Abstract
Objectives
To determine the prevalence of non-violent, gender-based forms of maltreatment of women by husbands and in-laws (i.e., gender-based household maltreatment; GBHM) during pregnancy and postpartum; to clarify the role of GBHM in compromising infant health, and whether this role extends beyond that previously observed for intimate partner violence (IPV).
Methods
Cross-sectional, quantitative data were collected from women (ages 15-35) seeking immunizations for their infants <6 months of age (N=1061) in urban health centers in Mumbai, India. Logistic regression models were constructed to assess associations between maternal abuse (perinatal IPV, in-law violence and GBHM) and recent infant morbidity (diarrhea, respiratory distress, fever, colic and vomiting).
Results
More than one in four women (28.4%) reported IPV during their recent pregnancy and/or during the postpartum period, 2.6% reported perinatal violence from in-laws, and 49.0% reported one or more forms of perinatal GBHM. In adjusted regression models that included all forms of family violence and maltreatment, perinatal GBHM remained significantly associated with infant morbidity (AORs 1.4-1.9); perinatal IPV and in-law violence ceased to predict infant morbidity in models including GBHM.
Conclusions
Findings indicate that non-violent expressions of gender inequity (e.g., nutritional deprivation, deprivation of sleep, blocking access to health care during pregnancy) are more strongly associated with poor infant health than physical or sexual violence from husbands or in-laws in urban India. These results strongly suggest the need to expand the conception of gender inequities beyond IPV to include non-violent forms of gendered mistreatment in considering their impact on infant health.
Keywords: Family violence, in-laws, gender, pregnancy, infant morbidity
Although India has made significant gains in recent years regarding child survival, the under 5 mortality rate remains high at 56 deaths per 1,000 live births,1 far below the Millennium Development Goal of 38 by 2015. Globally, India accounts for 22% of all under 5 years child deaths and 30% of all neonatal deaths. Pneumonia and diarrheal disease remain the leading proximal causes of child mortality.1 However, recently, greater attention has been given to maternal vulnerabilities (e.g., very young maternal age, low education) as threats to infant and child death,2 with consistent evidence found for the association between maternal experiences of intimate partner violence (IPV) and increased risk for multiple major forms of child morbidity.3,4
Studies have documented increased risk of acute respiratory infections and diarrhea among children in Bangladesh3,4 increased risk of malnutrition among children in India, and increased risk of diarrhea, fever, and cough among children in Uganda,5 all based on mothers’ experiences of violence from their male partners. Significant increases in mortality among infants and children under 5 years in India have also been found to be associated with IPV against the child’s mother,6,7 with one study demonstrating that this effect was far greater for female as opposed to male children.8 Given that more than 1 in 5 child deaths globally occur in India,1 that over one third of Indian women report IPV victimization9 and that approximately one in four women in India report such violence during pregnancy,10 it is critical to understand the relationship of IPV to infant and child health and survival in this national context.
Other possible mechanisms thought to be related to both IPV and poor infant health specific to the prenatal period include maternal stress, related reduced immune function,11 and blocked access to prenatal care.11,12 During the post-partum period, inhibiting health-promoting practices such as breastfeeding13,14 and direct violence against an infant have been described as more likely among men who perpetrate IPV.15 What remains less clear is whether IPV is directly responsible for observed associations with perinatal risk factors for poor infant health, or whether IPV is a marker for other forms of chronic, mundane, non-violent maltreatment of women that reflect the pervasive gender inequities present in households affected by IPV.
Gender-based violence and maltreatment of women may also be perpetrated by other family members, with similar implications for infant health. In India and other patrilocal contexts (i.e., those in which women commonly co-reside with their husbands’ family-of-origin), in-laws may be a source of protection for a woman regarding violence and health, or they may be a source of violence and health risk, independent of violence and maltreatment from husbands.15,16 For example, a recent study found that Indian women experiencing IPV during pregnancy or within 6 months postpartum were over five times more likely to report violence from their in-laws during this same period.17
In previous research by the authors of the current study, interviews were conducted with Indian women who had recently given birth and who reported experiencing abuse in their households during the perinatal period, defined as during pregnancy or within 6 months postpartum. These qualitative data were used to generate a compendium of common non-violent forms of abuse from both husbands and in-laws that were reported to co-occur with IPV or in-law violence (ILV) during pregnancy and postpartum; examples included, but were not limited to, limiting nutrition, prohibiting periods of rest, limiting access to medical care for them or their child, and coerced heavy domestic labor, in the context of pregnancy or post-partum.17 These behaviors were labeled gender-based household maltreatment (GBHM). This maltreatment may be more prevalent than physical or sexual violence from household members, and may have direct implications for the health of infants. To clarify the scope of GBHM, its potential role in compromising infant health, and whether this role extends beyond that previously observed for IPV (and hypothesized for in-law violence), the current study assessed the relative prevalence of perinatal GBHM, IPV and ILV, and associations of these forms of abuse with common forms of infant morbidity. The aim of these analyses is to begin to discern whether IPV plays a direct role in affecting infant health, or may be a marker for more normative and prevalent and less stigmatized household patterns of behavior, i.e., GBHM.
Methods
Cross-sectional, quantitative data were collected from women (ages 15-35) seeking immunizations for their infants <6 months of age between August and December 2008. Recruitment and data collection occurred at three large urban health centers (UHCs) in three major slum communities in Mumbai, India. Prior research documents very high rates of infant immunization (97%) in Mumbai slum areas,18 allowing recruitment from a sample likely generalizable to the larger population. The three health centers were selected based on their provision of services to large slum areas, with each serving more than 100,000 residents.
Women were approached subsequent to their receiving immunizations for their children to determine whether they met the following eligibility criteria: a) having an infant ≤ 6 months of age and b) being willing to learn more about a study examining conflict in the family and health issues for women and children. All potential participants were led to a private room within the clinic where informed consent forms were read aloud due to concerns regarding low literacy of participants. Those providing verbal informed consent then completed a quantitative survey with a trained, female research staff member from the Indian National Institute of Research in Reproductive Health (NIRRH) reading all questions aloud and recording the answers provided on a paper survey form. All staff members were trained in research ethics, data collection, and interviewing women experiencing IPV. The survey required between 30-40 minutes to complete and was conducted in Marathi (the native language of Maharashtra) or Hindi, based on participant preference; survey items were developed first in English, then translated to Marathi and Hindi, and then back-translated to English to assure fidelity to original content. Following survey completion, all participants were screened for emotional distress and were given resources for legal, mental health and IPV-related assistance. The Harvard School of Public Health, the University of California at San Diego, and the Indian Council of Medical Research institutional review boards approved all study procedures.
During the recruitment period, a total of 1,830 women were approached for screening. All women presenting to the clinic seeking infant vaccinations were found to be eligible based on their having an infant ≤ 6 months of age. Of these women, 60.5% (1,108 / 1,830) agreed to meet privately with a research team member to learn more about the study; the major reason provided for not agreeing to hear more about the study was lack of time. Of women agreeing to hear about the study, 94.6% (1,049 / 1,108) provided consent and completed the survey. The final N for the current study was 1,061, based on the infant being the unit of analysis and 12 reported sets of twins.
Measures
Demographics of women were assessed via single-item measures and included age, completion of any formal education, current employment status, religion, native state, whether residing with in-laws, and number of children. Husband characteristics assessed via report of participants included age relative to wife’s age, current employment status, and completion of any formal education. Infant characteristics included age in months and whether they were born premature (<32 weeks), were ever breastfed, or were a twin.
Intimate Partner and In-Law Violence and Gender-based Household Maltreatment
Perinatal IPV, violence from in-laws (ILV) and gender-based household maltreatment (GBHM) measures were developed based on findings of the preceding qualitative component of this same study17 and the Indian National Family Health Survey-2.19 All abuse-related items used for the measurement of each of these variables were assessed dichotomously (i.e., yes/no), and separately for the period during the most recent pregnancy and subsequent to the birth of that infant (a period of 6 months or less for the current sample), i.e., postpartum.
Perinatal IPV was measured via four items for each of the assessed periods (during pregnancy or postpartum): (1) “Did your husband hit, push, kick, beat, or slap you?” (2) “Did your husband try to burn you?” (3) “Did your husband insist on sex when you did not want to have sex?” 4) “Did your husband use force to make you have sex when you did not want to have sex?” If they said yes to any of these four items for either of the two periods, they were defined as having experienced perinatal IPV. Cronbach’s alpha for this 8-item measure was .75.
Perinatal violence from in-laws (ILV) was measured via two items for each of the two assessed perinatal periods: (1) “Did your in-laws hit, push, kick, beat, or slap you?” (2) “Did your in-laws try to burn you?” If they said yes to either of these items for either period assessed, they were defined as having experienced perinatal ILV. Cronbach’s alpha for this 4-item measure was .85.
Perinatal gender-based household maltreatment (GBHM) was defined as non-violent forms of abuse from husbands or in-laws occurring during the recent pregnancy or postpartum. As discussed above, this measure was created for this study based on formative qualitative research with women who had recently given birth recruited from these same clinics. The ten identified GBHM items were asked separately for husbands and in-laws and, as with the violence measures, for both the pregnancy and postpartum periods (with the exception of one item, as noted below). These items included “Did your (husband/in-laws) force you to bring money or other things from your parents’ home?”, “Did your (husband/in-laws) interfere in your ability to get health care for yourself?”, “Did your (husband/in-laws) interfere in your ability to get health care for your children?”, “Did your (husband/in-laws) stop you from getting enough food for yourself?”, “Did your (husband/in-laws) stop you from getting enough food for your children?”, “Did your (husband/in-laws) stop you from getting the rest you needed?”, “Did your (husband/in-laws) attempt to stop you from going to your natal home for the birth?” (not assessed for postpartum period), “Did your (husband/in-laws) treat you badly for not having a boy child”, “Did your (husband/in-laws) stop you from taking care of your children?”, “Did your (husband/in-laws) neglect/ignore your baby?”. An additional GBHM item was asked only of husbands for the pregnancy and post-partum periods: “Did you ever feel that you needed help to care for your elder children from your husband but didn’t receive it?” There were also two GBHM items not specific to husbands or in-laws that assessed burden of household labor during pregnancy or post-partum: “Did anyone assist you to prepare meals for the household?”, “Did anyone assist you to perform cleaning work for the household?” Participants responding “yes” to one or more of the husband/in-law items or “no” to either of the household work items, either during pregnancy or post-partum, were coded as having experienced perinatal partner or in-law GBHM. (NOTE: To test for collinearity, correlations were assessed among the main predictor variables (IPV, ILC, partner GBHM and in-law GBHM; the correlation between husband and in-law GBHM exceeded r=.70 and, for this reason, husband and in-law GBHM were considered as a single variable in all subsequent analyses.) The final 44-item measure had a Cronbach alpha of .88.)
Infant Health Outcomes
To assess infant health, women self-reported whether or not their infant had suffered from diarrhea, respiratory distress (a chronic cough), fever, or vomiting in the past two weeks; measures were taken from the core Demographic and Health Survey indicators used for identification of forms of recent major infant morbidity.20 Based on infant health concerns discussed by women during the formative, qualitative phase of this study, an indicator of colic was also included. Colic is defined as crying for more than three hours per day, for more than three days per week, for more than three weeks;21,22 to conform to the format used for other infant morbidity assessments in the current study, women were asked whether their infant was continually crying during the past two weeks.
Data Analysis
Descriptive statistics were generated for all variables, for both the total sample and by each infant health outcome - diarrhea, respiratory distress, fever, vomiting and colic during the past two weeks. Logistic regression models were then constructed to assess the associations between abuse variables (perinatal IPV, ILV and GBHM) and each infant health outcome. Adjusted models were constructed with consideration of covariates previously documented as affecting infant health outcomes. These included maternal age, education, religion, household income, husband age relative to wife’s age, husband education, family type (nuclear or jointly residing with in-laws), and parity (number of children); infant characteristics considered for inclusion in adjusted models included infant’s premature birth (<37 weeks gestation), low birth weight (<2500g), ever being breastfed, being a twin, age (months) and sex. Covariates were considered for inclusion in models based on having a bivariate association with the given health outcome at p<0.30. Logistic regression models were then refined using a backwards stepwise selection process with p<0.05 as the inclusion criterion. Abuse variables (IPV, ILV and GBHM), prematurity, ever breastfed and infant age were retained in all adjusted models based on aims of the current study and known major determinants of infant health. All analyses were conducted using SAS software, Version 9.2 (Cary, NC, USA).
Results
Maternal and Infant Demographics and Infant Health Outcomes
Participating mothers of infants ranged in age from 17 to 45 years, with more than half (55.7%) under age 25 years. The most prevalent of the recent infant morbidities assessed were respiratory distress (46.4%), fever (32.3%) and diarrhea (22.1%); vomiting (16.1%) and colic (8.0%) were somewhat less prevalent.
Perinatal IPV, Violence from In-Laws (ILV), and Gender-Based Household Maltreatment (GBHM)
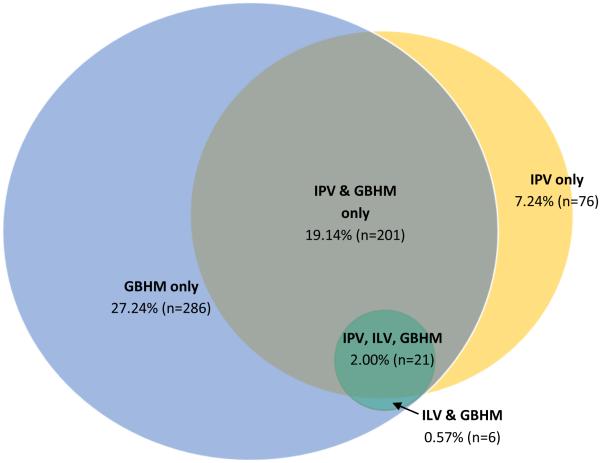
More than one in four women (28.4%) reported IPV during their most recent pregnancy and/or during the current postpartum period (10.9% during pregnancy only, 4.0% post-partum only, 13.5% both during pregnancy and post-partum). A smaller number (2.6%) reported perinatal violence from in-laws (1.2% during pregnancy only, 0.2% post-partum only, 1.1% during pregnancy and post-partum). Approximately one half of women (49.0%) reported one or more forms of perinatal GBHM (7.1% during pregnancy only, 5.1% post-partum only, 36.7% during both pregnancy and post-partum). The most common forms of GBHM were not receiving assistance from family with household work (cleaning and meal preparation), both during pregnancy (29.6% and 32.5%, respectively) and post-partum (33.4% and 35.1%, respectively). Being forced by in-laws to demand money from their natal family during pregnancy (4.7%), husband or in-laws preventing women from getting adequate rest during pregnancy (4.1% and 5.2%) and husband or in-laws preventing women from going to their natal homes during pregnancy (10.6% and 8.3%) were also reported. Slightly less common forms of GBHM reported were in-laws preventing women from getting adequate food during pregnancy (3.0%), abuse from husbands or in-laws post-partum for not having a boy child (3.0% and 3.5%) and interference from husbands or in-laws in women’s ability to seek health care during pregnancy (2.1% and 2.5%). Regarding the co-occurrence of these forms of abuse, ILV almost completely co-occurred with both IPV and GBHM; the majority (74.5%) of cases of IPV also include GBHM. However, the majority (54.5%) of cases of GBHM occurred in absence of either IPV or ILV (see Figure 1).
Figure 1.
Overlap of husband intimate partner violence (IPV), in-law violence (ILV) and gender-based household maltreatment (GBHM) during the perinatal
Associations of Perinatal IPV, ILV and GBHM with Recent Infant Health
In unadjusted analyses, significant associations were seen between perinatal IPV and infant diarrhea (OR=1.50, 95% CI=1.10–2.04), respiratory distress (OR=1.48, 95% CI=1.13–1.93), fever (OR=1.63, 95% CI=1.23–2.15), and vomiting (OR=1.56, 95% CI=1.10–2.21). Perinatal ILV was significantly associated with infant vomiting (OR=2.78, 95% CI=1.23–6.28); a non-significant trend for the association of in-law violence and fever (OR=2.00, 95% CI=0.93–4.29) was also observed. Perinatal GBHM was significantly associated with recent infant respiratory distress (OR=1.47, 95% CI=1.15–1.87), fever (OR=1.75, 95% CI=1.34–2.27), colic (OR=1.98, 95% CI=1.25–3.16), and vomiting (OR=1.72, 95% CI=1.23– 2.40).
In regression models that included all forms of family violence and maltreatment and were adjusted for all indicated covariates, only perinatal GBHM remained significantly associated with assessed forms of infant morbidity; perinatal GBHM was associated with recent infant respiratory distress (AOR=1.38, 95% CI=1.06, 1.81), fever (AOR=1.57, 95% CI=1.18–2.10), colic (AOR=1.88, 95% CI=1.15–3.06), and vomiting (AOR=1.52 95% CI=1.06–2.19).
Discussion
In this first exploration of the prevalence of non-violent forms of gender-based maltreatment of women from family members and the associations of such abuse during the perinatal period with infant morbidity, findings indicate that these mundane expressions of gender inequity (including nutritional deprivation, deprivation of sleep, blocking access to health care during pregnancy) that are more prevalent than IPV are more strongly associated with poor infant health than physical or sexual violence from husbands or in-laws in urban India. These results have important implications for both maternal and child health efforts, and also strongly suggest the need to expand the study of the roles of gender-based inequities in compromising health beyond IPV to include non-violent manifestations of such inequity in the family context.
More than one-quarter of participating women reported IPV during their most recent pregnancy and/or during the current postpartum period, the vast majority of which (24%) occurred during pregnancy. The prevalence of IPV during pregnancy and associations with recent infant morbidity found in the current study are comparable to those found in two recent studies of representative samples of women in India .7,10 Also consistent with earlier studies, IPV during the perinatal period was found to be associated with multiple forms of infant morbidity in unadjusted models.7,10
In this first study of the relationship between in-law violence (ILV) against new mothers and infant health, ILV was found to relate to increased likelihood of recent infant vomiting. Although the low prevalence of this exposure (3%) led to wide confidence intervals, effect sizes suggest that ILV should be further examined for associations with poor maternal and child health among larger samples.
Far more prevalent during the perinatal period than physical or sexual family violence were forms of gender-based household maltreatment from husbands and in-laws (GBHM). Approximately one half of women (49%) reported this form of abuse during the perinatal period, with more than 1 in 3 (37%) reporting GBHM both during pregnancy and postpartum. In this first study of associations between GBHM and infant health, similar to IPV, GBHM was found to be associated with multiple forms of infant morbidity in unadjusted models.
Although correlated, GBHM and IPV were not collinear, with more than half of women reporting GBHM not reporting IPV (Figure 1). Thus, screening for only IPV in maternal or child health settings would miss the majority of women experiencing GBHM. This exclusion would appear to be of consequence for detection of infant morbidity risk; after adjusting for GBHM and other predictors of poor infant health, neither IPV nor ILV was not found to be significantly associated with any of the major forms of morbidity assessed. In contrast, in these same models, GBHM remained a predictor of respiratory distress, fever, colic and vomiting during the past two weeks among this sample of infants less than 6 months of age.
Findings of this research raise important questions regarding whether GBHM is more proximally responsible for the associations previously observed between IPV and poor MCH outcomes; i.e., these more prevalent forms of household maltreatment may relate to mechanisms that lead directly to poor health around the time of pregnancy, with IPV possibly being a marker for such non-violent forms of abuse.
The current findings should be viewed in the context of several limitations. Data were self-reported and recall error or bias may have occurred regarding retrospective reports of perinatal abuse. The study design was cross-sectional, precluding assumptions of causality or directionality. The results of the current study may not generalize to higher-income, non-urban samples or those outside of Maharashtra, India. Finally, this study focuses on a new construct, GBMH, and related assessment. While GBHM is intended to represent non-violent forms of abuse, it is not possible to determine whether or not physical or sexual violence coincided with these incidents of maltreatment. Further research is required involving larger, representative samples across national contexts as well as longitudinal study to clarify the relative roles of IPV, ILV and GBHM in maternal and child health, and whether these behaviors are static across time.
Beyond the limitations of the current study design, the present findings suggest that programs to improve and secure the health and survival of women and children must 1) target these forms of normative gender-based household maltreatment in the context of reproductive and infant health promotion and 2) go beyond education of the individual woman in these same contexts to focus on those who control household norms and roles, as well as access to critical resources such as health care and nutrition – i.e., husbands and in-laws. Specifically, broadening current clinical screening protocols and recommendations regarding IPV to include GBHM should be considered if future studies confirm current findings. Screening for GBMH relative to IPV may be a more effective means of identifying women whose infants are at elevated mortality risk. Because GBHM behaviors are also likely less stigmatized and more normative than IPV across many populations, these forms of abuse may be more acceptable to discuss in the context of households visits with community health workers relative to IPV. Thus, interventions to reduce GBHM as a means of reducing gender inequities and infant mortality may hold promise for integration into existing health structures.
Table 1.
Sample characteristics and prevalence of child health outcomes among infants < 6 mos., Mumbai, Maharashtra, India (N=1,061*)
| (N= 1,061) |
Diarrhea
(22.1%, n=233) |
Respiratory
Distress (46.4%, n=489) |
Fever
(32.3%, n=340) |
Colic
(8.0%, n=84) |
Vomiting
(16.1%, n=170) |
|
|---|---|---|---|---|---|---|
|
| ||||||
| % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | |
| Age | ||||||
| <1 month | 10.3 (109) | 17.4 (19) † | 24.8 (27) † | 17.4 (19) † | 2.8 (3) †† | 10.1 (11) |
| 1 month | 24.3 (257) | 12.8 (33) | 42.4 (109) | 21.9 (56) | 7.8 (20) | 14.8 (38) |
| 2 months | 23.5 (249) | 19.0 (47) | 46.2 (114) | 29.2 (72) | 6.1 (15) | 19.1 (47) |
| 3 months | 18.9 (200) | 28.5 (57) | 50.0 (100) | 37.5 (75) | 9.5 (19) | 18.0 (36) |
| 4 months | 12.8 (135) | 32.8 (44) | 61.2 (82) | 48.5 (65) | 9.7 (13) | 15.7 (21) |
| 5 months | 10.3 (109) | 30.6 (33) | 52.8 (57) | 49.1 (53) | 13.0 (14) | 15.7 (17) |
| Child’s Gender | ||||||
| Female | 50.6 (536) | 22.9 (122) | 42.8 (228) † | 31.9 (170) | 7.9 (42) | 17.1 (91) |
| Male | 49.4 (523) | 21.3 (111) | 50.0 (261) | 32.6 (170) | 8.1 (42) | 15.2 (79) |
| Mother’s Age | ||||||
| 15 - 20 years | 7.6 (81) | 29.6 (24) † | 49.4 (40) | 29.6 (24) †† | 3.8 (3) †† | 17.5 (14) †† |
| 20 - 24 years | 48.1 (510) | 18.9 (96) | 45.2 (229) | 32.4 (164) | 8.7 (44) | 16.8 (85) |
| 25 - 29 years | 29.1 (309) | 25.6 (79) | 45.5 (140) | 29.3 (90) | 6.8 (21) | 13.0 (40) |
| > 30 years | 15.2 (161) | 21.4 (34) | 50.3 (80) | 39.0 (62) | 10.1 (16) | 19.5 (31) |
| Mother Any Formal Education | ||||||
| Yes | 84.3 (894) | 21.1 (188) †† | 46.7 (416) | 30.7 (273) † | 7.9 (70) | 15.9 (141) |
| No | 15.7 (167) | 27.4 (45) | 44.5 (73) | 40.9 (67) | 8.5 (14) | 17.7 (29) |
| Religion | ||||||
| Hindu | 37.7 (400) | 16.1 (64) † | 39.2 (156) † | 24.4 (97) † | 6.8 (27) †† | 11.8 (47) † |
| Muslim | 58.8 (624) | 26.3 (163) | 51.2 (318) | 37.7 (234) | 9.1 (56) | 19.2 (119) |
| Other | 3.5 (37) | 16.7 (6) | 41.7 (15) | 25.0 (9) | 2.8 (1) | 11.1 (4) |
| Household Income (rupees) | ||||||
| <=3,000 | 23.2 (246) | 22.6 (55) | 53.1 (129) †† | 39.9 (97) † | 9.5 (23) | 20.6 (50) †† |
| >3,000 and <=4,500 | 25.1 (266) | 20.7 (55) | 45.5 (121) | 34.3 (91) | 8.0 (21) | 15.2 (40) |
| >4,500 and <=7,000 | 27.1 (287) | 24.8 (71) | 42.7 (122) | 27.3 (78) | 8.4 (24) | 14.0 (40) |
| >7,000 | 24.6 (260) | 20.0 (52) | 45.0 (117) | 28.5 (74) | 6.2 (16) | 15.4 (40 |
| Husband Any Formal Education | ||||||
| Yes | 87.7 (930) | 20.5 (190) † | 45.0 (416) † | 30.9 (286) † | 8.0 (74) | 15.9 (147) |
| No | 12.4 (131) | 33.1 (43) | 56.2 (73) | 41.9 (54) | 7.8 (10) | 17.8 (23) |
| Husband Age Relative to Wife’s | ||||||
| Age | 55.7 (591) | 22.5 (132) | 44.7 (263) †† | 32.4 (190) | 7.2 (42) †† | 15.0 (88) |
| < 5 years older | 41.7 (442) | 21.4 (94) | 47.4 (208) | 32.1 (141) | 9.6 (42) | 17.4 (76) |
| 5-10 years older | 2.6 (28) | 25.0 (7) | 64.3 (18) | 32.1 (9) | 0 (0) | 21.4 (6) |
| > 10 years older | ||||||
| Family Type | ||||||
| Nuclear | 38.7 (410) | 22.9 (93) | 47.8 (194) | 31.8 (129) | 7.4 (30) | 16.0 (65) |
| Joint | 61.3 (650) | 21.6 (140) | 45.5 (295) | 32.6 (211) | 8.4 (54) | 16.2 (105) |
| Number of Other Children | ||||||
| 0 | 40.4 (427) | 22.1 (94) | 47.0 (200) | 31.9 (136) | 7.5 (32) | 14.4 (61) |
| 1 | 32.3 (341) | 20.9 (71) | 45.9 (156) | 31.0 (105) | 7.4 (25) | 17.4 (59) |
| 2-3 | 22.9 (242) | 21.7 (52) | 43.8 (105) | 31.7 (76) | 8.8 (21) | 17.1 (41) |
| >4 | 4.4 (46) | 32.6 (15) | 58.7 (27) | 47.8 (22) | 10.9 (5) | 19.6 (9) |
| Premature Birth | ||||||
| Yes | 13.8 (146) | 21.2 (31) | 56.9 (83) † | 28.8 (42) | 9.0 (13) | 15.2 (22) |
| No | 86.2 (910) | 22.2 (202) | 44.7 (406) | 32.8 (298) | 7.8 (71) | 16.3 (148) |
| Low Birth Weight¶ | ||||||
| Yes | 18.3 (193) | 21.8 (42) | 46.6 (90) | 33.7 (65) | 6.2 (12) | 19.2 (37) |
| No | 81.7 (863) | 22.2 (191) | 46.3 (399) | 31.9 (275) | 8.4 (72) | 15.5 (133) |
| Ever Breastfed | ||||||
| Yes | 99.4 (1046) | 22.0 (230) †† | 46.0 (481) †† | 32.2 (336) | 7.8 (81) †¶ | 15.7 (164) †¶ |
| No | 0.6 (6) | 50.0 (3) | 83.3 (5) | 50.0 (3) | 50.0 (3) | 83.3 (5) |
| Twin | ||||||
| Yes | 2.6 (24) | 8.7 (2) †† | 47.8 (11) | 8.7 (2) † | 17.4 (4) ††¶ | 4.4 (1) ††¶ |
| No | 97.7 (1037) | 22.4 (231) | 46.3 (478) | 32.8 (338) | 7.8 (80) | 16.4 (169) |
All outcomes had fewer than 9 missing responses and each bivariate analysis had fewer than 12 children with a missing response to the outcome or demographic variable
Significant differences between groups observed (p < 0.05) and considered for inclusion in multivariate models.
Considered for inclusion in multivariate models (p < 0.30).
Fisher’s exact test used instead of χ2, due to small cell sizes
122 birth weights were imputed using mean birth weight by prematurity status and none were low birth weight: premature = 2,515g, full term = 2,826g.
Table 2.
Unadjusted associations of perinatal abuse (IPV, ILV, and GBHM) of mothers of infants <6 mos. and infant health (past two weeks), Mumbai, Maharashtra, India (N=1,061)
|
Diarrhea
(n = 233) % OR (95% CI) |
Respiratory Distress
(n = 489) % OR (95% CI) |
Fever
(n = 340) % OR (95% CI) |
Colic
(n = 84) % OR (95% CI) |
Vomiting
(n = 170) % OR (95% CI) |
|
|---|---|---|---|---|---|
| Perinatal IPV | |||||
| Yes | 1.50 (1.10 – 2.04) | 1.48 (1.13 – 1.93) | 1.63 (1.23 – 2.15) | 1.30 (0.81 – 2.09) | 1.56 (1.10 – 2.21) |
| No | REF | REF | REF | REF | REF |
| Perinatal ILV | |||||
| Yes | 1.29 (0.55 – 3.07) | 1.46 (0.68 – 3.14) | 2.00 (0.93 – 4.29) | 2.24 (0.78 – 6.42) | 2.78 (1.23 – 6.28) |
| No | REF | REF | REF | REF | REF |
| Perinatal GBHM | |||||
| Yes | 1.26 (0.94 – 1.69) | 1.47 (1.15 – 1.87) | 1.75 (1.34 – 2.27) | 1.98 (1.25 – 3.16) | 1.72 (1.23 – 2.40) |
| No | REF | REF | REF | REF | REF |
Table 3.
Adjusted associations of perinatal abuse (IPV, ILV and GBHM) of mothers of infants <6 mos. and infant health (past two weeks), Mumbai, Maharashtra, India (N=1,061)
|
Diarrhea
AOR † (95% CI) |
Respiratory Distress
AOR † (95% CI) |
Fever
AOR † (95% CI) |
Colic
AOR † (95% CI) |
Vomiting
AOR † (95% CI) |
|
|---|---|---|---|---|---|
| Perinatal IPV | |||||
| Any | 1.34 (0.95 – 1.90) ‡ | 1.22 (0.91 – 1.65) § | 1.31 (0.96 – 1.80) ǁ | 0.99 (0.59 – 1.64) ¶ | 1.22 (0.83 – 1.80) # |
| None‡ | - | - | - | - | - |
| Perinatal ILV | |||||
| Any | 0.77 (0.30 – 1.98) § | 0.84 (0.37 – 1.89) ǁ | 1.05 (0.47 – 2.35) ¶ | 1.28 (0.42 – 3.92) # | 1.75 (0.73 – 4.21) ** |
| None‡ | - | - | - | - | - |
| Perinatal GBHM | |||||
| Any | 1.11 (0.80 – 1.53) § | 1.38 (1.06 – 1.81) ǁ | 1.57 (1.18 – 2.10) ¶ | 1.88 (1.15 – 3.06) # | 1.52 (1.06 – 2.19) ** |
| None‡ | - | - | - | - | - |
All models include IPV, ILV, GBHM, premature birth, ever breastfed, and infant age
Referent is no IPV/ILV/GBHM
Additional significant covariates: husband’s education, mother’s age, religion (p < 0.05)
Additional significant covariates: religion, gender (p < 0.05)
Additional significant covariates: religion, twin (p < 0.05)
No additional significant covariates (p < 0.05)
Additional significant covariate: religion (p < 0.05)
Acknowledgements
The current study was funded by the US National Institutes of Health and the Indian Council on Medical Research Indo-US Program on Maternal and Child Health and Human Development (R03HD055120-01; Silverman and Balaiah PIs), and the U.S. National Institute on Child Health and Development (R01HD061115-01; Raj PI).
References
- 1.UNICEF . Levels & Trends in Child Mortality. New York, New York: 2013. [Google Scholar]
- 2.Raj A, McDougal L, Rusch ML. Effects of young maternal age and short interpregnancy interval on infant mortality in South Asia. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2014 Jan;124(1):86–87. doi: 10.1016/j.ijgo.2013.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ackerson LK, Subramanian SV. Domestic violence and chronic malnutrition among women and children in India. American journal of epidemiology. 2008 May 15;167(10):1188–1196. doi: 10.1093/aje/kwn049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silverman JG, Decker MR, Gupta J, Kapur N, Raj A, Naved RT. Maternal experiences of intimate partner violence and child morbidity in Bangladesh: evidence from a national Bangladeshi sample. Archives of pediatrics & adolescent medicine. 2009 Aug;163(8):700–705. doi: 10.1001/archpediatrics.2009.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karamagi CA, Tumwine JK, Tylleskar T, Heggenhougen K. Intimate partner violence and infant morbidity: evidence of an association from a population-based study in eastern Uganda in 2003. BMC pediatrics. 2007;7:34. doi: 10.1186/1471-2431-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ackerson LK, Subramanian SV. Intimate partner violence and death among infants and children in India. Pediatrics. 2009 Nov;124(5):e878–889. doi: 10.1542/peds.2009-0524. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed S, Koenig MA, Stephenson R. Effects of domestic violence on perinatal and early-childhood mortality: evidence from north India. American journal of public health. 2006 Aug;96(8):1423–1428. doi: 10.2105/AJPH.2005.066316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverman JG, Decker MR, Cheng DM, et al. Gender-based disparities in infant and child mortality based on maternal exposure to spousal violence: the heavy burden borne by Indian girls. Archives of pediatrics & adolescent medicine. 2011 Jan;165(1):22–27. doi: 10.1001/archpediatrics.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. JAMA : the journal of the American Medical Association. 2008 Aug 13;300(6):703–710. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- 10.Koski AD, Stephenson R, Koenig MR. Physical violence by partner during pregnancy and use of prenatal care in rural India. J Health Popul Nutr. 2011 Jun;29(3):245–254. doi: 10.3329/jhpn.v29i3.7872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chambliss LR. Intimate partner violence and its implication for pregnancy. Clinical obstetrics and gynecology. 2008 Jun;51(2):385–397. doi: 10.1097/GRF.0b013e31816f29ce. [DOI] [PubMed] [Google Scholar]
- 12.Dietz PM, Gazmararian JA, Goodwin MM, Bruce FC, Johnson CH, Rochat RW. Delayed entry into prenatal care: effect of physical violence. Obstetrics and gynecology. 1997 Aug;90(2):221–224. doi: 10.1016/s0029-7844(97)00252-4. [DOI] [PubMed] [Google Scholar]
- 13.Sarkar NN. The impact of intimate partner violence on women's reproductive health and pregnancy outcome. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2008 Apr;28(3):266–271. doi: 10.1080/01443610802042415. [DOI] [PubMed] [Google Scholar]
- 14.Lau Y, Chan KS. Influence of intimate partner violence during pregnancy and early postpartum depressive symptoms on breastfeeding among chinese women in Hong Kong. Journal of midwifery & women's health. 2007 Mar-Apr;52(2):e15–20. doi: 10.1016/j.jmwh.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Chan KL. Children exposed to child maltreatment and intimate partner violence: a study of co-occurrence among Hong Kong Chinese families. Child abuse & neglect. 2011 Jul;35(7):532–542. doi: 10.1016/j.chiabu.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Raj A, Livramento KN, Santana MC, Gupta J, Silverman JG. Victims of intimate partner violence more likely to report abuse from in-laws. Violence against women. 2006 Oct;12(10):936–949. doi: 10.1177/1077801206292935. [DOI] [PubMed] [Google Scholar]
- 17.Raj A, Sabarwal S, Decker MR, et al. Abuse from in-laws during pregnancy and postpartum: qualitative and quantitative findings from low-income mothers of infants in Mumbai, India. Maternal and child health journal. 2011 Aug;15(6):700–712. doi: 10.1007/s10995-010-0651-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma B, Mahajan H, Velhal GD. Immunization coverage: role of sociodemographic variables. Advances in preventive medicine. 2013;2013:607935. doi: 10.1155/2013/607935. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.National Family Health Survey India . NFHS-2. International Institute for Population Science; Mumbai: 2005. [Google Scholar]
- 20.DHS Demographic and Health Surveys. http://www.measuredhs.com/. Accessed August 21, 2012.
- 21.Akhnikh S, Engelberts AC, van Sleuwen BE, L'Hoir MP, Benninga MA. The excessively crying infant: etiology and treatment. Pediatric annals. 2014 Apr;43(4):e69–75. doi: 10.3928/00904481-20140325-07. [DOI] [PubMed] [Google Scholar]
- 22.Garg P. Infantile colic--unfolded. Indian journal of pediatrics. 2004 Oct;71(10):903–906. doi: 10.1007/BF02830833. [DOI] [PubMed] [Google Scholar]