Abstract
Stemming the tide of noncommunicable diseases (NCDs) worldwide requires a multi-pronged approach. Although much attention has been paid to disease control measures, there is relatively little consideration of the importance of training the next generation of health-related researchers to play their important role in this global epidemic. The lack of support for early stage investigators in low- and middle-income countries interested in the global NCD field has resulted in inadequate funding opportunities for research, insufficient training in advanced research methodology and data analysis, lack of mentorship in manuscript and grant writing and meager institutional support for developing, submitting and administering research applications and awards. To address this unmet need, the NHLBI-UnitedHealth Collaborating Centers of Excellence initiative created a Training Subcommittee that coordinated and developed an intensive, mentored health-related research experience for a number of early stage investigators from the 11 Centers of Excellence around the world. We describe the challenges faced by early stage investigators in low- and middle-income countries, the organization and scope of the Training Subcommittee, training activities, early outcomes of the early stage investigators (foreign and domestic) and training materials that have been developed by this program that are available to the public. By investing in the careers of individuals in a supportive global NCD network, we demonstrate the impact that an investment in training individuals from low- and middle-income countries can have on the preferred future of or current efforts to combat NCDs.
Introduction: The Importance of Research Training to Combat NCDs
Noncommunicable diseases (NCDs) are the leading causes of death worldwide. The Global Burden of Disease study estimates that NCDs were responsible for the deaths of 38 million people in 2013, a 42% increase compared to 19901. Forty-two percent of NCD deaths occur in people under 70 years of age and of those deaths and 82% are in low- and middle-income countries (LMIC)2. The determinants of NCDs in developing countries span many disciplines including individual- (e.g., sex, education), population- (e.g., urbanization, food systems) and macro-level drivers (e.g., taxation policies, trade agreements)3. While the trans-disciplinary nature of NCDs is increasingly recognized, less attention has been given to training the next generation of trans-disciplinary leaders from LMICs to tackle these problems4.
There is a shortage of LMIC investigators who are willing and able to conduct health-related research within their own countries5,6, yet this capacity is critically important given the contextual nature of determinants of NCDs as well as approaches to their treatment7. For example, while the risk factors for myocardial infarction are common around the globe8, the attributable risk of individual factors differs according to ethnicity and endemic risk factors may also play a role9. Because use of secondary prevention medications is especially low in low-income countries and rural areas, contextualized approaches to improve the long-term use of basic, inexpensive, and effective drugs are required10. Finding effective interventions for behavioral risk factors and sustainable policy requires researchers cognizant and familiar with the issues that inform a country’s policy and practice such as culture, race, ethnicity, and environment. For example, smoke-free policies with strong support in some Latin American and African countries are not popular in others due, in part, to varying levels of interference from tobacco companies11. Without a contextualized research agenda for NCDs, innovation and effective action will be limited.
To tackle the multifaceted issues surrounding NCD control in LMICs, it is crucial to have leaders trained in different disciplines. Historically, academic pursuits in many LMICs have been seen as a luxury and have not been incentivized as a legitimate career pathway12. To build capacity and ensure sustainability, early stage investigators (ESIs) in LMICs must be identified, attracted, trained, mentored, offered opportunities to gain experience, and then incentivized to remain in research as a career. This training extends beyond training people to direct research projects; people must be empowered to facilitate changes within institutions and promote policy changes within countries to reduce the burden of NCDs. Such empowerment must extend beyond intra- and inter-institutional collaboration to include buy-in from local, regional, and national agencies such as the Ministry of Health and sponsors.
Unfortunately, such training programs have been rare4. This article highlights a public-private partnership and how the NHLBI-UnitedHealth Collaborating Centers of Excellence (COEs) (Engelgau MM et al.; Narayan KM, Bloomfield Global Heart 2015 theme issue) built unique research training programs for ESIs from numerous LMICs. In 2009, the NHLBI in partnership with UnitedHealth Group established a network of collaborating COEs based in institutions from LMIC who partnered with research institutions from high-income countries13,14. The eleven COEs are based in ten countries (i.e., Mexico, Guatemala, Peru, Argentina, Tunisia, Kenya, South Africa, India, China and Bangladesh) as described in this issue of the Journal (Engelgau MM et al.; Narayan KM, Bloomfield Global Heart 2015 theme issue). These COEs have the ultimate goal of countering the burden of NCDs in developing nations by enhancing the infrastructure and training necessary to conduct innovative and locally relevant health-related research. Herein, we describe how the training program was set up, the challenges faced, the training approach and selected accomplishments of the training component of the COE program over a 5 year period. While this article focuses on clinical and public health-related research training for ESIs from LMICs and the potential impact of this training on the NCD burden, it is also noteworthy that, to various extents, COEs also engaged in training other cadres of individuals including community health workers, clinicians, administrators and policy makers. We focus on ESI-related training because this level of training was the most common across COEs.
Challenges of NCD Training in LMIC
Training ESIs in LMICs is fraught with numerous challenges. There are few individuals who could serve as research mentors for cardiovascular or pulmonary disease research in the LMIC institutions. Often, it falls to one or a few individuals to take on this responsibility for numerous trainees each year; a situation that is unsustainable and challenging for the small number of individuals. Many institutions lack qualified course developers to address the gaps in the training program. As a result, potential mentors often lack time to devote to training because senior investigators are too busy securing funding for sustainability and capacity building, conducting their own research projects or traveling for academic meetings. Training materials are also in short supply, especially in some native languages. From the trainee perspective, there is often a lack of initiative to invest the time in cultivating a research career because this career pathway is not formalized, publicized, and employment opportunities for such a career are few. Scholarship opportunities to continue studies abroad or locally are few. Lastly, there is the belief that a career focusing primarily on clinical practice is more financially rewarding than a research-focused career.
The COEs needed to enable ESIs to focus on their studies and research when competing activities, some financially rewarding (e.g., locums) were available. The training program needed to be sustainable, with ESIs incentivized to continue in research as a career and avoid human capital flight (i.e., “brain drain”) once the program was over. The COE investigators initially struggled to identify individuals interested in NCD research, while the pool of applicants focused on communicable diseases was plentiful owing to perceptions of disease burden. It was also difficult to identify students with the appropriate backgrounds and qualifications for an NCD training program. Outreach strategies were needed to contact potential ESIs who were “new” to research (i.e., reaching talented individuals who were not part of the existing and established research groups). Identified individuals may have also been skeptical of the prospects of this new program in an emerging field while being asked to leave the security of their current clinical service employment. Implementing their research projects often involved fieldwork that was more time-consuming than anticipated, making it more difficult to focus on training.
Organization and Leadership for Training
While the overall COE program’s goals and accomplishments were broad in scope, a fundamental objective was “to combat non-communicable chronic cardiovascular and pulmonary diseases (CVPD), in developing countries, by enabling clinical research infrastructure development and research training and by conducting research…” that would “facilitate development of country- or region-specific independent chronic cardiovascular and pulmonary disease investigators” as described in the original broad agency announcement (https://www.fbo.gov/?s=opportunity&mode=form&id=e3a267b75087f151e43e3ce3751e3e38&tab=core&_cview=1).
The training goals of the COE program were achieved primarily through resources in the COEs, the Developed Country Partners, the Administrative Coordinating Center and the Training Subcommittee. The Training Subcommittee, formed in 2010, allowed individual COE training directors to learn from each other; share training successes and challenges; strengthen their individual COE training programs; and collaborate on activities that would not only enhance their individual training programs but provide unforgettable and invaluable experiences for their ESIs. The Training Subcommitte included at least one COE-selected representative from each of the 11 COEs as well as representatives from NHLBI and the Administrative Coordinating Center. The Training Subcommittee met in person twice yearly during the COE Steering Committee meetings as well as through periodic conference calls to share best practices and plan future activities. The COE representatives were individuals in leadership positions such as a principal investigator (PI), Co-Investigator, or director of academic affairs. The Training Subcommittee implemented team science methods as researchers with various disciplines and training perspectives shared ideas and collaborated on specific training and capacity-building activities. The Training Subcommittee also compared research training capacity efforts across COEs; discussed ways to evaluate, improve, and expand upon the existing training programs to ensure they met local and regional needs; and developed the agendas and activities for the training aspects of the annual Steering Committee meetings that selected ESIs attended in the fall. The coordinating center staff collected training metrics and materials, providing administrative support that gave NHLBI an opportunity to evaluate the training programs, provide guidance, and offer training opportunities for senior investigators and ESIs.
Training Program Elements
The COE training program offered many health-related research training opportunities to ESIs. Some of these opportunities were the result of a single COE’s effort while others involved collaborating with developed country partners, other COEs or local partners. Both joint training activities across COEs and trainings within each COE were essential aspects of our training portfolio. Many COEs collaborated with local partners in their respective countries to provide training. Such organizations resided within their regions/countries and supported interventions, recruitment and/or training efforts. In some instances, the COE’s program extended beyond their country borders to include neighboring countries. For example, owing to international collaboration and partnerships, the Guatemala-based COE participated in the creation of a regional network of research institutions (Red de Instituciones de Investigación en Enfermedades Crónicas) in nine countries which provided mentorship to locally-based ESIs at each institution. COE researchers were also expected to collaborate with existing local health care systems to foster the sharing of best practices and following research and training guidelines that are consistent with the NHLBI’s ethics and public use dataset policies and procedures. The international nature of the program and training sites yielded benefits for trainees in high-income countries as well, as outlined below.
While training programs within individual COEs were tailored to meet local needs, there were several common elements that were employed throughout the entire program. Additionally, some mid-program training enhancements were made as a result of recommendations from the Training Subcommittee and a mid-program process evaluation. Structured training activities in the COEs included degree and non-degree programs, facilitated mentoring, and in-person activities during the annual Steering Committee meeting in Bethesda, MD and at other conferences.
Academic degree programs
ESIs received educational opportunities through enrollment in degree programs (e.g., master’s, PhD’s, post-graduate) and fellowships, some of which were eligible for scholarships. Areas of interest included clinical effectiveness, epidemiology, epidemiological research, cardiovascular epidemiology, social medicine and health education, public health, international health, and research governance. Some ESIs attended postdoctoral programs at a number of academic institutions including Tulane School of Public Health and Tropical Medicine, Johns Hopkins Bloomberg School of Public Health, the University of Washington, the University of Sydney and on the NIH campus through the Fogarty International Center.
Non-degree credential programs
COE ESIs also received training in human subject protection and good clinical practices from the Collaborative Institutional Training Initiative. Some ESIs attended the Summer Institute epidemiology courses at the Johns Hopkins University Bloomberg School of Public Health. While most of the training was in research or research methods, the Kenya COE also delivered clinical training in cardiovascular medicine, pulmonary medicine, Basic Life Support and Advanced Cardiac Life Support for trainees21.
Mentoring
Mentoring was an integral part of the COE program. Mentor-mentee relationships developed within COEs, across COEs and with developed country partners. While most COEs received some of their mentoring in-person or by phone, all used e-Mentoring, with interactions through email, web conferencing, and the internet. ESIs were often mentored on topics related to research conduct, training, regulatory requirements and ethics, biostatistics, data analysis, data management, program management and grant writing.
Annual Steering Committee meetings
ESI workshops and activities were held concurrently during portions of the annual Fall Steering Committee meetings. Typically, most of the time was spent participating in training activities that ended with a tour of the NIH Bethesda, MD campus. Combining the annual meeting with these activities was a cost-effective way of availing ESIs of training and network opportunities and exposure to the main activities of the Steering Committee. ESIs had the opportunity to interact with investigators during poster sessions and social events. Examples of other training and networking opportunities that occurred during the Steering Committee meetings included:
Case study presentations and discussions. ESIs were organized into teams to discuss 16 COE-submitted case studies with NIH and NHLBI experts providing feedback. The goal of the case studies was to discuss specific methodological difficulties or questions the ESIs were facing in the research studies they were conducting or participating in. For each case there was a group discussion. Trainees were organized in teams to formulate and present approaches to address the issues posed. The experts then provided comments on the trainees’ feedback and final suggestions/clarifications on the issues presented. The majority of the case studies focused on intervention or data collection studies with statistical concerns.
Meet the Expert. ESIs participated in “Meet the Expert” roundtable discussions with epidemiology and training program officers from NHLBI and Global Research Initiative Program for New Foreign Investigators.
Tour of the NIH campus. ESIs had an opportunity to tour the NIH campus where they visited the Clinical Research Center and the National Library of Medicine. This tour provided an opportunity to see the laboratories where NIH scientists conduct their research, the world’s largest biomedical library that promotes access to health communities across the US, and a special exhibit that focused on the Native Americans’ beliefs on health and illness (i.e., “Native Voices: Native People’s Concepts of Health and Illness”).
Workshops. Two grant-writing workshops and one research-management workshop were offered that were instructed by global health experts from academia and government. Results from the 2012 post-workshop evaluation indicated that 97% of the respondents agreed that the topics covered during the workshop would help them write research grants and manage future research endeavors and projects.
Poster sessions. Seed grant awardees presented their research projects, and showcased their projects posters alongside other ESIs and COE PIs.
Conferences, workshops, and other educational opportunities
ESIs had numerous educational opportunities outside degree and credential programs that included conferences, seminars, short courses, workshops, lectures and online trainings in clinical and public health research methods. Biostatistics, epidemiology, data analysis, and scientific writing were common subjects. Several COEs organized journal clubs and held group activities and discussion groups that allowed ESIs to learn from each other as well as senior investigators and professors. Through the COE, ESIs attended the Household Air Pollution Summer Course (Bethesda, Maryland in 2012), the World Hypertension Conference (Istanbul, Turkey in 2013), the 20th International Congress of Nutrition (Granada, Spain in 2013), the Sub-Saharan Africa Grant-Writing and Scientific Peer Review Workshop (Johannesburg, South Africa in 2013), the NIH-Colombia Regional Grant-Writing and Scientific Peer Review Workshop (Bogota, Colombia in 2012), the Summer Institute on Randomized Behavioral Clinical Trials (Warrenton, Virginia in 2013) and the NIH Residency Training component of the Biomedical/Biomedical Research Administration Development Program (Bethesda, MD in 2013) to name some of the most widely attended.
Knowledge to Action: Implementing Skills Gained Through Training
ESIs had numerous opportunities to apply their academic learning through participation in research projects and collaboration with senior investigators. Research shadowing, or mentored research opportunities, made possible by the COE program were essential to link training and implementation of research for ESIs. These opportunities afforded real life experience in data analysis, writing manuscripts, and delivering presentations on the results of their research. To support the next step of implementing their knowledge and acquired skills, the Training Subcommittee proposed that NHLBI announce a Call for Applications for Seed Grant Awards in the fall of 2012. Guidelines were provided, including a requirement for mentoring from a senior investigator, and COE ESIs were invited to submit research proposals on topics within their COE’s Statement of Work. Grant awardees would then go on to conduct the research and present their results to experts and peers via a final report prior to pursuing peer-reviewed publication.
Seed grant applicants were given assistance with their applications from their respective mentors and with a broader range of experts from the COEs and developed country partners at the 2012 Steering Committee meeting in Bethesda. ESIs planning to submit an application were encouraged to draft a specific aims page and present their research ideas to selected members of the Steering Committee and obtain feedback from the faculty.
Twenty-five ESIs submitted Seed Grant proposals. Thirteen seed grants were awarded for a total amount of $242,510. Four quarterly seed grant progress report conference calls were held between March 2013 and January 2014 to assist the seed grant recipients with any challenges they might be experiencing and answer any questions concerning their research and final report requirements. The Seed Grant awards enabled selected ESIs to experience the complete process of successfully submitting a grant application, conducting research, writing the final report, and presenting the research findings and outcomes to their peers. During the 2014 final Steering Committee meeting, an entire day was devoted to ESI seed grant award recipients presenting the results of their research projects and receiving feedback from experts, mentors, and peers. Moreover, a number of publications have resulted from the Seed Grant program including in this issue of the Journal (Zavala et al.; Poggio et al.; Quispe et al.; Maatoug et al.; Carrillo-Larco et al. Global Heart 2015 theme issue).
Training Program Accomplishments
Over the five-year duration, the COE program had numerous successes in training the next cadre of chronic cardiovascular and pulmonary disease investigators from LMICs. The nine COEs funded by the NHLBI trained 563 ESIs and delivered 57 short courses over five years. At the time of this writing, 42 individuals had completed master’s degrees and doctoral programs. Ten ESIs have health research-related degrees pending and four others are completing postdoctoral programs.
ESI accomplishments over this short time period are likewise laudable (Figure 1). ESIs were primary authors on >90 publications (including 9 manuscripts) and participated in 123 presentations (including lectures, poster sessions, and panel discussions) over the COE funding period. Seventy-six ESIs (including 13 Seed Grant Awardees) presented posters on their respective research during the annual steering committee meetings. Research topics included cardiovascular disease risk factors, chronic obstructive pulmonary disease, using technology to manage chronic disease conditions, nutrition, obesity and the effects of indoor air pollution on cardiovascular and respiratory conditions.
Figure 1. Scholarship from early stage investigators from high, and low- and middle-income countries during the COE program.
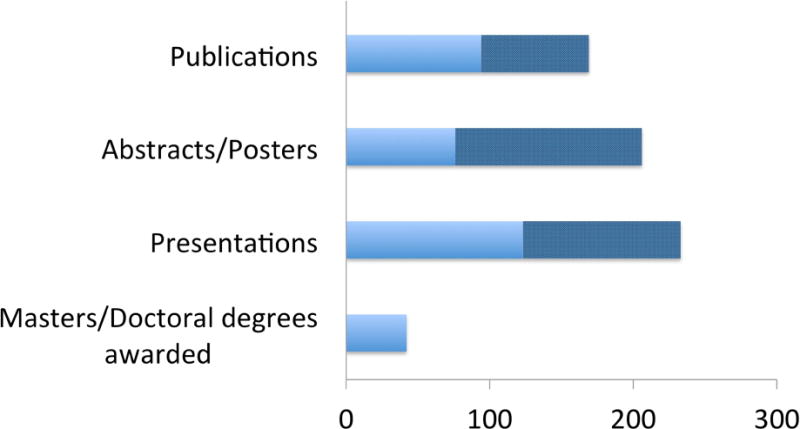
Master’s or higher degrees, presentations, abstracts/posters and publications where an early stage investigator from a low- or middle-income country (solid light blue bars) and high-income country (solid dark blue bars). Values for each bar are presented in the text. For light blue bars: Low- or middle-income countries. For dark blue bars: High-income countries.
Many ESIs from the COE program remain active in research. The program used a Trainee Career Tracking System, comprising the same set of questions used by Fogarty International Center15, to collect data from the ESIs. The criteria for remaining in research included (1) securing research-related employment and/or funding; (2) being appointed to a relevant academic role (e.g., research fellow); or (3) authoring a recent (2011 or later) publication and/or presentation. To date, 236 ESIs have been contacted and 101 responded. The majority (86%) of the responding ESIs remain in research. Typical research-related positions include research director, manager, investigator, officer, scientist, analyst, assistant, biostatistician, and study coordinator. Academic roles included a professor, instructor, or teacher in a health research-related field or with accompanying research funding, publications or presentations.
Impact of the COE Training Program on High-Income Country-based ESIs
The COE program is the quintessential example of an NCD program built on partnerships between high-income country and LMIC institutions. Such partnerships, while designed to benefit LMICs primarily, often benefit high-income countries as well. It was a requirement of the COE program for applicant institutions to be participants in the Fogarty International Clinical Research Scholars and Fellows15, which similarly fosters bi-directional benefits between high-income and LMIC institutions. Through these partnerships, high-income countries often learn about rural health service delivery; skills substitution; creative problem-solving; innovation in mHealth; health financing; and social entrepreneurship16. High-income countries discover potential new ways to address personnel shortages such as task shifting, community-based interventions, increased use of para-professionals, increased community involvement, and using mobile technology to deliver health information16,17.
In the COE program, high-income country institutions also benefited with respect to training and education. Indeed, capacity building and training ESIs in high, middle and low-income country settings is required to create an international NCD network. We polled all principal investigators and developed country partners from the 11 COEs and generated a list of ESIs from high-income country-based institutions that have worked substantively with the COEs since 2009. We then collected information directly from the trainees (n=61) to catalog the extent to which collaboration with the COEs influenced their career development and interests. Among the respondents (n=34), 18 were medical residents/fellows/post-doctoral graduates and 14 were junior faculty from 17 high-income country-based institutions who collaborated with nine of the COEs. High-income country-based ESIs in the COE network published over 75 manuscripts, presented over 130 abstracts/posters and delivered >100 presentations related to research in the COE network. For 14 individuals, their first appointment or promotion was related to their global health career interests, which were fostered by involvement in the COE program. These ESIs have submitted >35 grant applications, been awarded 3 career development awards and have, in turn, mentored more than 70 trainees. Beyond the scholarly activities, clinician investigators and trainees working abroad can also develop clinical skills and become more culturally competent18. Select US universities are also recognizing the importance of global health thus potentially attracting stronger applicants19,20. Thanks to the collaboration with the COEs in LMIC, these universities have access to field programs that provide proper training grounds for students and faculty interested in global health. The implications for the definitions of academic success for US-based ESIs in global health research have also been described18.
Shared Knowledge, Available Widely
One of the great successes of the COE training activities is the reach of these activities beyond the borders of the COEs themselves. Table 1 provides detailed information on the content that was developed by subject matter experts for the COEs. In addition, NHLBI coordinated with coordinating center staff to develop a repository of training materials that would be made available globally on the NHLBI public web site at the end of the COE Program. The COEs collectively submitted >300 training products in 15 topic domains such as economics, biostatistics, research management, research methods, data analysis, and how to write scientific papers. Institutions could customize these training materials to meet their local and regional needs with minimal cost as compared to developing these materials from the beginning. NHLBI is currently developing a web page on their public web site where a list of the COE Training Materials and several samples will be available. This repository will provide a rich database of tools to other LMICs who are interested in building capacity in their institutions that could not be otherwise be built as a single institution. Owing to the prominence of the COE program in the NCD arena, we attracted many subject matter experts who developed content specifically for this program. Topics included health economics concepts for health researchers and a verbal autopsy toolkit. Table 2 provides current information on the repository of training materials created by the individual COEs which, in addition to materials being catalogued, will be publicly available.
Table 1.
Mentoring, training and courses across 15 topics developed by the COE training program
| COE | DCP | Career | Management | Requirements | Economics | Ethics | Epidemiology | Biostatistics | Data Analysis | Building | Scientific Writing | Management | Grantsmanship | Applications | Verbal Autopsy | Diabetes | Prevention, Health |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| China International Center for Chronic Disease Prevention (CICCDP), China | Duke University | M | M, T |
M, T |
M, M, T |
M | M, T |
M | M | M, T |
M | M, T |
M, T, C |
||||
|
|
|||||||||||||||||
| The George Institute, Sydney | M, T |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
||||
|
|
|||||||||||||||||
| Imperial College London | M | M | M | M | |||||||||||||
|
|
|||||||||||||||||
| University Of Queensland | M, T |
M, T |
|||||||||||||||
|
|
|||||||||||||||||
| Universityof Sydney | M, T |
M | T | ||||||||||||||
|
| |||||||||||||||||
| Institute of Nutrition of Central America and Panama (INCAP), Guatemala | Johns Hopkins University | M | M | M, T |
M, T |
M, T |
M, T |
||||||||||
|
|
|||||||||||||||||
| Harvard University | T | ||||||||||||||||
|
|
|||||||||||||||||
| University of Michigan | M, T, C |
M, T, C |
M, T, C |
M, T, C |
M, T, C |
T, C |
M | T, C |
M, T, C |
||||||||
|
|
|||||||||||||||||
| RAND Corporation | M | T, C |
T, C |
M | T, C |
T, C |
M | ||||||||||
|
| |||||||||||||||||
| St. John’s Research Institute, India (Bangalore) | Public Health Research Institute | M, T |
M, T |
M | M, T |
M, T |
M | T | M, T |
M | T | ||||||
|
| |||||||||||||||||
| Center for cArdiometaboli c Risk Reduction in South Asia (COE-CARRS), India (New Delhi) | Emory University | M | M | M | M | M | M | M | M | M | M | ||||||
|
| |||||||||||||||||
| Moi University, School of Medicine, Kenya | Brown University | M, T |
M, T |
M, T |
M | M | T | M | |||||||||
|
|
|||||||||||||||||
| Duke University | M | M, T |
T | M, T,(C) |
M, T,(C) |
M | M | ||||||||||
|
| |||||||||||||||||
| CRONICAS Universidad Peruana Cayetano Heredia, Perú | Johns Hopkins University | M | M | M | M | T | M, T |
M, T |
M | M, T |
M | T | |||||
|
| |||||||||||||||||
| University of Cape Town, South Africa CESCAS | Harvard University | M, T |
T | M | T | M, T |
M | ||||||||||
|
|
|||||||||||||||||
| Tulane University | M, T,(C) |
M, T |
C | M, T,(C) |
M, T,(C) |
M, T,(C) |
M | M | |||||||||
|
|
|||||||||||||||||
| Total | 15 | 11 | 17 | 7 | 19 | 20 | 24 | 21 | 6 | 21 | 9 | 14 | 15 | 2 | 3 | ||
Legend: Over the 5-year COE program there were 12 activities and content produced for Research as a Career, 9 for Research Management, 17 for Regulatory Requirements, 7 for Economics, 18 for Ethics, 17 for Epidemiology, 20 for Biostatistics, 18 for Data Analysis, 6 for Clinical Skill Building, 21 for Scientific Writing, 8 for Project Management, 14 for Grantsmanship, 15 for Funding Applications, 2 for Verbal Autopsy and 2 in other domains. DCP, developed country partners; M, Mentoring activity; T, Training content developed; C, course developed.
Table 2.
Training material developed for COE trainees that will be widely available for other trainees
| Training Material | Brief description | Subject matter expert(s) |
|---|---|---|
| Health Economics Concepts for Health Researchers | A web-based training (3-modules over 90 minutes) providing an overview of healthcare system economics within LMICs and offers researchers ideas about incorporating that information into their healthcare research studies and proposals so as to better inform healthcare policy and decision-making. The intended audience is primarily healthcare researchers wanting their research to have an increased relevance to their specific country’s economic environment but others interested in the impact of health economics on healthcare research will also benefit from the training. | Dr. Rachel Nugent (University of Washington) Mr. Andrew Mirelman (Johns Hopkins University) |
|
| ||
| Verbal Autopsy Toolkit | An introduction to VA for health researchers and interested members of the public. The toolkit is an introduction to verbal autopsy and consists of four tools:
|
Dr. Rohina Joshi (The George Institute) Dr. Rasika Rampatige (University of Queensland) Dr. Henry Kalter (Johns Hopkins University) |
Challenges and Lessons Learned
There have been many challenges and lessons learned over five years of building research capacity in the COE institutions. Promoting collaboration and team science with great cultural and organizational diversity among the COEs presented many challenges that required network members to communicate openly and honestly, respect each other’s differences, agree on a policy to resolve conflict, develop relationships and prioritize tasks, and create a mutually agreeable decision-making process. From a training standpoint, the NHLBI supported the formation of the Training Subcommittee for the purpose of addressing these challenges and promoting team science. As would be expected with COEs from numerous countries, individual COEs varied in how their programs were structured and capabilities in different areas. For example, while the China and India COEs offered training for post-doctoral fellows, the Peru and Guatemala COEs focused on training Master’s-level students and professors. Such variance posed a challenge to leveraging and distributing this expertise across COEs uniformly. The COE Program needed to be flexible and allow individual COEs to meet the needs of their country with respect to available resources and culture while still meeting NHLBI’s training program objectives.
Network members were cognizant of potential language barriers. Among seven different languages across the COEs, English was a common language, but communication was still challenging for some investigators. Staff strove to minimize the use of acronyms. Procedures were implemented to standardize messages and make it easier for everyone to communicate. Examples of such procedures included creating an email template for communications that noted urgency and date for response; copying additional COE staff on all COE PI communications; and keeping emails short and concise by putting additional information, guidance or procedures in an email attachment.
Geographic distance was a challenge for some training-related programs such as mentoring. We therefore took advantage of the Steering Committee meetings for ESIs to interact with a broad array of investigators and structured specific activities to nurture this interaction. Even with this intervention, however, the network could support a limited number of ESIs to attend Steering Committee meetings. Future efforts to minimize the challenges related to distance should consider funding more ESI attendees as well as taking advantage of the e-Mentoring initiative (http://www.nhlbi.nih.gov/research/training/e-mentoring/) and other training related resources through the NHLBI (http://www.nhlbi.nih.gov/research/training), the NIH Clinical Center’s bioethics courses (http://bioethics.nih.gov/courses/index.shtml) and clinical research training (http://clinicalcenter.nih.gov/training/training/ippcr.html).
Attracting and retaining qualified and interested candidates made it challenging to build capacity within the COEs to offer strong research training programs for ESIs. While the training offered through the COE program addressed these challenges initially, if the investment in training is to have a lasting impact on NCD control it will fall to individual LMIC institutions and governments to retain the human capital that has been developed for NCD research. In addition to research training, endeavors such as the COE training program are likely to be sustained with more investment in institutional research infrastructure and research administration enhancement, faculty research development and training and facilities and resources improvements. The trainee network is also organically supported by mutual interests, geographic proximity mentor connections and social media connections that facilitate continued communication beyond the funding period.
Conclusion
The COE training program applied team science principles by bringing together a group of investigators with diverse disciplines, management styles, local and regional global health needs, core competencies, and training program objectives working towards a common goal. By working together and leveraging on their training expertise, COE training representatives closed gaps in their training programs, provided a unique experience for the NCD-interested ESIs, and collaborated on proposals, securing additional funding from NHLBI to enhance their respective training programs. The quantifiable products of the training components of the COE program (i.e., numbers of trainees, training materials for the public, etc.) have already impacted NCDs locally and regionally. The intangible benefits of enhanced networking, cultural competence and development of a cohort of NCD-minded global health practitioners will undoubtedly continue to be reaped over time.
Acknowledgments
This work was funded with federal funds from the United States National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract Nos. HHSN268200900029C, HHSN268200900032C, HHSN268200900027C, HHSN268200900028C, HHSN268200900025C, HHSN268200900026C, HHSN268200900031C, HHSN268200900033C, HHSN26820090030C. GSB is supported by the FIC of the NIH under award number K01TW008407. RV is supported by the Fogarty International Center (FIC) of the National Institutes of Health (NIH) under Award Number K01 TW 009218 – 05.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.GBD. Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2013:2014. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Fact sheet: Noncommunicable diseases. 2015 http://www.who.int/mediacentre/factsheets/fs355/en/. Accessed July 11, 2015.
- 3.Stuckler D, Siegel K. Sick societies: responding to the global challenge of chronic disease. Oxford: Oxford University Press; 2011. [Google Scholar]
- 4.Siegel KR, Kishore SP, Huffman MD, et al. Trans-Disciplinary Education and Training for NCD Prevention and Control. Glob Heart. 2011;6(4):191–193. doi: 10.1016/j.gheart.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Luepker RV. Careers in cardiovascular disease epidemiology and prevention. Circulation. 2009;120(6):533–538. doi: 10.1161/CIRCULATIONAHA.107.752725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huffman MD, Labarthe DR, Yusuf S. Global cardiovascular research training for implementation science, health systems research, and health policy research. J Am Coll Cardiol. 2015;65(13):1371–1372. doi: 10.1016/j.jacc.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Belue R, Okoror T, Iwelunmor J, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Globalization and health. 2009;5(1):10. doi: 10.1186/1744-8603-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 9.Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112(23):3554–3561. doi: 10.1161/CIRCULATIONAHA.105.563452. [DOI] [PubMed] [Google Scholar]
- 10.Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 11.Sebrie EM, Schoj V, Glantz SA. Smokefree environments in Latin America: on the road to real change? Prev Control. 2008;3(1):21–35. doi: 10.1016/j.precon.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pobee JO. Cardiovascular research: a luxury in tropical Africa? East African medical journal. 1987;64(6):396–410. [PubMed] [Google Scholar]
- 13.Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009;373(9680):2004–2006. doi: 10.1016/S0140-6736(09)61074-6. [DOI] [PubMed] [Google Scholar]
- 14.UnitedHealth Group/National Heart L, Blood Institute Centres of E. A global research network for non-communicable diseases. Lancet. 2014;383(9927):1446–1447. doi: 10.1016/S0140-6736(13)61808-5. [DOI] [PubMed] [Google Scholar]
- 15.Carothers CL, Heimburger DC, Schlachter S, et al. Training programs within global networks: lessons learned in the Fogarty International Clinical Research Scholars and Fellows Program. Am J Trop Med Hyg. 2014;90(1):173–179. doi: 10.4269/ajtmh.12-0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Syed SB, Dadwal V, Rutter P, et al. Developed-developing country partnerships: benefits to developed countries? Global Health. 2012;8:17. doi: 10.1186/1744-8603-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rennert W, Koop E. Primary health care for remote village communities in Honduras: a model for training and support of community health workers. Fam Med. 2009;41(9):646–651. [PubMed] [Google Scholar]
- 18.Jaacks L, Ali MK, Bartlett JD. Global non-communicable disease research: Opportunities and challenges. Ann Intern Med. 2015 doi: 10.7326/M15-1068. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med. 2009;84(3):320–325. doi: 10.1097/ACM.0b013e3181970a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Powell AC, Mueller C, Kingham P, Berman R, Pachter HL, Hopkins MA. International experience, electives, and volunteerism in surgical training: a survey of resident interest. J Am Coll Surg. 2007;205(1):162–168. doi: 10.1016/j.jamcollsurg.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 21.Binanay CA, Akwanalo CO, Aruasa W, Barasa FA, Corey GR, Crowe S, et al. Building Sustainable Capacity for Cardiovascular Care at a Public Hospital in Western Kenya. Journal of the American College of Cardiology. 2015;66(22):2550–2560. doi: 10.1016/j.jacc.2015.09.086. http://doi.org/10.1016/j.jacc.2015.09.086. [DOI] [PMC free article] [PubMed] [Google Scholar]


