Abstract
Objective
To examine whether racial, gender, and ethnic salary disparities exist in the physician assistant (PA) profession and what factors, if any, are associated with the differentials.
Data Sources/Study Setting
We use a nationally representative survey of 15,105 PAs from the American Academy of Physician Assistants (AAPA).
Study Design
We use bivariate and multivariate statistics to analyze pay differentials from the 2009 AAPA survey.
Principle Findings
Women represent nearly two‐thirds of the profession but receive approximately $18,000 less in primary compensation. The differential reduces to just over $9,500 when the analysis includes a variety of other variables. According to AAPA survey, minority PAs tend to make slightly higher salaries than White PAs nationally, although the differences are not statistically significant once the control variables are included in the analysis.
Conclusions
Despite the rough parity in primary salary, PAs of color are vastly underrepresented in the profession. The salaries of women lag in comparison to their male counterparts.
Keywords: Workforce diversity, physician assistant, health care supply, gender, race and ethnicity
Several researchers have examined salary disparities of physicians, and most report substantial gender differences (Sasser 2005; American Medical Association, 2008; Leigh et al. 2010; Lo Sasso et al. 2011). Physicians are relatively well‐paid professionals. Their long years of academic rigor and residency give them great insight into their respective disciplines. But not all physicians are paid equally (Langwell 1982; Sasser, 2004; O'Neill and O'Neill 2005; Marrast et al. 2014). Like other disciplines throughout U.S. society, women and people of color continue to lag behind (Tolbert Coombs and King 2005; Nunez‐Smith et al. 2007).
Differences among physician assistants (PAs) have been examined less often. In this article we analyze salary disparities between female and male PAs but also those between racial and ethnic PAs. Two recent reports, using different datasets, noted that female PAs make substantially less than their male counterparts. Coplan and others used the 2009 survey of the AAPA to estimate that the gender gap in pay is 17 percent or $14,685 (Coplan, Essary, Virden III, Cawley, & Stoehr, 2012). Seabury, Chandra, and Jena (2013), on the other hand, used the March Current Population Surveys from 2006 to 2010 to estimate the gender pay gap to be substantially higher at 29 percent. They also showed that as the profession morphed from being a predominantly male to predominately female occupation (Lindsay 2005), the salary disparity increased from 7 percent in the late 1980s to 19 percent in the late 1990s and to 29 percent in their most recent data. They were not able to control for medical specialties, and they did not include PAs younger than 35. While both articles incorporated variances in hours worked and annual earnings in their analyses, neither investigated regional differences, age differences, and places of work. Furthermore, previous studies have not reported on the existence of salary inconsistencies among PAs on the basis of race and ethnicity. This is surprising considering the history of discrimination experienced by communities of color in the United States (James 1994; Byrd and Clayton 2000; Smith 2011). In this article we examine differences in the primary salaries of PAs by gender and race and ethnicity as reported by the AAPA.
Methods
Data
We used 2009 data from the American Academy of Physician Assistants. The Academy sent emails from their databank of PAs and subsequently sent follow‐up emails to nonresponders. They also advertised the survey in several media venues.1 The AAPA had information on 72,433 PAs, and 44,629 of those were members of the Academy. Over 19,000 PAs (19,608) or 27 percent of those contacted participated in the survey.
Data from the AAPA indicate that 24.5 percent of female PAs participated in the survey compared to 19.9 percent of male PAs. Because male PAs have significantly higher salaries than female PAs, the lower response rate of the male PAs underestimates the average salary of all PAs.
Those PAs under the age of 45 were slightly more likely than older PAs to respond (24.7 percent compared to 21.3 percent), and PAs working in a specialty were slightly more likely to be responders (28.4 percent compared to 26.4 percent). Nonresponders varied slightly from responders on places of practice and types of practice, but the differences were small and were not statistically significant.
We excluded respondents reporting less than $10,000 annual income (1 percent of the sample), assuming that they were retired or working only a few hours a week, and those that did not report their income (15 percent). Those that did not report their income were slightly more likely to have a PhD (24 percent compared to 20 percent of those with a master's degree), and they were slightly less likely to have bachelor's degree (5 percent less likely). This response bias again underestimates somewhat the overall salary figure of PAs. There was no difference in reporting or nonreporting of income by those with a master's or associates degree.
The primary difference was that those not reporting their income were much more likely to have worked longer; among those not reporting income 43 percent had worked longer than 20 years compared to only 21 percent of those that had worked less than 20 years. Thus, those that did not report their income are likely well paid due to their longevity in the profession, and the remaining data underestimated the average salary in the sample. The remaining sample was further reduced in the multivariate analysis because of missing data on other variables so that the final sample size was 15,102.
Measures
We used total income expected from one's primary employer. This included estimated incentives, but not income from other practices or sources of income. Eighty‐four percent of the PAs in the sample indicated that they worked only one job and 90 percent indicated that they did not receive incentive pay. Bonuses and other income likely fluctuate from year to year. Thus, the most consistent measure of salary is annual salary from the primary employer.
The original dataset included race‐ethnicity categories for non‐Hispanic White, non‐Hispanic Black, Hispanic, Asian, and Other. We grouped age into ten 5‐year intervals and treated the resulting distribution as a continuous variable based on the midpoints of the categories. We also included a squared term for age in the regression models because diagnostics indicated its relationship with salary was nonlinear. The dataset included age at graduation grouped into four categories of less than 25, 25–27, 27–34, and over 34. Likewise the data contained the number of years since graduation (six categories: <3, 4–6, 7–10, 11–15, 16–20, >20). Education included categories for associate's, bachelor's, master's, and doctorate degrees. Medical specialties were combined into six groups: family medicine, surgery, pediatrics, internal medicine, emergency medicine, and “other” specialties.
Hours worked per week, years working in current specialty, and size of city where the respondents practice were also built in as control variables (see Table 1). The number of hours worked consists of time the respondents spent in any paid employment because the data did not have a separate variable for specific hours in one's primary position. A squared term for hours worked is entered in regression models because diagnostics indicated its relationship with salary is nonlinear. We treated “years working,” grouped into seven categories, as a continuous variable. Size of city contained categories for large (over 250,000 people), small (under 250,000), and suburban (non‐metro areas adjacent to large cities).2 Additionally, region was coded using the census categories of West, Mountain, Midwest, Northeast, and South. To explore potential differences between the D.C. metro area and the South, we treated D.C., Maryland, and Virginia as a separate region because it is a high‐income area. We used ordinary least squares regression in the analyses.
Table 1.
Sample Characteristics (N = 15,102)
| Attributes | Frequency | Percentage | Mean | SD | Range |
|---|---|---|---|---|---|
| Dependent variable | |||||
| Annual salary | $88,544 | $28,430 | ($17,500–210,000) | ||
| Main explanatory variables | |||||
| Female | 9,797 | 35.1 | .65 | .48 | (0, 1) |
| Male | 5,305 | 64.9 | |||
| Race | |||||
| White | 13,363 | 88.5 | .89 | .32 | (0, 1) |
| Black | 428 | 2.8 | .03 | .16 | (0, 1) |
| Hispanic | 554 | 3.7 | .04 | .19 | (0, 1) |
| Asian | 593 | 3.9 | .04 | .20 | (0, 1) |
| Other | 164 | 1.1 | .01 | .10 | (0, 1) |
| Mediators | |||||
| Specialty | |||||
| Family medicine | 3,682 | 24.4 | .24 | .43 | (0, 1) |
| Surgery | 2,461 | 22.9 | .26 | .44 | (0, 1) |
| Pediatrics | 611 | 4.1 | .04 | .20 | (0, 1) |
| Internal medicine | 2,598 | 17.2 | .17 | .38 | (0, 1) |
| Emergency medicine | 1,554 | 10.3 | .10 | .30 | (0, 1) |
| Other | 3,196 | 21.2 | .18 | .39 | (0, 1) |
| Hours worked (per week) | 41.23 | 11.07 | (0, 93.5) | ||
| Geographical region | |||||
| West | 1,844 | 12.2 | .12 | .33 | (0, 1) |
| Mountain | 1,426 | 9.4 | .09 | .29 | (0, 1) |
| Midwest | 3,535 | 23.4 | .23 | .42 | (0, 1) |
| Northeast | 3,484 | 23.1 | .23 | .42 | (0, 1) |
| South | 4,053 | 26.8 | .27 | .44 | (0, 1) |
| DC area | 760 | 5.0 | .05 | .22 | (0, 1) |
| Urban/rural area | |||||
| Urban (250K+ residents) | 11,016 | 72.9 | .73 | .44 | (0, 1) |
| Small city (<250K residents) | 1,844 | 12.2 | .12 | .33 | (0, 1) |
| Suburban | 1,318 | 8.7 | .09 | .28 | (0, 1) |
| Rural | 924 | 6.1 | .06 | .24 | (0, 1) |
| Control variables | |||||
| Age (5‐year intervals) | 41.0 | 11.24 | (27, 72) | ||
| Education | |||||
| Associate's | 800 | 5.3 | .05 | .22 | (0, 1) |
| Bachelor's | 8,775 | 58.1 | .58 | .49 | (0, 1) |
| Master's | 3,265 | 21.6 | .22 | .41 | (0, 1) |
| Doctorate | 2,262 | 14.9 | .15 | .36 | (0, 1) |
| Age at graduation | 29.2 | 4.7 | |||
| Less than 25 years old | .16 | .36 | (0, 1) | ||
| 25–27 years old | .30 | .46 | (0, 1) | ||
| 28–33 years old | .30 | .46 | (0, 1) | ||
| 34 years or older | .24 | .43 | (0, 1) | ||
| Years since graduation (<3, 4–6, 7–10, 11–15, 16–20, >20) | 10.22 | 7.27 | (3,23) | ||
| Years practiced in current specialty (<1, 1–3, 4–6, 7–10, 11–15, 16–20, >20) | 3.22 | 1.76 | (1,7) | ||
| Extra pay/fees available | .88 | .33 | (0, 1) | ||
| Incentives available | .30 | .46 | (0, 1) | ||
Source: American Academy of Physician Assistants (AAPA) Census of Physician Assistants (2009).
Results
The AAPA demographic profile of active PAs indicates that while roughly two‐thirds of practicing physicians are male, nearly two‐thirds (65 percent) of PAs are female (Seabury, Chandra, and Jena 2013). The profession is predominantly non‐Hispanic White (88.5 percent); according to the AAPA data, only 2.7 percent of PAs identify as Black or African American,3 3.4 percent as Hispanic, and 3.9 identify as Asian. In other words, Hispanics and African American, though the largest minority groups in the United States, are significantly underrepresented in the PA profession.4
The results portray the PA profession as it is represented in the AAPA data. Most PAs (58.1 percent) have a bachelor's degree and 21.6 percent have master's degrees in addition. Most (72.9 percent) practice in urban areas (populations of 250,000 or more). Roughly one quarter have their primary specialty as either family medicine (24.4 percent) or surgery (22.9 percent). Seventeen percent practice in internal medicine and 10 percent practice in emergency medicine. The number of PAs compared to the population varies across the country. The number of PAs per capita in the South is somewhat lower than the percentage of the population in the region (27 percent compared to 33 percent) and higher in the Northeast (23 percent of PAs compared to 18 percent of the population). The Midwest and West regions have roughly the same proportions of PAs as the population (23 percent of PAs and 22 percent of the population in the Midwest and 22 percent PAs and 23 percent of the population in the West). The average age of PAs in the 2009 sample was 40.8 years, and the mean age when the respondents graduated from PA School was 29.2. Thus, the typical PA has been practicing for about 10 years. Furthermore, the majority of women are in their first 10 years since graduation, whereas the majority of men have been working in the field over 20 years.
Average salary of PAs in 2009 from their primary place of employment (only) was $88,545, and the median was $88,750 (see Figure 1 and Table 1). Figure 1 shows the reported incomes of PA salaries from their primary jobs. The salaries reflect time in the profession, as well as medical specialty, urban and regional location, age, time in the profession, education, hours worked, and unmeasured variables.
Figure 1.
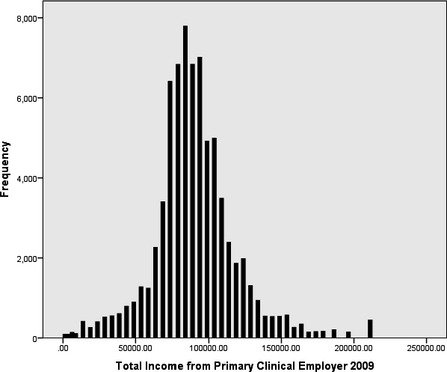
Total Income from Primary Clinical Employer, 2009
Gender, Racial, and Regional Differences in Salary of Physician Assistants
The average salary for male PAs was $99,771 compared to the average salary of female PAs of $82,079. The difference of $17,692 is somewhat less than the $25,226 found by Seabury, Chandra, and Jena (2013).
Interestingly, given the income differences by race in society in general, the PA differences by racial and ethnic groups are not large and not statistically significant in the AAPA data. The highest paid group is composed of those who indicated “other” for their racial/ethnicity category, but the overall difference is not statistically significant. These respondents may be biracial, multiracial, Native Americans, Pacific Islanders, or they may be highly skilled individuals who have immigrated to the United States and identify with different ethnic groups than are usually listed in the United States (e.g., Pakistanis, Indian, or other parts of the world including those who identify with specific Asian groups rather than the more general Asian designation). The racial/ethnic groups with the highest percentage of females (69 percent in the Midwest and Northeast) have the lowest average salaries ($85,314 and $86,036, respectively). Nationally, Hispanic PAs are the second highest paid group of PAs, and non‐Hispanic Whites actually have the lowest average salary reported in the dataset.
As noted, salaries also vary by region. The average salary for PAs is highest in the Pacific states ($94,293) of California, Oregon, Washington, and Alaska where the cost of living is high and lowest in the Midwest ($83,577). Ironically, however, the AAPA data indicate that PAs are not paid particularly well in the Northeast, another area where the cost of living is high. Furthermore, the data reveal that PAs in the South are paid more than any other region of the country except the Pacific region, and the cost of living is generally low in the South. Surprisingly, PAs in the D.C. area, where the cost of living is high, make less than their national counterparts, but the difference is not statistically significant. Primary salary figures by region and race/ethnicity are presented in Table 2.
Table 2.
Average Annual PA Salary in Dollars by Region and Race/Ethnicity
| Pacific | Mountain | Midwest | Northeast | South | D.C. Areaa | |
|---|---|---|---|---|---|---|
| White | 95,037 | 88,096 | 85,677 | 86,252 | 91,414 | 89,100 |
| Black | 95,798 | 96,875b | 90,489 | 85,726 | 88,130 | 81,357 |
| Hispanic | 93,482 | 89,091 | 90,900 | 87,000 | 92,823 | 86,670 |
| Asian | 92,270 | 87,154 | 86,368 | 86,073 | 92,625 | 77,910 |
| Others | 95,928 | 81,792 | 91,416 | 87,316 | 98,815 | 126,522b |
| Not reported | 93,261 | 86,871 | 88,765 | 84,855 | 96,792 | 93,879 |
| Totals | 94,293 | 87,999 | 86,249 | 86,063 | 92,087 | 88,508 |
D.C. Area includes D.C., Maryland, and Virginia.
p < .01 Statistically significantly higher than the average for the region.
Racial and Ethnic Difference of Physician Assistants within Regions
The percentage of PAs of color is low in all areas of the country. The West region has the highest percentage of Hispanic PAs (8.2 percent), but 28.6 percent of the population in the West identify as Hispanic, according to the 2010 U.S. census. The 2010 census further shows the population of the West composed of 76 percent Whites (both Hispanic and non‐Hispanic Whites), 11.1 percent Asian, and 5.7 percent Black. Ten percent of PAs in the West are Asian, and 3.9 percent are Black. The South has similar percentages. Eighty‐seven percent of PAs in the South are White, while the 2010 U.S. census shows that 20 percent of the population is Black, 15.9 percent Hispanic, and 3.3 percent Asian. Even the Midwest, where 11 percent of the population is Black, 3 percent Asian, and 7 percent Hispanic according to the 2010 census, the AAPA survey results show the Midwest to have the highest percentage of White PAs (94.8 percent). The percentage of Asian and Hispanic PAs is highest in the West and lowest in the Midwest. Black PAs are most common in the D.C. area (D.C., Virginia, and Maryland).
Salaries are fairly consistent across ethnic and racial groups within their respective region. With a few exceptions, African Americans and those in the “other” race category in the various regions of the country do as well financially as White, Hispanic, and Asian groups. Two exceptions for African American PAs are those in the South and especially in the D.C. area. In those two areas, African American PAs have somewhat lower salaries than White PAs, but the differences are not statistically significant. African American PAs in the Mountain region have somewhat higher incomes than all other groups; the Mountain West is in an area where African Americans are a very small proportion of the population. Over half of African American PAs in the Mountain region (75/138) practice in Arizona, which likely accounts for the reported higher salaries in the major metropolitan areas there. This figure is based on a relatively small sample of PAs, but the difference is statistically significant compared to all the other PAs within the region (p < .01). The same is true of the highest paid group in the country—the group in the D.C. area that marked “other” as their racial or ethnicity identity. They earn the highest salary in the D.C. area ($126,522), and that figure is significantly higher than the average of PAs in the region ($88,508) and the country as a whole ($89,208). We also note that only 31 individuals were part of the “other” ethnicity category in our sample from the D.C. area. Most other race/ethnic differences in salary are small and not statistically significant. The one exception in salaries for those in the “other” grouping is the Mountain area, where they earn significantly less than their counterparts from other racial and ethnic groups. Comparatively, the data indicate that Hispanic PAs do well financially in most areas of the country.
Minority PAs, compared to White PAs, are far more likely to work in urban areas of 1 million people or more. Sixty percent of African American PAs, 57 percent of Hispanic PAs, and 68.5 percent of Asian PAs work in these major urban areas compared to 41 percent of White PAs. These results are not surprising given the residential patterns of Whites and minorities in the United States (see Mulitalo and Jones 2004). The AAPA data indicate that minority PAs tend to work adjacent to Metro areas but not in them.
Despite having slightly higher salaries, Black PAs in the AAPA sample have slightly less education than other groups; they are slightly more likely to have a BA degree (61 percent compared to all PA average of 55 percent), but are slightly less likely to have a degree beyond the BA (31 percent compared to 40 percent). The number of years worked as a PA does not vary greatly by race or ethnicity, suggesting that the low percentage of Black and Hispanic PAs has been steady for the last 20 years.
Older PAs with more experience and longer tenure have higher incomes than younger PAs, but the difference is not large. The highest incomes are in the 45–49 age grouping. The salaries of older PAs tends to drop slightly but is especially pronounced for those ages 65 and older. Younger PAs (under age 35) have the lowest salaries of the age groups ($80,086) compared to those 45–49 years of age ($94,818).
Multivariate Analysis
The multivariate analysis of primary salaries includes salaries by racial/ethnic group with gender, age, length of time in practice, region, education, type of practice and location of practice (urban/suburban/small city), medical specialty, and hours worked. When these variables are included in the analysis, we examine factors affecting salaries. Young female PAs (under the age of 30) still have a deficit compared to male PAs, but it is smaller ($4,164) compared to the overall sample ($9,536). But mid‐career females between the ages of 30 and 50 have larger deficits (ranging from $9,923 to $12,057) compared to their male counterparts. And female PAs in their fifties have somewhat lower than average deficits—in the range of $8,300 to $8,600. These differences occur even when all the other variables are included in the analysis and are statistically significant at the .05 level or higher (see Table 3).
Table 3.
Ordinary Least Squares Regression Results for PA: Primary Source of Annual Income in Dollars from 2009 AAPA Census (N = 15,102)
| Block 1: Demographic, Education, and Location of Practice | Block 2: First Block Factors Plus Work Specialties and Hours Worked | |||
|---|---|---|---|---|
| Coef | CI | Coef | CI | |
| Demographics | ||||
| Female (implicit is male) | −17,677.05*** | (−18,620.5, −16,733.6) | −9,535.61*** | (−10,372.3, −8,698.9) |
| Age (in 5‐year intervals) | −151.28** | (−238.4, −64.2) | −193.50*** | (−267.7, −119.3) |
| Race (implicit is White) | ||||
| Black | 550.14 | (−2,034.3, 3,134.6) | 327.56 | (−1,869.9, 2,525.0) |
| Hispanic | −447.51 | (−2,737.6, 1,842.6) | 1,927.06 | (−21.0, 3,875.2) |
| Asian | 251.75 | (−1,977.1, 2,480.6) | 300.72 | (−1,594.2, 2,195.6) |
| Other | 2,216.87 | (−1,899.9, 6,333.6) | 249.45 | (−3,248.4, 3,747.3) |
| Education variables | ||||
| Degree obtained (implicit is bachelor's) | ||||
| Associate's | 2,673.71** | (702.4, 4,645.1) | 2,115.00* | (439.6, 3,790.5) |
| Master's | −483.70 | (1,580.1, 612.8) | 1,200.13* | (266.9, 2,133.3) |
| Doctorate | −4,112.06*** | (−5,388.9, −2,835.2) | −3,946.63*** | (−5,038.0, −2,855.2) |
| Age at graduation (<25, 25–27, 28–33, 34+) | 809.85* | (187.6, 1,432.1) | 1,091.82*** | (562.2, 1,621.5) |
| Years since graduation (<3, 4–6, 7–10, 11–15, 16–20, >20) | 1,746.81*** | (1,253.0, 2,240.6) | 1,596.29*** | (1,118.3, 2,074.3) |
| Region/city size of practice | ||||
| Region (implicit is South) | ||||
| West | 2,366.72** | (871.11, 3,862.3) | 4,478.12*** | (3,202.2, 5,754.0) |
| Mountain | −3,366.27*** | (−4,986.3, −1,746.3) | −611.44 | (−1,991.6, 76,838) |
| Midwest | −4,129.31*** | (−5,348.0, −2,910.7) | −4,565.00*** | (−5,602.8, −3,527.2) |
| Northeast | −3,894.44*** | (−5,120.4, −2,668.5) | −4,540.68*** | (−5,589.7, −3,491.7) |
| DC area | −2,147.40* | (−4,220.8, −74.0) | −2,746.5** | (−4,510.2, −982.8) |
| City size (implicit is urban) | ||||
| Small city | −2,242.70** | (−3,580.8, −904.6) | −2,341.10*** | (−3,479.1, −1,203.1) |
| Suburban | −3,760.10*** | (−5,298.0, −222.2) | −1,391.55* | (−2,722.0, −61.2) |
| Rural | −3,885.46*** | (−5,714.2, −2,056.8) | −640.74 | (−2,220.6, 939.1) |
| Work characteristics | ||||
| Primary specialty (implicit is general) | ||||
| Surgery | 13,364.67*** | (12,232.2, 14,497.2) | ||
| Pediatrics | 2,013.33* | (45.2, 14,497.2) | ||
| Internal medicine | 3,680.77*** | (2,492.4, 4,869.1) | ||
| Emergency medicine | 18,917.18*** | (17,531.8, 20,302.5) | ||
| Other specialty | 9,627.13*** | (8,505.8, 10,748.5) | ||
| Years worked in current specialty | 2,496.94*** | (2,165.4, 2,828.447) | ||
| Hours worked per week | ||||
| Under 32 hours | −39,211.47*** | (−40,332.4, −37,912.6) | ||
| 32–38 hours | −5,724.69*** | (−6,858.9, −4,590.4) | ||
| Full‐time | −3,338.45*** | (−4,223.4, −2,453.9) | ||
| Model R 2 | 0.058*** | 0.184*** | ||
Significance values: *p < .05; **p < .01; ***p < .001.
When all the variables are included in the analysis, age is not strongly related to salary earned. Younger PAs tend to make only slightly less than older PAs. The regression results indicate that each decade of age results in older PAs earning only, on average, about $193 more per year. Other factors are more significant than age. Additionally, those with associate's degrees and those with master's degrees make more than those with bachelor's degrees ($2,115 and $1,200 respectively). However, those with doctorate degrees make less than those with bachelor's degrees ($3,947).
Regional differences remain and are statistically significant when all the variables are included in the analysis; the West region remains the highest paid region. This difference reflects the high wage scale generally present in the West. Those in the West make on average $4,478 more than those in the South, which is the next highest region according to the data. The average salaries of those in the Midwest and Northeast lag behind the West by roughly $9,000. Salaries in the Mountain West region are in between the West and the Northeast. PAs in the D.C. area, on average, make $2,747 less than those in the South.
PAs that work in small cities make $2,341 less than those in larger urban areas, and those that work in suburban areas make $1,391 less than the urban areas. Those that work in rural areas earn nearly as much as those in urban areas ($641 less). Minority PAs are more likely to work in urban communities at higher rates than minority physicians (Mulitalo and Jones 2004).
Interestingly, racial and ethnic differences in salary are not statistically significant when all the other variables are included in the analysis. With all the variables included in the analysis, minority PAs do not appear to make significantly more or less than White PAs.
The highest paid specialties are emergency medicine ($18,917 more than those in general PA practice) and surgery ($13,365 more than those in general PA practice) followed by the “other” specialties such as internal medicine and pediatrics. Years worked in current specialty are also an important factor in average salary, as is hours worked (see Table 3).
Limitations
The data have some important limitations. First, the response rate of the AAPA was relatively low. We make our conclusions with the understanding that the PA profession as a whole may differ somewhat from the conclusions presented here. As we noted, the primary difference was that those that had worked longer as PAs were less likely to respond to the surveys, and this likely underestimates the overall salary figures of PAs. Second, we excluded from our analysis those that did not report income, but otherwise completed the survey. This, again, likely underestimates actual salaries earned. Finally, we examined salary figures only for the primary place of employment. Income from other sources is not included. Bonuses and incentives from primary place of income are included, however.
Discussion and Conclusion
Using income from PA primary employer, we provide a more extensive description of the AAPA membership than has previously been published. We have included the distribution of PAs regionally and in urban location since these factors have not previously been studied. We also focus on the salary variations by race and gender. Surprisingly, we find no significant overall differences of minority PAs and White PAs, though we find some regional differences. Salaries of older PAs drop some, probably because they begin to work fewer hours or in different locations than younger PAs, and recent PAs make less than more experienced PAs.
The large salary difference between men and women is the most important finding, a finding that is consistent with previous studies. The large difference between men and women appears to result from several factors: number of hours worked, type of medical specialty, and time in the profession as well as other factors. The difference between the AAPA survey and the Seabury et al. study may be due to sampling variations or the time frame in which the data were collected (the AAPA data is slightly more recent that the data used by Seabury et al.—complied from the years 2006–2010). By comparison the Bureau of Labor Statistics reported in May of 2012 that the average salary for PAs including wages from all sources was 92,460. The somewhat larger average salary observed by the BLS reflects the fact that some PAs work more than one job, thus increasing their overall compensation. Additionally, the results reported here are slightly lower than that reported by Coplan et al. and also included all income from all sources, whereas the results we compiled here are based upon primary income only. At the same time, these explanations do not account for all the differences. Sasser (2005), for example, notes that female physicians make a tradeoff between careers and family by choosing specialties that are compatible with family responsibilities and by working fewer hours than male physicians. The same is likely true for female PAs. We included some of these same factors in our analysis, and they help explain part of the pay differentials. Another factor, not measured in the data, may be that female PAs move in and out of the profession while attending to childbearing/childrearing duties, and these career interruptions may delay their professional development. Likewise, they may use the profession and income as supplementary when husbands are also employed. Still other factors may be that they attend to elderly parents or follow spouses as they move to new locations. These are all traditional roles reserved more to females than males.
At the same time men in traditional female professions, such as the PA profession, may encounter “structural advantages,” which tend to enhance their careers (Lindsay 2005). Males in traditionally female profession tend to go into administrative positions more than women in these professions. We cannot ascertain how much these factors play in the career choice and pay disparities of female PAs.
The comparable salaries of minority PAs are so mewhat unexpected but encouraging, considering the discrimination that minorities experience in the general society. The salary differences by race and ethnicity reflect where they practice, the kinds of practices they have, length of service, and a variety of other factors. Differences by race and ethnicity may exist, but we are unable to ascertain that with this dataset.
We note the low enrollment of African American and other PA students of color in PA schools (Muma and Pries 2010). African Americans represented only 3 percent of the PA graduates from accredited training institutions in 2012 (CASPA/PAEA cycle 12 report 2012). Asians, Latinos, and Native Americans make up 3.9, 3.6, and 0.6 percent of all current practicing PAs, respectively (American Academy of Physician Assistants, 2009). The reasons for this dearth are multifaceted, but not well‐understood or well‐documented.
The reasons for the salary differences by education are not entirely clear. Those with bachelor's degrees may work more than one job while those with an associate's degree tend to work in one location. Those with Ph.D.s likely have their primary employment in the academy teaching and practice on the side. The figures we have examined are for primary place of employment only.
Finally, the higher salaries in rural areas and the South region may reflect a greater reliance on PAs, with an attendant higher salary, because of the lower number of MDs working in those areas. Other research confirms that nonphysicians tend to practice at higher rates in urban and underserved communities compared to physicians (Grumbach et al. 2003). Of note, the data show that PAs in the Midwest are more likely to work in small cities or rural areas while PAs in the South are most likely to work in suburban areas. PAs in the D.C. greater vicinity obviously tend to work in urban settings.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors would like to thank Tasha E. Sabino for her work editing the draft.
Disclosures: None.
Disclaimers: None.
Notes
American Academy of Physician Assistants. 2010. “2010 AAPA Physician Assistant Census National Report” [accessed August 26, 2015]. Available at http://www.aapa.org
Testing the Variance Inflation Factors (VIF) scores of the variables included in the model determined that the model fit the assumptions of noncollinearity. Multiple tests for heteroskedasticity were inconclusive; the tests determined that a robust model yielded very little differences from the original regression though tests suggest that other variables not included in the current dataset would help further specify the model.
We use African American and Black interchangeably throughout this article; we understand, however, that racial and ethnic categories are social constructions with little biological basis. Hispanics can be any race, and biracial people and Hispanic and Asian individuals may choose to list “other” when queried about their “race” or ethnicity.
By comparison the 2010 U.S. census lists 16.3 percent of the population as self‐identified Hispanics or Latinos, and 12.6 percent of the population in 2010 self‐identified as African American or Black in the census. Asian/Pacific Islanders were 3.6 percent of the AAPA sample (compared to 4.8 percent in the 2010 census) and American Indian/Alaskan Natives were 0.6 percent of the AAPA sample (compared to 0.9 percent in the 2010 census). These latter two groups obviously are much closer to their percentages in the population than are African Americans and Hispanics. In the U.S. census 72.4 percent of the population in the 2010 census of the United States identified as non‐Hispanic White.
References
- American Medical Association . 2008. Report 19 of the Board of Trustees (A‐08): Gender Disparities in Physician Income and Advancement [accessed August 24, 2015]. Available at http://www.ama-assn.org/resources/doc/council-on-med-ed/a-08botrpt.pdf. [Google Scholar]
- Byrd, W. M. , and Clayton L. A.. 2000. An American Health Dilemma: A Medical History of African Americans and the Problem of Race, Beginnings to 1900. London: Routledge. [Google Scholar]
- CASPA/PAEA cycle 12 report (Central Application Service for Physician Assistants/Physician Assistant Education Association) (2012). 2012 cycle report.
- Coplan, B. , Essary A. C., Virden T. B. III, Cawley J., and Stoehr J. D.. 2012. “Salary Discrepancies Between Practicing Male and Female Physician Assistants.” Women's Health Issues 22: e83–e89. [DOI] [PubMed] [Google Scholar]
- Grumbach, K. , Gary Hart L., Mertz E., Coffman J., and Palazzo L.. 2003. “Who is Caring for the Underserved? A Comparison of Primary Care Physicians and Nonphysicians in California and Washington.” Annals of Family Medicine 1: 97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, S. 1994. “John Henryism and the Health of African‐American.” Culture, Medicine, and Psychiatry 18: 163–82. [DOI] [PubMed] [Google Scholar]
- Langwell, K. . 1982. “Factors Affecting the Incomes of Men and Women Physicians: Further Explanations.” Journal of Human Resources 17 (2): 261–75. [PubMed] [Google Scholar]
- Leigh, J. P. , Tancredi D., Jerant A., and Kravitz R. L.. 2010. “Physician Wages across Specialties: Informing the Physician Reimbursement Debate.” Archives of Internal Medicine 170: 1728–34. [DOI] [PubMed] [Google Scholar]
- Lindsay, S. 2005. “The Feminizaton of the Physician Assistant Profession.” Women and Health 41 (4): 37–61. [DOI] [PubMed] [Google Scholar]
- Lo Sasso, A. T. , Richards M. R., Chou C.‐F., and Gerber S. E.. 2011. “The $16,819 Pay Gap for Newly Trained Physicians: The Unexplained Trend of Men Earning More Than Women.” Health Affairs (Millwood) 30: 193–201. [DOI] [PubMed] [Google Scholar]
- Marrast, L. M. , Zallman L., Woolhandler S., Bor D. H., and McCormick D.. 2014. “Minority Physicians' Role in the Care of Underserved Patients: Diversifying the Physician Workforce May Be Key in Addressing Health Disparities.” JAMA Internal Medicine 174 (2): 289–91. doi:10.1001/jamainternmed.2013.12756. [DOI] [PubMed] [Google Scholar]
- Mulitalo, K. , and Jones P. E.. 2004. Physician Assistant Practice Patterns: A Review of Texas‐Mexico Border Counties. Presented at the Thirty‐Second Annual Conference of the American Academy of Physician Assistants, Las Vegas, NV. [Google Scholar]
- Muma, R. D. , and Pries P.. 2010. “Evaluation of a Diversity Intervention Funded by Title VII.” Journal of Physician Assistant Education 21: 4–17. [DOI] [PubMed] [Google Scholar]
- Nunez‐Smith, M. , Curry L. A., Bigby J. A., Berg D., Krumholz H. M., and Bradley E. H.. 2007. “Impact of Race on the Professional Lives of Physicians of African Descent.” Annals of Internal Medicine 146: 45–W7. [DOI] [PubMed] [Google Scholar]
- Nunez‐Smith, M. , Pilgrim N., Wynia M., Desai M. M., Jones B. A., Bright C., Krumholz H. M., and Bradley E. H.. 2009. “Race/Ethnicity and Workplace Discrimination: Results of a National Survey of Physicians.” Journal of General Internal Medicine 24: 1198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill, J. E. , and O'Neill D. M.. 2005. What Do Wage Differentials Tell Us about Labor Market Discrimination?. Working Paper No. 11240. Cambridge, MA: National Bureau of Economic Research (NBER). [Google Scholar]
- Sasser, A. C. 2005. “Gender Differences in Physician Pay: Tradeoffs between Career and Family.” Journal of Human Resources 40: 477–504. [Google Scholar]
- Seabury, S. A. , Chandra A., and Jena A. B.. 2013. “Trends in the Earnings of Male and Female Health Care Professionals in the United States, 1987 to 2010.” JAMA Internal Medicine 173: 1748–50. [DOI] [PubMed] [Google Scholar]
- Smith, D. T. . 2011. Fall. “Dirty Hands and Unclean Practice: How Medical Neglect and the Preponderance of Stress Illustrates How Medicine Harms Rather Than Helps.” In D. Smith (Guest Ed.), Journal of Black Masculinity, Health Care Disparities in African Americans Special Edition 2 (1): 11–33. [Google Scholar]
- Tolbert Coombs, A. A. and King R. K.. 2005. “Workplace Discrimination: Experiences of Practicing Physicians.” Journal of the National Medical Association 97: 467–77. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


