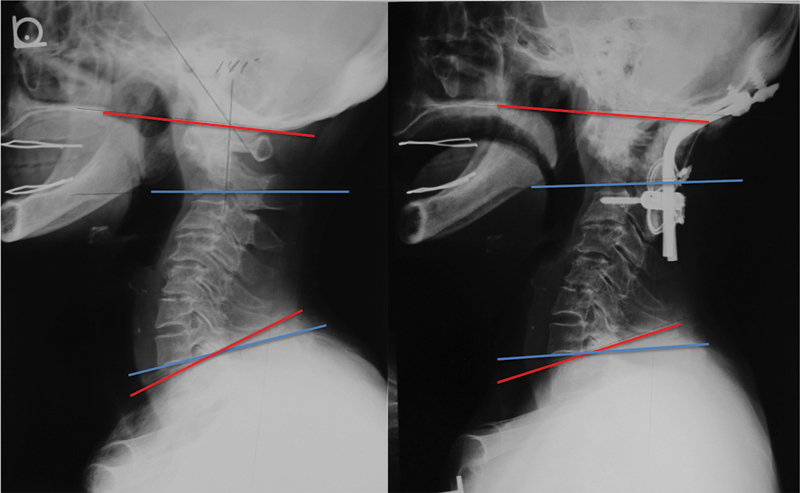
Case 3. A 78-year-old woman with rheumatoid arthritis. Preoperative (left) and 5 years postoperative (right) X-rays. Occipito–C2 angle did not change postoperatively, and none of the sagittal parameters changed 5 years postoperatively.
Fig. 7.
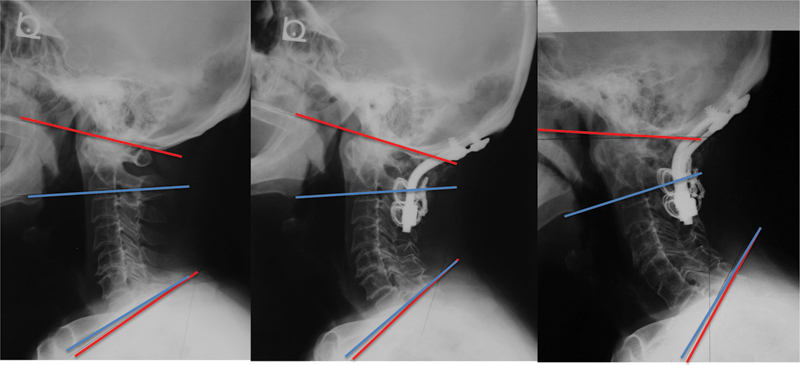
Case 4. A 63-year-old woman with rheumatoid arthritis. Preoperative (left), 6 months postoperative (middle), and 4 years postoperative (right) X-rays. Although the occipito–C2 angle did not change postoperatively, T1 slope increased 6 months postoperatively, probably because of the kyphotic changes of thoracic spine. Compensational lordotic change of the subaxial cervical spine maintained the McGregor slope. Four years postoperatively, the T1 slope increased beyond the limit of cervical compensation, and then the McGregor slope changed.
Finally, the multiple linear regression model for postoperative cervical alignment demonstrated that the postoperative subaxial cervical angle could be predicted from the preoperative O–C7 angle and postoperative O–C2 angle. These findings indicate that we should preoperatively plan the occipitocervical fixation angle, considering not only the preoperative occipitocervical angle but also the whole cervical spine sagittal alignment, including the T1 slope.
There are several limitations in this study. This study included patients with rheumatoid arthritis who generally have a fragile spine, and thus a change of alignment could be influenced by concurrent deformity or progression of the disease. There were relatively few patients with sitting X-ray. Standing X-ray may provide additional information for understanding the influence of thoracolumbar alignment. Further investigations on a healthy population with standing whole spine X-ray should be conducted to provide additional information.
Conclusions
In the present study, we demonstrated that correlation between the T1 slope and the O–C7 angle is stronger than that with the C2–C7 angle both pre- and postoperatively. Our results suggest that the O–C7 angle is regulated by the T1 slope, and the corresponding O–C7 angle was divided into the O–C2 and C2–C7 angles with inverse correlation to each other and then maintained horizontal gaze (McGregor slope). We should pay close attention to the alignment of the craniocervical junction, as well as the subaxial cervical spine when considering cervical spine treatment.
Footnotes
Disclosures Yoshitaka Matsubayashi, none Takachika Shimizu, Royalties: Robert Reid, Inc. Hirotaka Chikuda, none Katsushi Takeshita, none Yasushi Oshima, none Sakae Tanaka, none
References
- 1.Glassman S D, Bridwell K, Dimar J R, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30(18):2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 2.Jackson R P, McManus A C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19(14):1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 3.Schwab F, Patel A, Ungar B, Farcy J P, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 4.Glassman S D, Berven S, Bridwell K, Horton W, Dimar J R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30(6):682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 5.Takayama K, Nakamura H, Matsuda H. Quality of life in patients treated surgically for scoliosis: longer than sixteen-year follow-up. Spine (Phila Pa 1976) 2009;34(20):2179–2184. doi: 10.1097/BRS.0b013e3181abf684. [DOI] [PubMed] [Google Scholar]
- 6.Ames C P, Blondel B, Scheer J K. et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38(22) 01:S149–S160. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 7.Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2003;28(12):1258–1262. doi: 10.1097/01.BRS.0000065487.82469.D9. [DOI] [PubMed] [Google Scholar]
- 8.Tang J A Scheer J K Smith J S et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery Neurosurgery 2012713662–669., discussion 669 [DOI] [PubMed] [Google Scholar]
- 9.Lee S H, Kim K T, Seo E M, Suk K S, Kwack Y H, Son E S. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25(2):E41–E47. doi: 10.1097/BSD.0b013e3182396301. [DOI] [PubMed] [Google Scholar]
- 10.Nojiri K Matsumoto M Chiba K et al. Relationship between alignment of upper and lower cervical spine in asymptomatic individuals J Neurosurg 200399(1, Suppl):80–83. [DOI] [PubMed] [Google Scholar]
- 11.Ishii K, Matsumoto M, Takahashi Y. et al. Risk factors for development of subaxial subluxations following atlantoaxial arthrodesis for atlantoaxial subluxations in rheumatoid arthritis. Spine (Phila Pa 1976) 2010;35(16):1551–1555. doi: 10.1097/BRS.0b013e3181af0d85. [DOI] [PubMed] [Google Scholar]
- 12.Ito H, Neo M, Sakamoto T, Fujibayashi S, Yoshitomi H, Nakamura T. Subaxial subluxation after atlantoaxial transarticular screw fixation in rheumatoid patients. Eur Spine J. 2009;18(6):869–876. doi: 10.1007/s00586-009-0945-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoshida G, Kamiya M, Yoshihara H. et al. Subaxial sagittal alignment and adjacent-segment degeneration after atlantoaxial fixation performed using C-1 lateral mass and C-2 pedicle screws or transarticular screws. J Neurosurg Spine. 2010;13(4):443–450. doi: 10.3171/2010.4.SPINE09662. [DOI] [PubMed] [Google Scholar]
- 14.Yoshimoto H, Ito M, Abumi K. et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29(2):175–181. doi: 10.1097/01.BRS.0000107225.97653.CA. [DOI] [PubMed] [Google Scholar]
- 15.Matsunaga S, Onishi T, Sakou T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976) 2001;26(2):161–165. doi: 10.1097/00007632-200101150-00010. [DOI] [PubMed] [Google Scholar]
- 16.Passias P G, Wang S, Kozanek M, Wang S, Wang C. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoaxial dislocations. J Spinal Disord Tech. 2013;26(1):15–21. doi: 10.1097/BSD.0b013e31823097f9. [DOI] [PubMed] [Google Scholar]
- 17.Ha Y, Schwab F, Lafage V. et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J. 2014;23(3):552–559. doi: 10.1007/s00586-013-2953-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knott P T, Mardjetko S M, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10(11):994–998. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 19.Smith J S, Shaffrey C I, Lafage V. et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 2012;17(4):300–307. doi: 10.3171/2012.6.SPINE1250. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu T, Oyama M, Fueki K. et al. Correction surgeries for irreducible kyphotic deformities at craniovertebral junction (in Japanese) Orthop Surg. 2013;64:939–945. [Google Scholar]
- 21.McGreger M. The significance of certain measurements of the skull in the diagnosis of basilar impression. Br J Radiol. 1948;21(244):171–181. doi: 10.1259/0007-1285-21-244-171. [DOI] [PubMed] [Google Scholar]
- 22.Shoda N, Takeshita K, Seichi A. et al. Measurement of occipitocervical angle. Spine (Phila Pa 1976) 2004;29(10):E204–E208. doi: 10.1097/00007632-200405150-00022. [DOI] [PubMed] [Google Scholar]


